A huge leap of evolution in neuroimaging has occurred since the invention of magnetic resonance imaging (MRI). In the past, brain imaging with computed tomography (CT) could demonstrate only macro changes of the pathologic lesions. The development of MRI allows us to ‘visualize’ the brain not only as an organ but also at the cellular and molecular level. The developments of biomolecular nanotechnology may help diagnose underlying pathology related biomarkers, for example amyloid plaque in Alzheimer’s disease (AD), or specific neurotransmitters to demon- strate brain images without the necessity for cranial vault opening.
The anatomical information can be revealed by using CT or conventional MRI (cMRI) which include T1W, FLAIR, T2W, GEW and MR angiography. Most CNS diseases are diagnosed by cMRI, which has higher resolution than CT. MRI also provides quantitative information such as hippocampal volumetric measurements, which can identify early cases of AD or demonstrate subtle atrophy in hippocampal sclerosis. Measurement of T2 sequence values (not visualized as subtle changes of signal intensity) were demonstrated in the hippocampal sclerosis or white matter diseases such as multiple sclerosis (MS). There are still pitfalls to watch out for if we generalize about quantitative information; standard values still need to be known for valid comparisons between patients. However, comparison of patients over different periods of time is a viable follow up treatment response.
Many pulse sequences or techniques in MRI have been proposed for demonstrating pathologic lesions. Appropriate selection of those techniques will give the highest sensitivity and accuracy for the diagnosis. For example, susceptibility weighted imaging (SWI) is very useful in identifying small microbleeds which may indicate the prescence of cerebral amyloid angiopathy. SWI is also beneficial in helping to distinguish tumors from tumifactive demyelination, deep infarction or infection. Abnormal microvascular structures in tumors with angiogenesis are clearly demonstrated by SWI. In other lesions, the transmedullary vein is seen passing through the lesions without destruction. (Figure1).
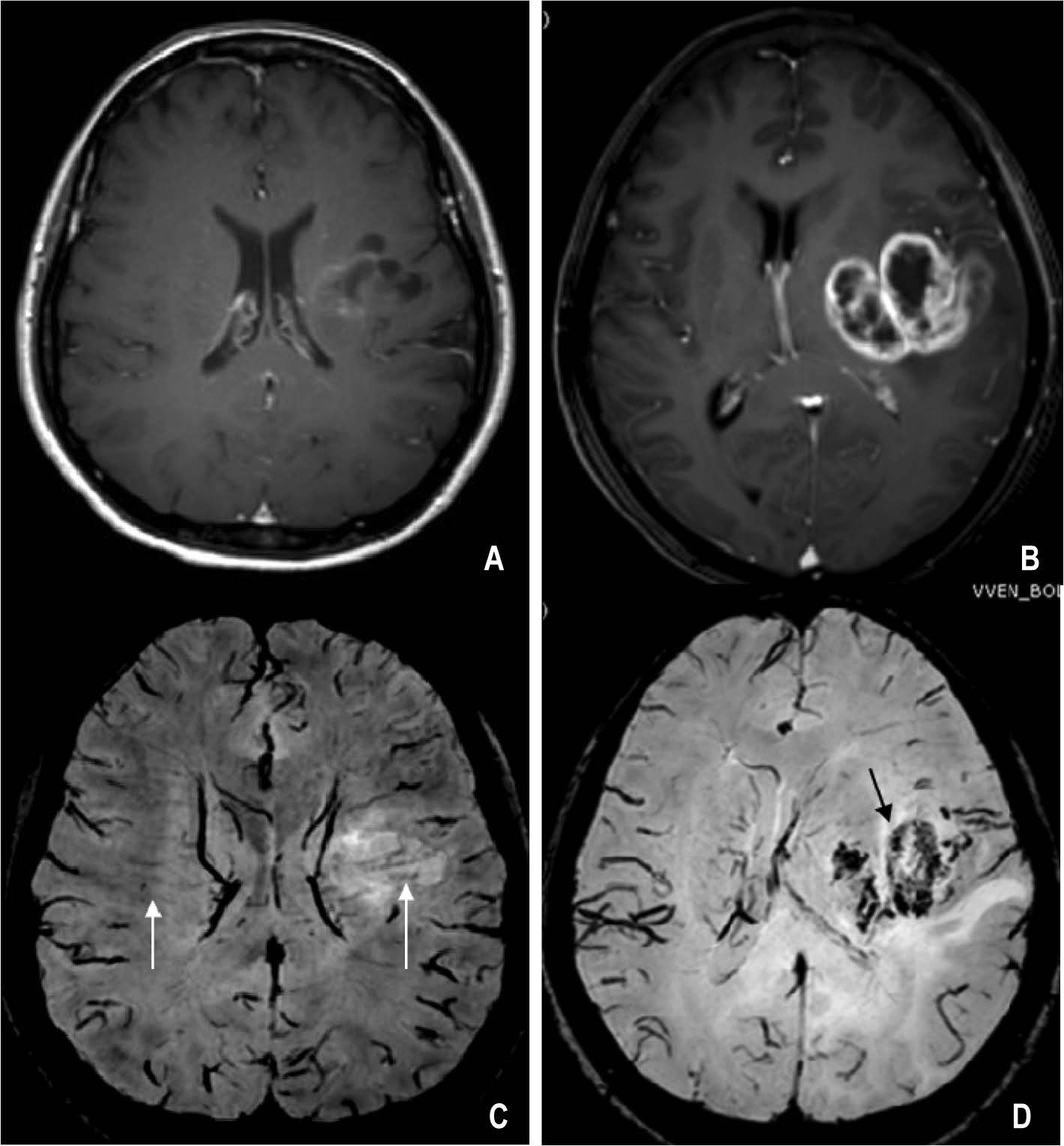
Figure 1: (A, B) Gd-T1 W, (C, D) SWI: comparing between multiple sclerosis (A, C) and glioblastoma multiforme (B, D). There is enhancement at the periphery of both lesions. On SWI, the transmedullary vein is seen passing the MS lesion (arrows in C). In glioblastoma multiforme the normal vein was destroyed and replaced by tumor microvasculature (arrow in D).
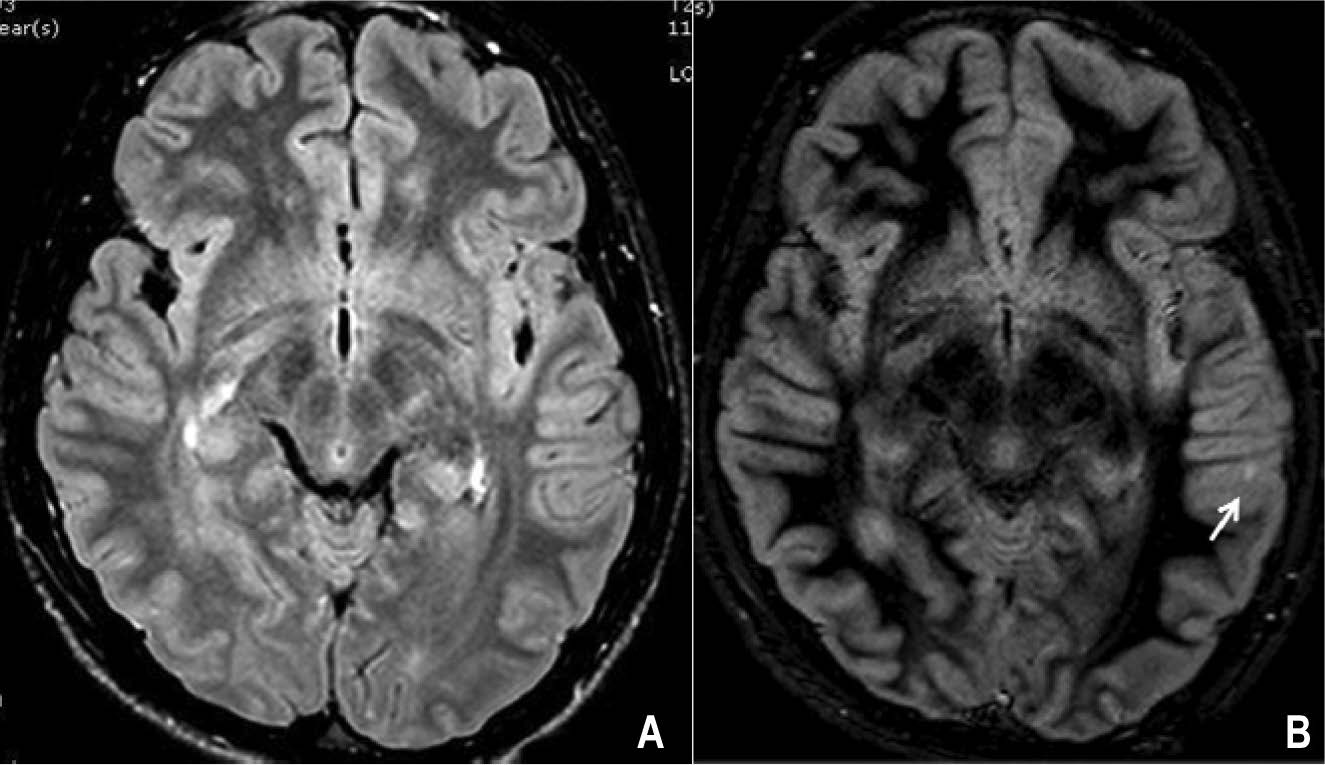
Figure 2: Double inversion recovery (DIR) in multiple sclerosis: (A) FLAIR, (B) DIR show lesion in the gray matter of cerebral cortex on DIR (arrow in B) which is not seen on FLAIR.
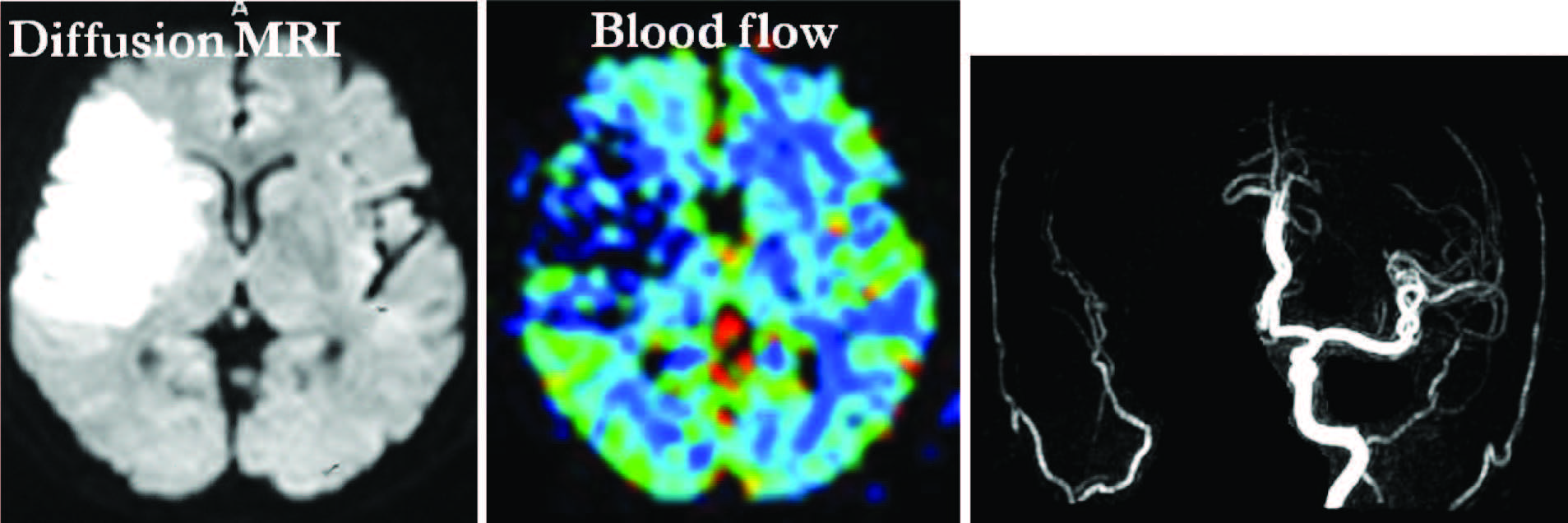
Figure 3: Acute infarction due to occlusion of right internal carotid artery showing lesion on DWI corresponding to perfusion MRI (blood flow) or “diffusion/perfusion match”. It means totally infarct without penumbra of the ischemic area and no advantage to apply thrombolytic agent.
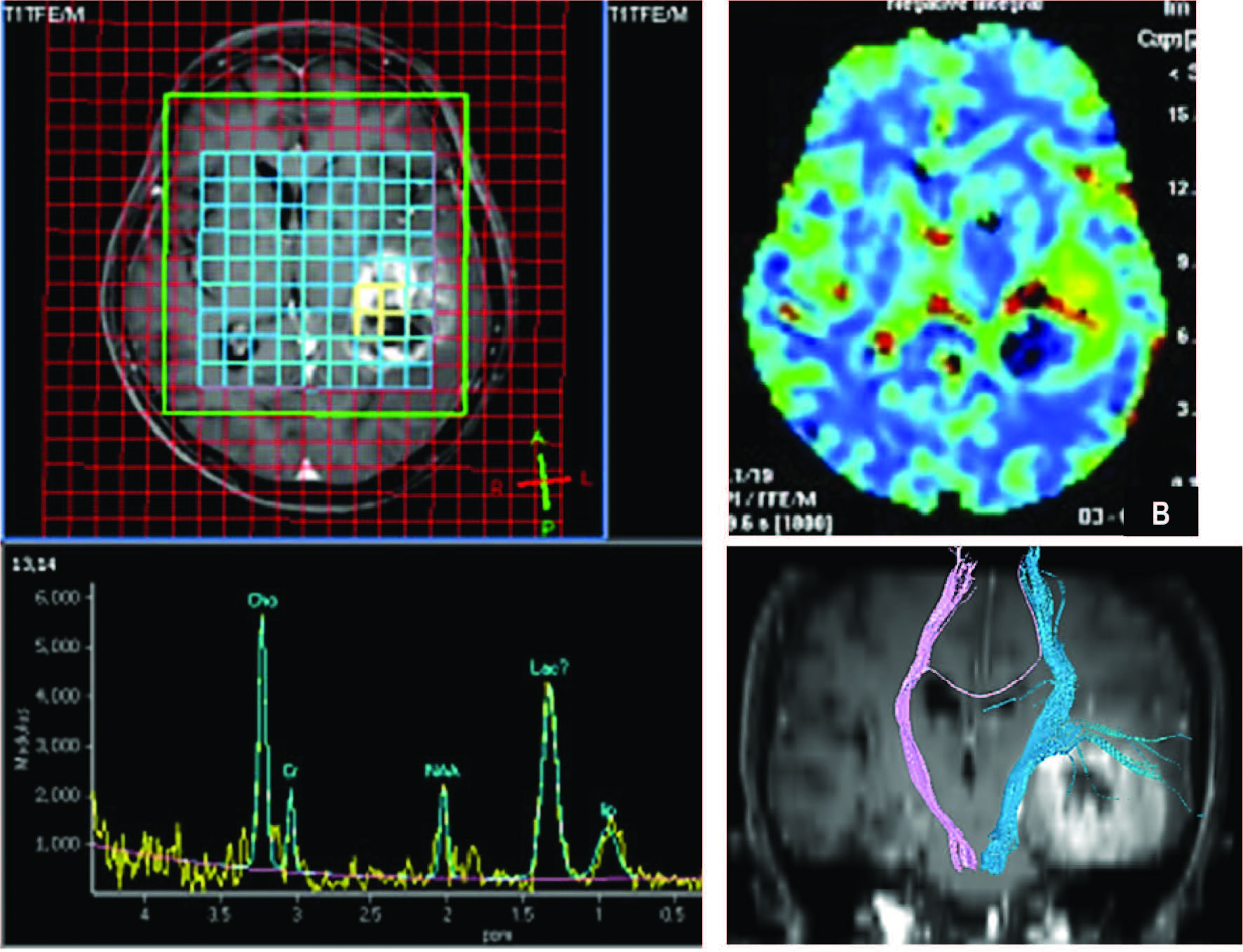
Figure 4: Hight gradeglioma (A) MRS, (B) p MRI (CBV), (C) DTI. MRS shows definitely increased Cho, Lac and Lip peaks in brain tumor. The NAA is markedly decreased. pMRI demonstrates increased blood volume at the periphery (arrow in B) and no blood supply of the central necrosis. DTI shows the relationship between the tumor and the ipsilateral corticospinal tract.
Double inversion recovery (DIR) is an MRI tech- nique demonstrating lesions in gray matter, especially in the cerebral cortex. This technique is useful to identify cortical lesions in MS and support the finding of cortical lesions in pathologic studies (Figure 2). DIR is also useful for demonstrating vascular wall for diagnosis of vascular dissection or identifying vulnerable plaque in atherosclerosis.
Diffusion MRI (D-MRI) is the imaging technique of choice for making immediate decisions about treatment for acute ischemic stroke. The basic principle of D-MRI is detection of water molecule movement in the tissue. Ion-pump dysfunction of ischemic cells causes increased accumulation of water intracellularly, not equilibrate to extracellular space. Restricted diffusion of water mol- ecules is shown as high signal on diffusion weighted imaging (DWI) or low apparent diffusion coefficient on ADC map (Figure 3).
DWI is also useful in brain tumor, MS, epilepsy and oncologic imaging both for demonstrating the pathologic lesions and measuring ADC values. D-MRI is valuable for demonstrating fiber tract in the brain by diffusion tensor imaging (DTI) technique. The technique enables neurosurgeons to plan for brain tumor surgery (Figure 4).
Molecular imaging has been used in neuropsychiatry for a long time. CT, MRI, SPECT and PET enable us to understand the basic functions of brain biology. The protective mechanism of the blood-brain barrier (BBB) and the complexity of networks between the different areas of brain mean it is much more difficult to study brain function, compared to other organs in the body.
Molecular imaging is the technique identifying non- water molecules and their metabolism. It demonstrates brain status before disease develops. SPECT and PET are conventional molecular imaging techniques which have been in use for more than 20 years. Magnetic resonance spectroscopy (MRS) demonstrates various chemical components in the viable tissue by displaying the amplitude of substances of interest in a spectral curve. In a normal brain, N-acetyl aspartate (NAA) is a marker of viable neurons. Choline (Cho) is a marker of cell membrane metabolism which usually has low rates in normal brains. Cho is elevated during the process of cell destruction or proliferation such as occurs in brain tumors. MRS is useful to distinguish between high grade tumors and follow up treatment (Figure 4).
It has been used to differentiate between recurrent tumors and post treatment necrosis. MRS is also able to show abnormalities in AD and hippocample sclerosis which cMRI cannot. Besides MRS, the new technologies using optical imaging have been able to verify progenitor cells in brain parenchyma in many research studies. In amide proton transfer imaging (APT), MRI can detect labile amide protons via the water signal. The detection of polyamide-based images is useful for following up brain tumor and ischemic disease.
In apoptosis (programmed cell death), cell shrinkage and precipitated chromatin differ from necrosis or cell autolysis. The latter processes involve cell edema and disintegration. In normal conditions, the rate of cell proliferation is balanced to apoptosis. If cell proliferation overtakes apoptosis, neoplasm develops. If the converse is true, then degeneration occurs. Annexin A5 was found attaching onto apoptotic cells. Using optical imaging, annexin A5 labeled with illuminated agent was demon- strated to identify myocardial infarct and tumor respon- siveness. The annexin A5 was attached to gadolinium (Gd) or 99mTc to demonstrate tumor responses and atherosclerosis using MRI or SPECT.
Development of pharmaceutical agents for studying cells with MRI may be divided into 2 categories. One detects gene products, for example enzymes which change the chemical structure of the contrast media and leads to changes of relaxation time of the contrast. Another detects changes of transporter proteins on the cell membranes which carry the contrast media into the cytoplasm.The second category is a surrogate method of using functional MRI (fMRI) to detect the altered function of neurons after introducing some drugs such as dopamine transporter, GABAA receptors and opiate receptors.
In terms of molecular size and amount of tracer, PET and SPECT are classified as nano-molecular imaging. Besides the usual radioactive agents: 99mTC, 125I, 123I, 201Tl, 111In and 18F-FDG, there are other specific agents such as 11C-methionine used for detecting brain tumors. 11C-PIB was proved to be useful in identifying Alzheimers and other neurodegenerative diseases. 18F-DOPA was used in studies of Parkinson disease and schizophrenia.
The technology of multidetector CT and related software development have enabled calculation of perfusion of blood into the organ of interest. Computed tomography perfusion (CTP) is a recent imaging modality for studying brain circulation and perfusion.
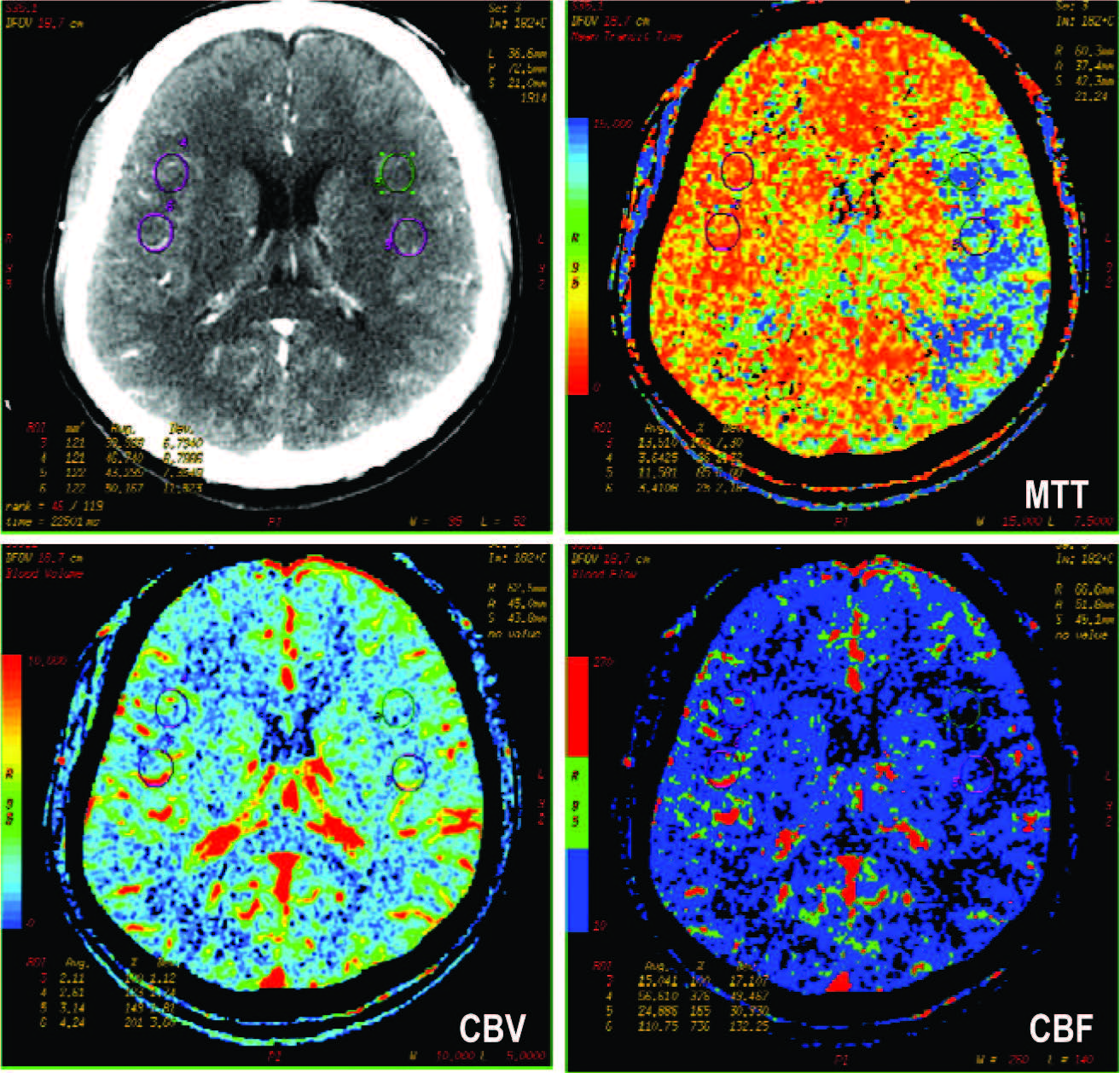
Figure 5: CT perfusion of a patient presented with sudden right sided weakness. There is no detectable abnormality on CECT. The color map of MTT and CBF show the ischemia in left brain (left MCA territory). The CBV does not show definite abnormality.
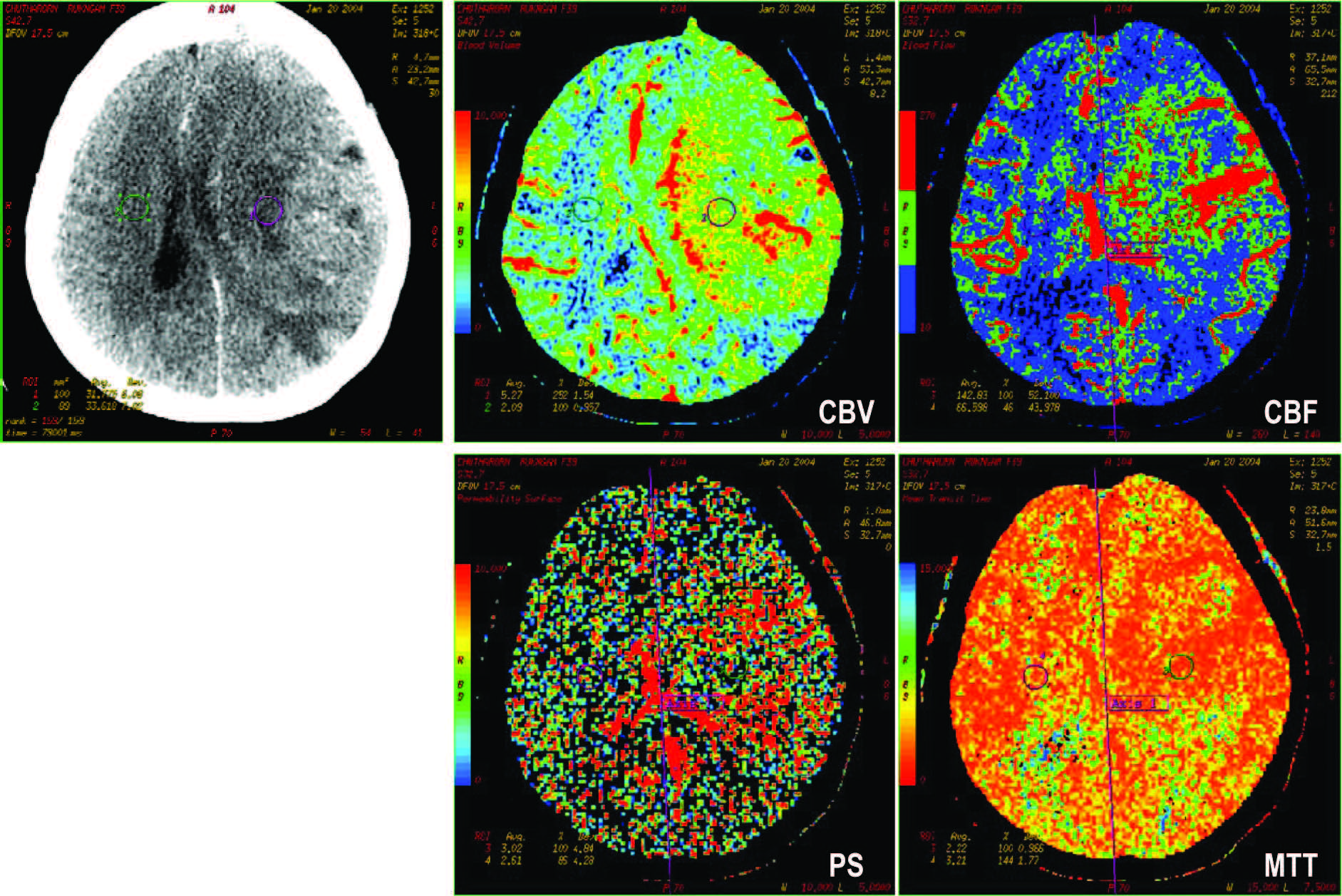
Figure 6: CT perfusion of a patient diagnosed glioblastoma multiforme, status post craniotomy. The surgical
bed of left cerebrum shows definitely increased CBV, CBF. The icreased permeability surface index (PS)
indicates recurrent brain tumor.
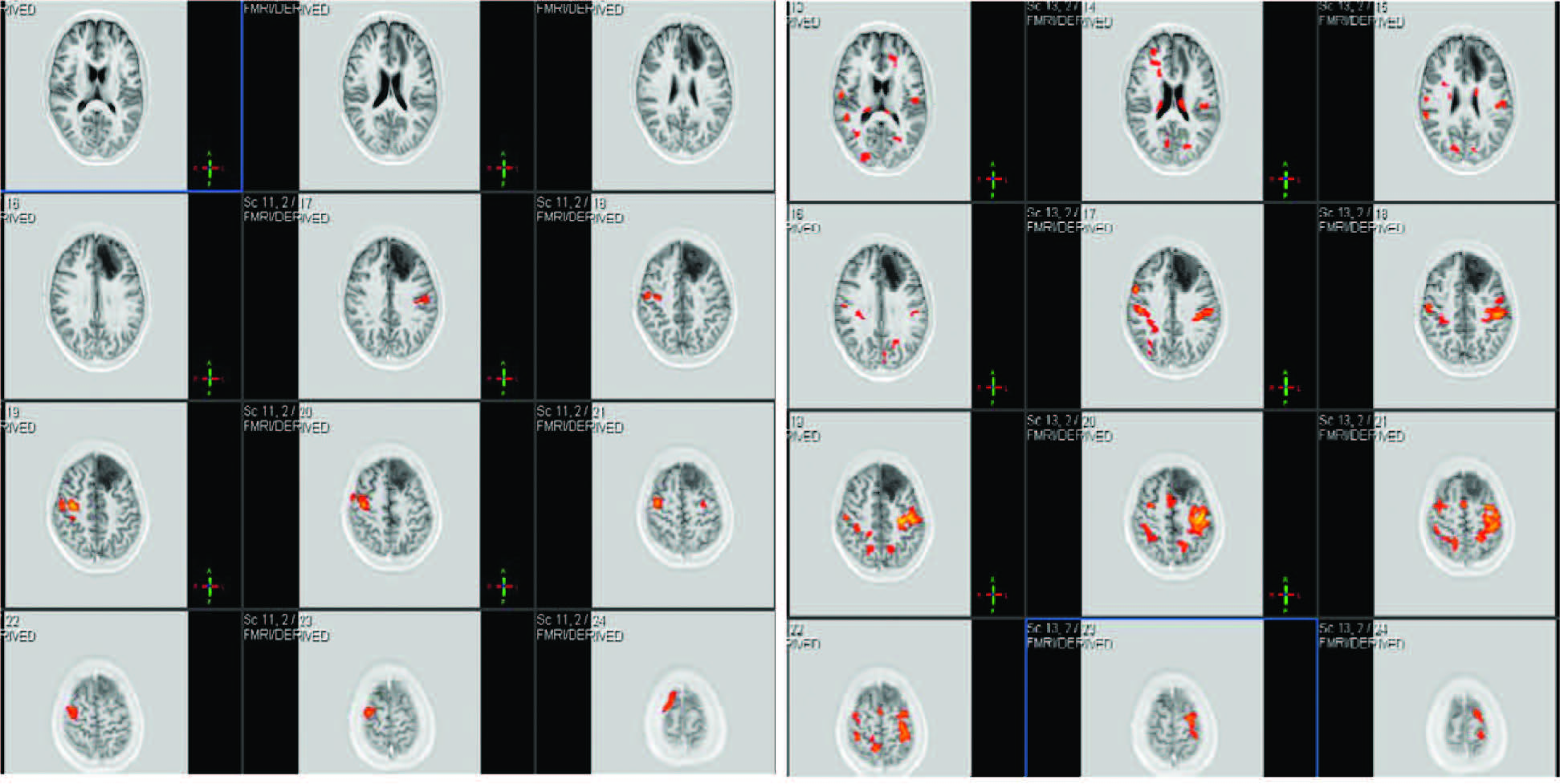
Figure 7: Functional MRI shows areas of stimulated brain during left hand movement (A), and right hand movement (B). There is a brain tumor in the left frontal lobe.
Due to the increased speed of scan, changes of tissue attenuation during injection of contrast media can be detected and calculated into cerebral blood flow, blood volume and mean transit time. Some stroke centers have introduced CTP for acute stroke triage to thrombolytic therapy. It is reported to be able to reduce the number of cases with high risk of hemorrhagic complications and also treat more patients by extending golden time window from 3-4-5 hours to 6-9 hours for transarterial approach and mechanical thrombolectomy. CTP is also useful in determining cerebrovascular reserve in chronic stenosis of the internal carotid artery in order to plan for prophylactic bypass graft, thrombolectomy or stent placement (Figure 5).
CTP has been reported as useful in distinguishing brain tumors from brain abscesses, high grade or metas- tasis from low grade tumor, and recurrent tumor from post treatment change (Figure 6). The disadvantages of early generation CTP include limited brain coverage (2-4 cm. in 16 or 64 slices MDCT) and radiation doses. These drawbacks make MRI seem more favorable.
Perfusion MRI (pMRI) is a technique studying brain perfusion. It has been accepted as a standard imaging tool, together with DWI to identify penumbra area for intraarterial r-TPA (Figure 3). The principle of pMRI is similar to CTP but detects changes in signals during passage of Gd into the brain. The uses of Perfusion MRI are similar to CTP above. Studying permeability status of vasculature by measuring Ktrans proved to be more accurate than MRS in detecting recurrent brain tumor.
There are other MRI techniques for the study of cerebral perfusion which do not inject contrast media, namely arterial spin labeling (ASL) and blood-oxygen level dependent (BOLD). These techniques are based on observing changes of signal of intrinsic paramagnetic substances in the blood passing into the tissue.
BOLD is more widely used to demonstrate activated neurons. The principle of the technique is detecting changes of signal during changes of cerebral blood flow and oxygen consumption of the activated neurons. It has been reported in studying brain function in AD, psychiatric disorders and planning surgery for temporal lobe epilepsy or brain tumor (Figure7).
Studies using fMRI in comatose patients reported different brain responses to environment in individual cases. Coleman M, et al reported different levels of response to sounds in a group of vegetative patients. Owen A, et al. reported a case of a patient at the vegetative stage due to traumatic brain injury and found activated brain area during which the patient was told to imagine walking in her own house or playing tennis. The patient recovered from comatose status months later. These studies may be helpful for prognosis assessment.
Another study with fMRI in soldiers with post- traumatic stress syndrome found excess areas of brain activation when the soldiers were shown violent pictures. This study may lead to more research into better treatment for this condition.
Inventions and applications of new technologies in brain imaging are ongoing. Combinations of these advanced techniques or parallel imaging are increasingly used, so as to compensate for the shortcomings of individual techniques. The more we know about our brains, the less we need have nightmares about untreatable diseases.