Orthopedic surgeon operated shoulder ultrasound as an extension of physical examination is gaining favour in Europe and the USA, but not so in Thailand.Ultrasonography of the rotator cuff was first presented at the American Institute of Ultrasound in Medicine (AIUM) in 1977.1 Subsequently, Middleton et al. published a technique of ultrasonography of rotator cuff in 1984,2 followed by ultrasonographic detection of rotator cuff tear in 1985.3 Technological improvements in ultrasound machines and well-defined ultrasound examination protocols4,5 has allowed for better accuracy in diagnosis and more widespread in-office use by different medical specialties. In spite of evidence of the accuracy of orthopaedic surgeon operated ultrasonographic diagnosis, and benefits of its in-office use,6-8 many orthopaedic surgeons are hesitant to incorporate diagnostic ultrasound in their9 practice. We recently acquired an ultrasound machine for our department and have been using it as an extension of physical examination for various musculoskeletal problems. In this report we focus on our experience in using ultrasonography for shoulder problems and through this report would like to encourage more orthopaedic surgeons to incorporate use of ultrasound in their practice.
Between June 2019 to March 2020 we performed 90 ultrasonographic shoulder examinations in our outpatient setting. All the ultrasonography was performed by the senior author (NB). The senior author had undergone a 2 days’ hands-on musculoskeletal ultrasound training course and had been doing ultrasonographic examinations using borrowed ultrasound machines from other departments for about a year before we were able to acquire a machine for our department. Before each ultrasound examination a thorough clinical history and physical examination of the shoulder was done. Indication of an ultrasound examination included clinical suspicion or objective finding of pathology of rotator cuff. Every patient gave verbal consent for the ultrasound examination. Some patients had the ultrasound examination on more than one occasion. Shoulder ultrasonography was done following the technical guideline of the European Society of Musculoskeletal Radiology (ESSR),10 using SONIMAGE HS1, Konica Minolta Inc., Japan and linear transducer frequency range 4-18 MHz.
The patient was seated comfortably on a stool facing the monitor of the ultrasound machine with the examiner standing behind him towards the side being examined. For examining the biceps tendon, the patient had his arm adducted against his body, his elbow flexed 90 degrees and forearm supinated on his ipsilateral thigh. The biceps tendon was examined in the long and short axis. In the same position the subscapularis tendon was examined in long axis and short axis. Passive external and internal rotation of shoulder was done to check integrity of subscapularis tendon and also to check for subcoracoid impingement and for dislocation of biceps tendon from bicipital groove. The patient was then asked to put his hand on the side being examined like putting it in the back pocket of his trousers so that the shoulder is in extension and internal rotation. The supraspinatus tendon was examined in this position in long and short axis. The subacromial-subdeltoid (SASD) bursa was also visualized in this position. Next, dynamic subacromial impingement was assessed by bringing the arm back to the first position and placing the probesuperiorly in a coronal plane across the lateral edge of acromion and the supraspinatus tendon. The arm was then passively abducted and adducted to visualize gliding of supraspinatus tendon under the acromion process. The infraspinatus tendon was examined from the posterior by placing the probe just below the spinous process of the scapula and tracing the tendon laterally to its attachment to the greater tuberosity. It was also examined in long and short axes. Last of all the acromioclavicular (AC) joint was examined by placing the probe in line with the clavicle across the AC joint. While performing the examination the patient was also educated about the anatomy and any pathology detected was pointed out to him on the monitor. If it was deemed by the examiner that a therapeutic injection could benefit the patient, he was informed and given a choice to undergo the injection or to try another form of treatment first. If the patient preferred to take the injection, it was done right away under the ultrasound guide. All relevant ultrasound images were saved in the hospital’s PACS (picture archiving and communications system) system, and a short written report was also made in the patient’s file.
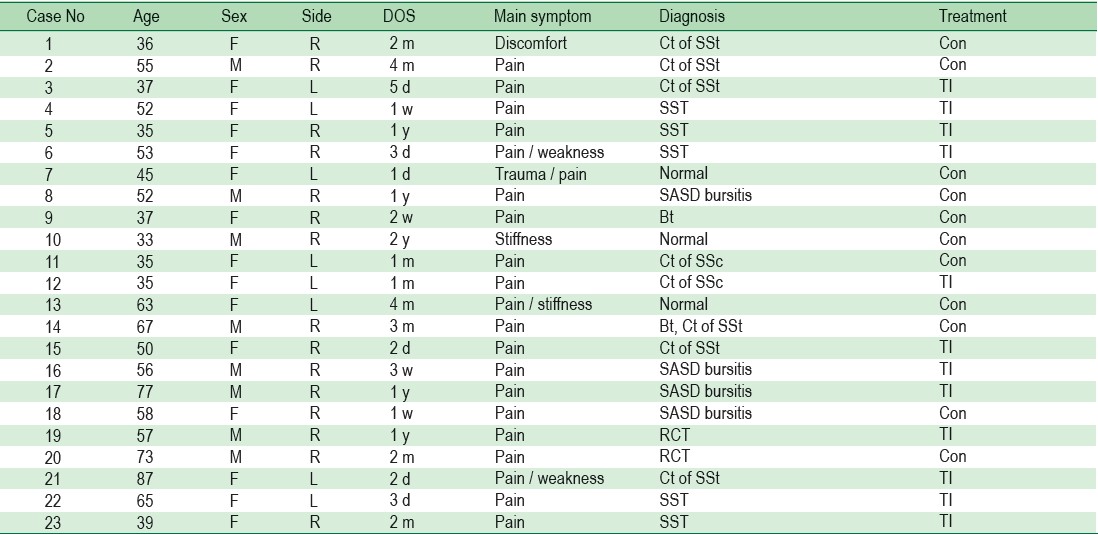
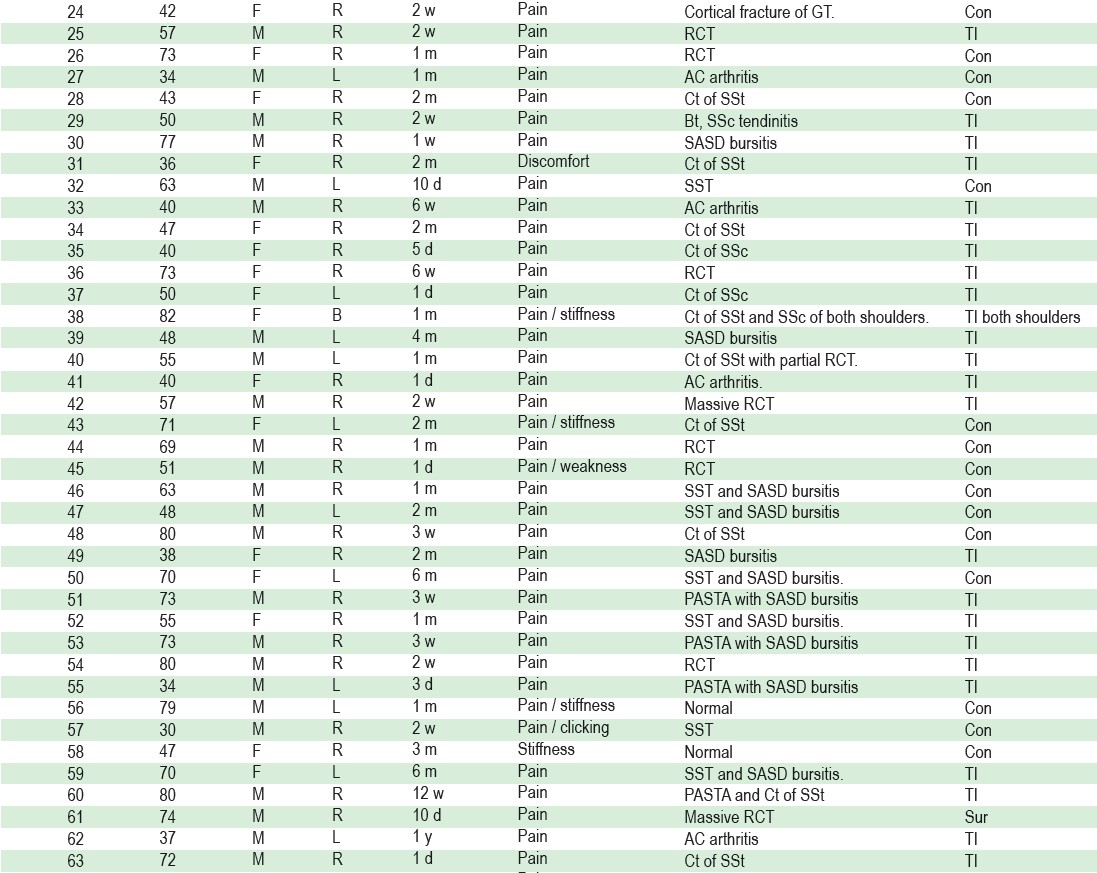
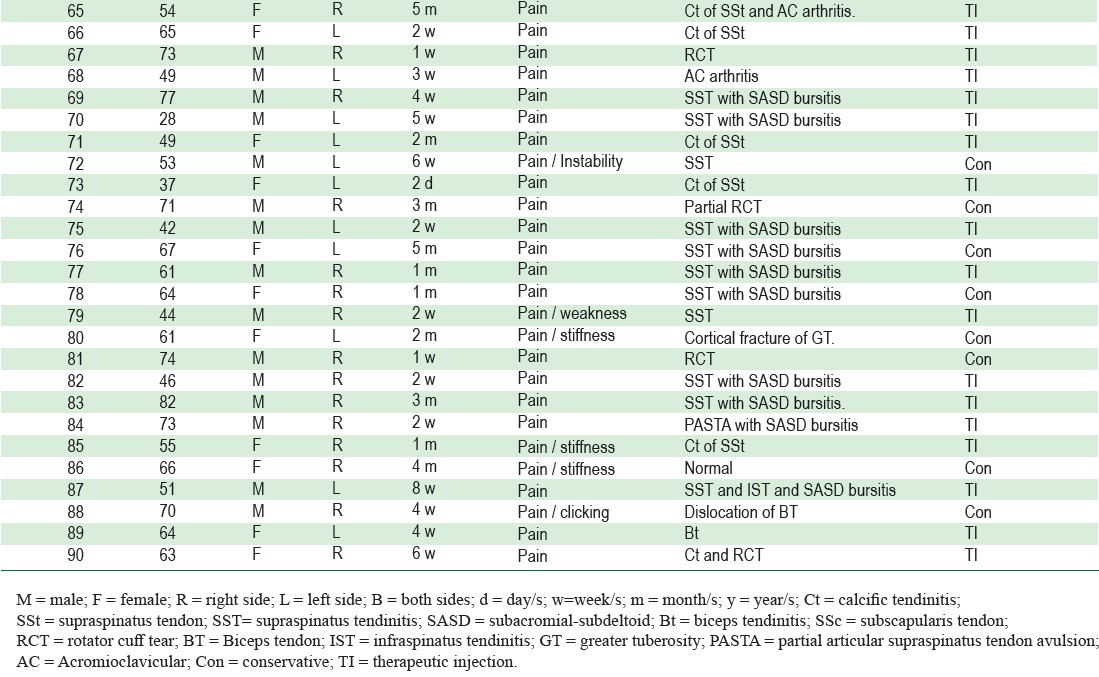
Our patients consisted of 48 males and 42 females, whose ages ranged from 28 to 87 years, with a mean age of 57 years (Table 1). Ultrasound examination was done in 57 right side shoulders, 32 left-side shoulders and 1 on both shoulders. Pain was the most common chief complaint, sometimes accompanied with clicking, stiffness or weakness.
Table 1: Demography, symptoms, diagnosis and treatment of patients.
The ultrasonography pathology detected is shown in Table 2. In 6 shoulders, no pathology was detected, and 111 pathologies were detected in the rest of 84 shoulders. In 27 shoulders, more than one pathology was detected. The most common pathologies detected were SASD bursitis and supraspinatus tendinitis. In 13 shoulders these two pathologies were detected in combination.
SASD bursitis was detected by distension of fluid anechogenicity in the bursa (Figure 1). Supraspinatus tendinitis was detected by loss of normal fibrillar pattern of tendon with focal or diffuse hypoechogenicity. Calcification in tendons was detected by well-circumscribed hyperechogenicity (Figure 2) or hyperechogenic arc with shadow (Figure 3). Full thickness rotator cuff tear was seen as absence of supraspinatus tendon attached to the greater tuberosity. The torn tendon could be seen retracted medially if it was not hidden under the acromion process. The greater tuberosity is seen covered by bursal tissue and deltoid muscle (Figures 4A,B), or by fluid anechogenicity replacing the tendon in the gap (Figure 5). Sagging of peribursal fat and cortical irregularity of greater tuberosity could also be seen in both long and short axis (Figures 4A,B). Partial thickness tear of rotator cuff is seen as hypoechoic or anechoic changes in the tendon (Figure 6).
Acromioclavicular joint arthritis shows up as effusion in the AC joint seen as ballooning out of joint capsule or geyser phenomenon (Figure 7). Biceps tendinitis was detected by loss of fibrillar pattern in the tendon and fluid anechogenicity around the tendon (Figures 8A, B). We were also able to detect 2 cases of cortical fracture of greater tuberosity causing persistent post-traumatic pain where x-rays were not able to detect any bone injuries (Figure 9). One case of biceps tendon dislocation was detected on seeing the biceps tendon on the lesser tuberosity and empty bicipital groove (Figure 10). We performed 54 therapeutic injections under ultrasound guide including 34 injections into SASD bursa (Figure 11), 13 injections around calcific mass, 5 injections into AC joint and 2 injections into bicipital synovial membrane. In one case we were also able to demonstrate integrity of rotator cuff 3 months post arthroscopic rotator cuff repair (Figure 12A,B).
Table 2: Ultrasonographic pathologies detected.
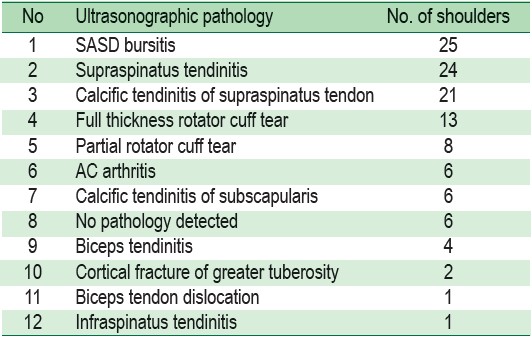
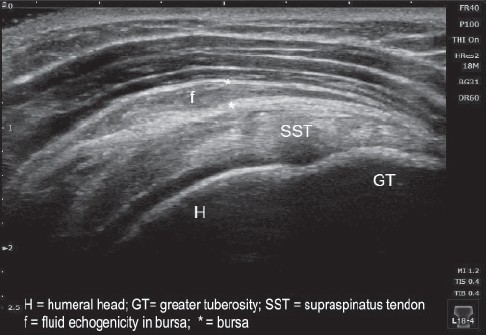
Figure 1: Long axis of supraspinatus tendo demonstrating fluid in SASD bursa indicating SASD bursitis.
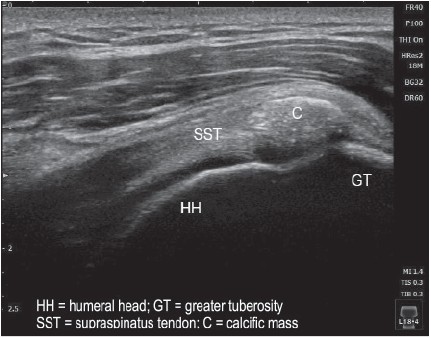
Figure 2A: Long axis of supraspinatus tendon demonstrating calcific tendinitis.
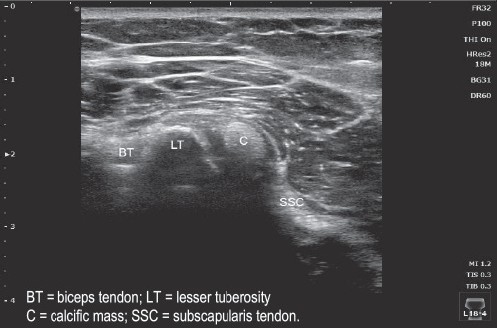
Figure 2B: Short axis of subscapular tendon demonstrating calcification in tendon.
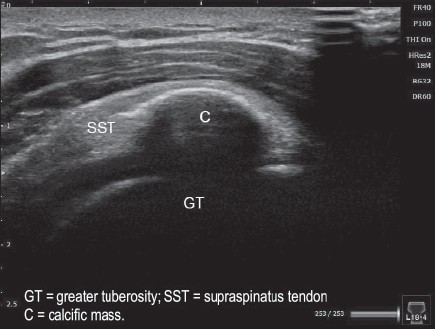
Figure 3: Long axis of supraspinatus tendon demonstrating calcific tendinitis in tendon.
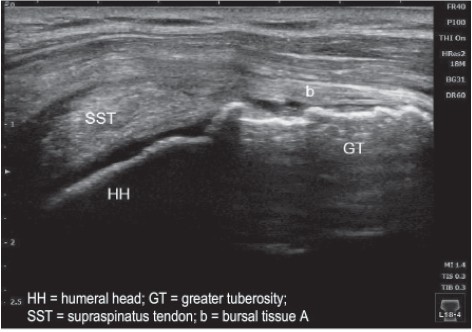
Figure 4A: Long axis of supraspinatus tendon demonstrating full thickness tear of the tendon.
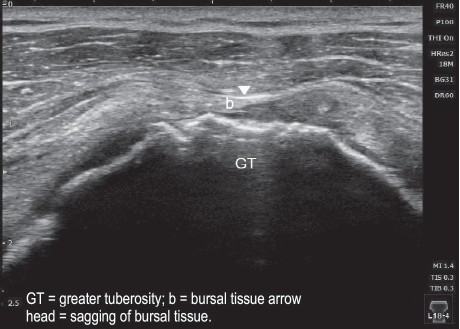
Figure 4B: Short axis of supraspinatus tendon demonstrating full thickness tear of the tendon.
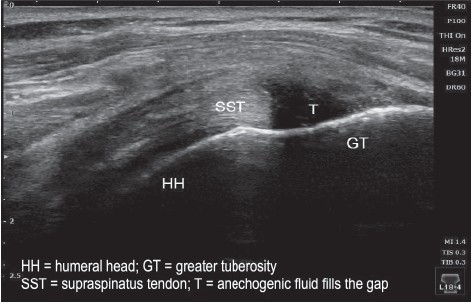
Figure 5A: Long axis of supraspinatus tendon demonstrating full thickness tear of the tendon.
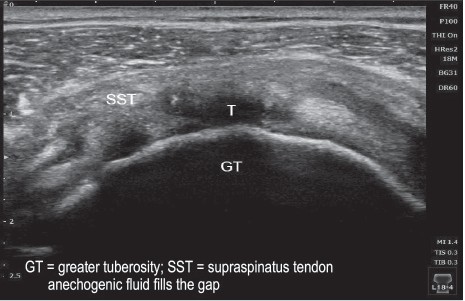
Figure 5B: Short axis of supraspinatus tendon demonstrating full thickness tear of the tendon.

Figure 6: Long axis of supraspinatus tendon demonstrating partial thickness tear of the tendon.
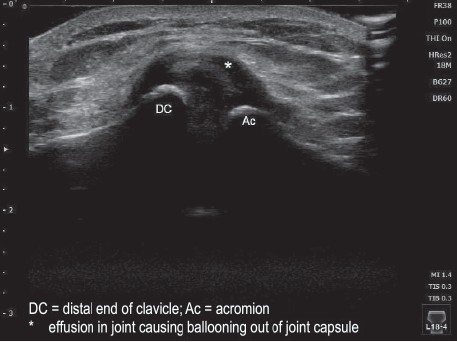
Figure 7: Long axis across acromioclavicular joint demonstrating AC joint arthritis.
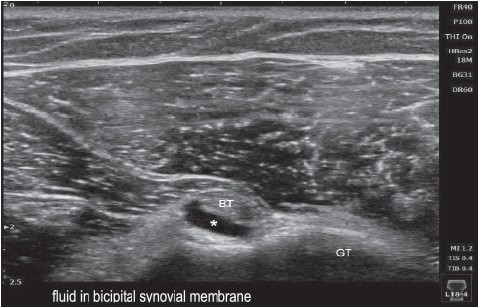
Figure 8A: Short axis of biceps tendon demonstrating biceps tendinitis.
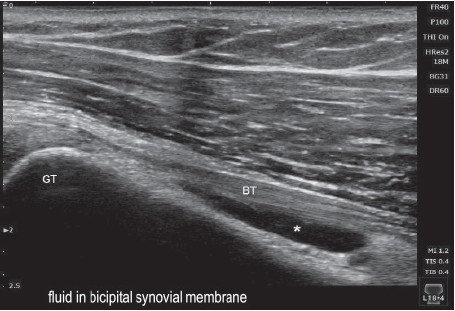
Figure 8B : Long axis of biceps tendon demonstrating biceps tendinitis.
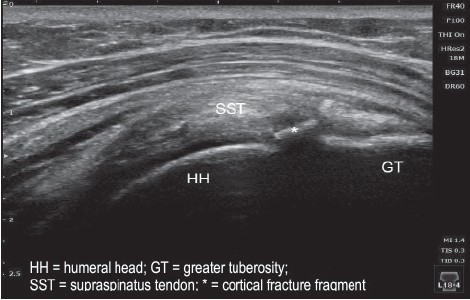
Figure 9A: Long axis of supraspinatus tendon demonstrating cortical fracture at junction of greater tuberosity and humeral head.
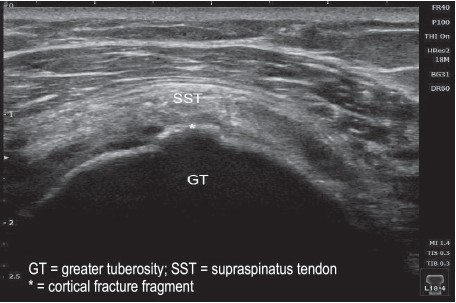
Figure 9B: Short axis of supraspinatus tendon demonstrating cortical fracture at junction of greater tuberosity and humeral head.
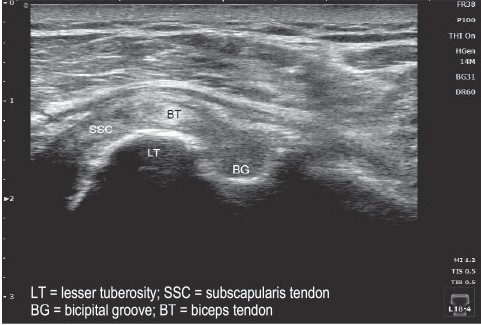
Figure 10: Short axis of biceps tendon demonstrating dislocation of biceps tendon from bicipital groove.
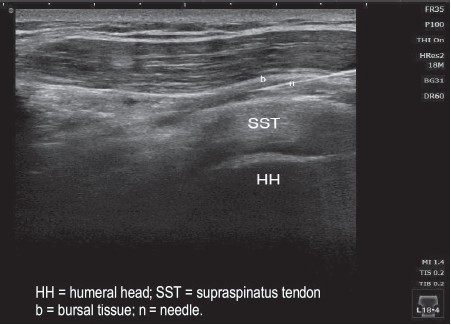
Figure 11: Long axis of supraspinatus tendon demonstrating ultrasound guided injection into SASD bursa.
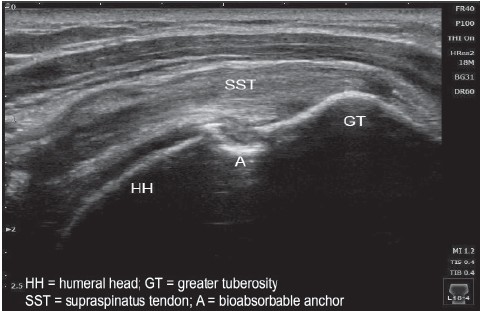
Figure 12A: Long axis of supraspinatus tendon demonstrating post rotator cuff repair integrity of supraspinatus tendon.
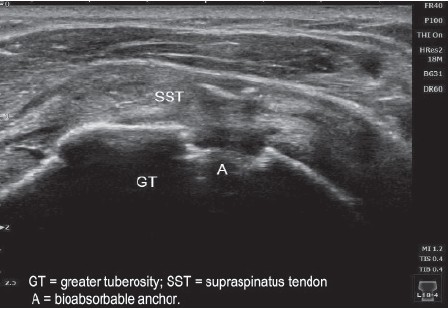
Figure 12B: Short axis of supraspinatus tendon demonstrating post rotator cuff repair integrity of supraspinatus tendon.
The first report on use of office–based ultrasound by orthopaedic surgeons for the purpose of diagnosing rotator cuff tear was by Roberts et al11 in 1998. There have been several reports of orthopaedic surgeons performing office-based shoulder ultrasound6-8, 11-18 (Table 3). All of these reports have focused on the detection of rotator cuff tears. The mean sensitivity for the ability of an orthopaedic surgeon to detect a full-thickness rotator cuff tear with ultrasound was 92.4% (range 70%-100%). The mean sensitivity in detecting partial-thickness rotator cuff tear was 67% (range 7%-95%). The overall specificity in detecting a normal tendon was 89% (range 80%-100%).9 In a meta-analysis on accuracy of ultrasound for rotator cuff tear, Smith et al19 reported orthopaedic surgeons to have the second highest accuracy, second only to musculoskeletal radiologist, beating ultrasonographer and general radiologists.
Table 3: Patient characteristics at baseline (n = 49)
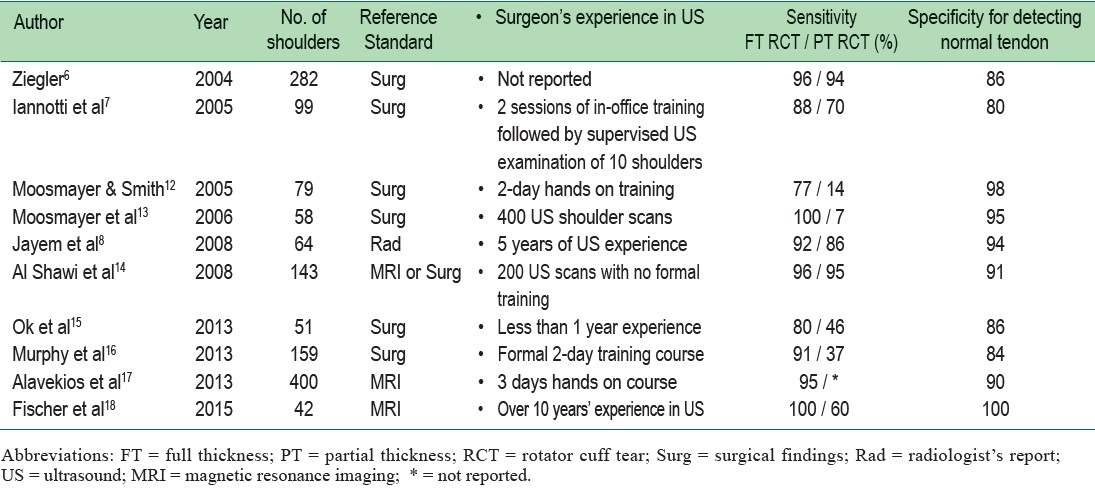
Several reports have addressed the issue of how much training and experience is needed for orthopaedic surgeons to be proficient in detecting rotator cuff tears by ultrasound. 7, 12, 14 -17, 20 Current training guidelines in the use of musculoskeletal ultrasound for clinicians who are not radiologists require the learning clinician to be supervised directly by a qualified musculoskeletal ultrasonographer or radiologist for at least 150-300 scans.21-23 Churchill et al,20 recommended a 4 hour initial training followed by 20-30 examinations to recognize normal anatomy followed by another 20-30 examinations of rotator cuff pathology coupled with MRI or arthrogram for verification. Despite these recommendations it has been shown that surgeons could develop proficiency in ultrasound assessment of rotator cuff integrity in a relatively short period of time using different independent training protocols.7, 12, 14, 16, 17, 24 Murphy et al16 showed that after a 2-day formal training course, orthopaedic surgeons could be trained to reliably evaluate rotator cuff integrity using ultrasound within 50 to 100 scans. Alavekios et al17 showed that after 3 days of hands-on instructional course orthopaedic surgeons accuracy to detect full-thickness supraspinatus tears plateaued after 100 ultrasound scans. Based on the experience of Murphy at el,16 the British Elbow and Shoulder Society (BESS) produced a guideline for accelerated learning method for shoulder ultrasound specifically designed for shoulder surgeons.25 Iossifidis et al,26 using similar protocol as recommended by BESS guideline, demonstrated that orthopaedic surgeons were able to achieve comparable sensitivity and even supersede the specificity of those achieved by musculoskeletal radiologists in detecting rotator cuff tear by ultrasound after about 140 scans. A study on the effectiveness of training workshop in shoulder ultrasonography for orthopaedic postgraduate trainees conducted by an orthopaedic shoulder surgeon27 showed that a single workshop session could be effective in the trainees being equipped with basic ultrasound techniques and that the trainees support ultrasound training in becoming an integral part of orthopaedic training.
Surgeon-operated ultrasonography in a shoulder clinic can significantly reduce the time to treatment and the financial cost for patients with rotator cuff tear.28 Several reports have shown benefits and accuracy of using ultrasound to evaluate postoperative rotator cuff healing.29-31 There have also been cadaveric studies showing better accuracy of injections into acromioclavicular and glenohumeral joints using ultrasound guide compared with palpation or blind injections.32-34
Orthopedic surgeons use of ultrasound is gaining favour in Europe and America. It is still rare in Thailand where patients are more commonly referred to the radiology department. Ultrasonography is non-invasive, has virtually no side effects and allows the rotator cuff to be visualized dynamically during rotation and elevation of the shoulder. It is cost effective and time efficient and allows patients to see their own pathology, leading to better understanding of the pathology and a constructive discussion on the treatment options. Orthopaedic surgeons have the advantage of better knowledge of shoulder anatomy through surgical experience and understanding of shoulder problems through clinical examination, which may shorten their learning curve for ultrasound examination of the shoulder.
Our purpose in this report was to present our initial experience with incorporating musculoskeletal ultrasound examination as an extension of physical examination of the shoulder. There is a plethora of evidence of its accuracy and benefits as an office-based diagnostic and therapeutic use. With some training and practice an orthopaedic surgeon can become proficient in its use to the benefit of their patients. We would like to encourage more orthopaedic surgeons to take up shoulder ultrasonography as part of their routine examination of shoulder problems and also consider integrating shoulder ultrasound training to the residency and fellowship training programs.