Stem cells based therapies are one of the most promising areas for translational research. Therapeutic applications of stem cells provided cure in many untreatable injuries and diseases where recent medicine reached the limitation.1 Mesenchymal stem cells (MSCs) can be differentiated into several cell types and could be a promising source for cell-based therapy, MScs have been shown to promote tissue repair by enhancing the production of growth factors and cytokines.2-4 Dental pulp stem cell (DPSC) was first isolated from human pulp tissue by Gronthos and colleagues in 2000.5 DPSCs have been shown to be used in many therapeutic applications such as bone regeneration and skin and shown remarkable properties in many pathologies requiring tissue repair such as multilineage differentiation capacity, vasculogenesis capacity, anti-inflammatory and immune-modulative activities.6-8 In veterinary medicine, stem cells were used for treatment for musculoskeletal injuries in horses and dogs.9-13 However, only a few studies have been conducted for clinical application of dental pulp stem cells in veterinary patients. Our studies have reported therapeutic effects of deciduous teeth stem cells for repair and maintain tissue functions in many diseases such as: recovery from infarcted myocardium; reconstruction of damaged corneal epithelium; therapeutic effect for chronic osteoarthritis; tendonitis; and chronic wound repair.14-16 The use of stem cells therapy has been hypothesized as a good choice in terms of effective treatment for tissue regeneration. However, the important points in DPSCs biology, such as homing, immune-regulation and long-term follow up require further studies of underlying mechanisms to support the application of DPSCs as a standard treatment in the future.
Allogenic dental pulp stem cells transplantation
Dental Pulp Stem Cells (DPSCs) were supported by the BioEden Asia Tooth Cell Bank. Cells were cultured in Dulbecco’s modified Eagle’s medium (Sigma-Aldrich, St. Louis, MO) supplemented with 10% fetal bovine serum (Invitrogen) and 1% penicillin/streptomycin at 37 °C, 5% CO2. Cells were harvested and collected from the culture at 80% confluency via trypsin-ethylene diamine tetraacetic acid (trypsin-EDTA) treatment (Figure 1). DPSCs at passages 4-8 were characterized by fluorescence-activated cell sorting analysis. DPSCs of different donors were freshly prepared and were admin- istered under aseptic conditions. The second transplan-tation was made 2 weeks after the first transplantation.
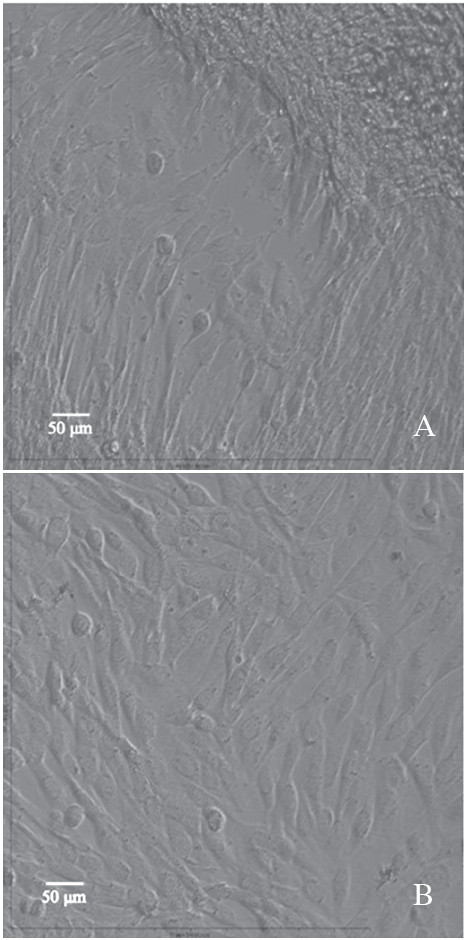
Figure 1: Photomicrograph of dental pulp stem cells (DPSCs) isolated from pulps tissue of the dog teeth. Cells aligned close to the pulp tissue showed in primary culture (A) and become semi-confluent in 25 cm2 flasks in 4-6 days (B).17
Applications of dental pulp stem cells
- Myocardial repair
The therapeutic effects of multipotent Stem Cells from Human Exfoliated Deciduous teeth (SHED) were examined. Thirty adult male New Zealand White rabbits underwent a left thoracotomy approach to produce chronic infarcted heart. The marginal branch of the left circum- flex coronary artery was ligated over 8 weeks to produce an ischemic area of 20-25% of the left ventricle (LV). SHEDs were freshly prepared and 1.0 ml of 106 cells was injected into each of the eight rabbits via the marginal ear vein. Echocardiography and heart rate variability (HRV) were measured to reflect cardiac function. The infarcted size measurements were performed at the end of each experiment. The SHED treatment groups show a significant improvement in cardiac autonomic tone and reduction in infarcted size. Dental pulp stem cell injection confirmed a restoration of the heart (Figure 2). The results suggest that SHED could provide an alternative selection of precursor cells for cardiac repair.
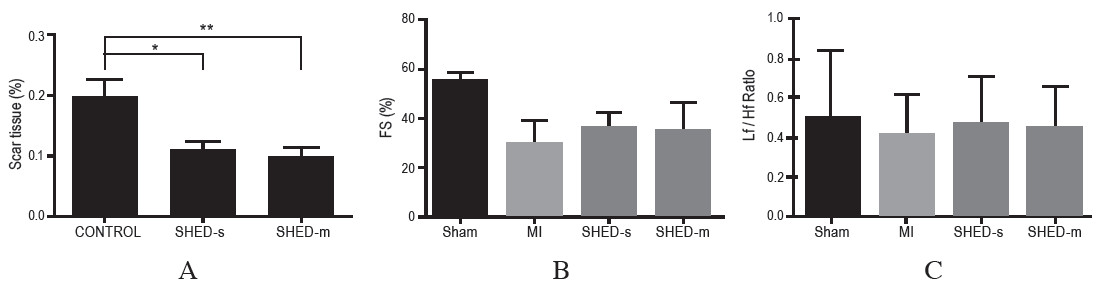
Figure 2: Effect of SHEDs intravenous injection on scar tissue (A); represented heart section from untreated group (Control) compared to single SHEDs-treated (SHED-s) and multiple-treated (SHED-m), Values are mean ± SEM, *p < 0.05 and **p < 0.01. Correlation among Fraction Shortening (FS) in (B) and Heart Rate Variability in (C).
- Osteoarthritis (OA)
The production of canine dental derived stem cells and their possible application in cellular therapy for dogs was evaluated. The clinical effects of multiple intra- articular injections of 5x106 pDSCs were evaluated on 6 dogs with lameness associated with OA of the coxofemoral joints lasting on average 3 months. The second doses of pDSCs were delivered within 14 days after the first injection. Clinical outcomes were evaluated by radiographic evidence,gait changes including persistent lameness at walk or trot,limited range of motion with pain and responses to a questionnaire by the owners.
Results showed significantly better clinical outcomes such as decreased patient discomfort, increased functional ability, reduced aggressive behavior, and improved quality of life. Although radiographic findings did not confirm a positive outcome from the joint morphology, there was a significant reduction in pain without progression observed after treatment (Figure 3). These findings suggest that multiple doses of allogeneic dental tissue derived stem cells transplantations provide significant potential for clinical uses in the treatment of lameness, and pDSCs might be a novel strategy in the cell therapy for OA.
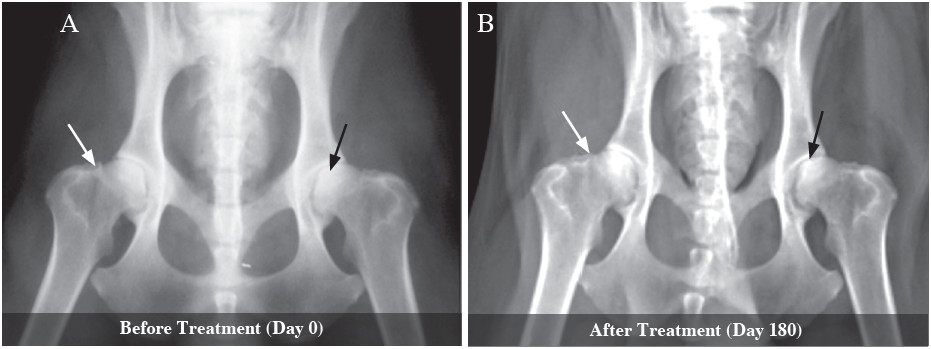
Figure 3: Radiographic findings before pDSCs injection in (A) and after pDSCs injection in (B) present subchondral sclerosis (black arrow), osteophyte formation on distal femur (white arrow).17
- Corneal wound healing
The current study investigates whether sub-conjunctival injection of dental pulp stem cells (DPSCs) promotes corneal regeneration and evaluates the efficacy of puppy deciduous teeth stem cells (pDSCs) in the treatment of corneal ulcers in dogs. In the corneal ulceration model, 5x105 cells DPSCs were injected into the subconjunctival space, and the corneal transparency of the eyes that underwent pDSCs injection improved throughout the follow-up period (Figure 4).
The clinical data were confirmed by histological analysis, and Reverse Transcription-olymerase Chain Reaction (RT-PCR) analysis of connexin 43 (Cx43). Injection of DTSCs showed a significant difference in the epithelial cell layers and Cx43 and a change between the control and treatment groups, suggesting that DPSCs promotes corneal reconstruction. These results suggest that pDSCs provide cell renewal in corneal wound healing and demonstrate the potential of the administration of pDSCs for clinical applications.
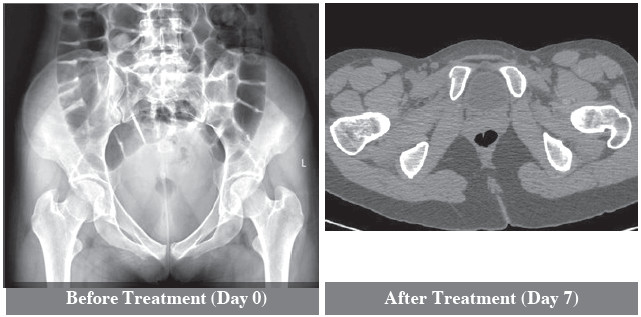
Figure 4: Corncal Ulcer post injection of DPSCs via sub-conjunctiva route resulted in healing within 7 days
- Tendonitis
Horses with superficial digital flexor tendon injury (SDFT) were treated using allogenic DPSCs injected into the lesions. The tendon lesions were monitored clinically and ultrasonographically. There were clinical improve- ments with less lame horses. The horses recovered and returned to their usual performance after completion of treatment without a recurrent injury. DPSCs injection is safe and seems to reduce re-injury. Our study might confirm evidence for the efficacy of DPSCs for the treatment of tendon injury in sport horses.
- Chronic wound repair
Multiple doses of allogeneic DPSCs suspension were intravenously injected into 5 patients with large and impaired-healing wounds. Injections of DPSCs enhanced the wound-healing rate and minimize scar formation. Patients exhibited immediate recovery with no complica- tions. The overgrowth of granulation tissue was visualized within 5-7 days after DPSCs transplantation. This showed a significant difference in the healing process in the wound bed as shown in Figure 5. Injection of DPSCs was a good choice in terms of wound regeneration and healing. Our results suggest that DPSCs may provide a new approach for the treatment of chronic and delayed- healing wounds.

Figure 5: Chronic wound injections of DPSCs promoted wound healing after day 28 and the healing capacity was improved throughout the follow-up
Multiple doses of dental pulp stem cells (DPSCs) improve the clinical outcome of many diseases and might replace drug therapy. However, the treatment cannot be recommended until more clinical cases have been evaluated. Further clinical studies with a longer follow-up period may be necessary to assess these initial clinical obser- vations. However, our study serves as a valuable model for pre-clinical evaluation of stem cells applications for human beings and also for veterinary patients. Our study has shown that administration of allogenic DPSCs were safe and can be applied on the basis of our results to improve the patient’s quality of life.
Our study has shown the efficacy of DPSCs treatment for many diseases and provided support for applying this treatment to humans in the future.
The authors are grateful to Dr. Petcharin Srivattanakul, laboratory director of BioEden Asia Tooth Cells Bank, for providing the basis for this study.