A 55-year-old, morbidly obese man body weight (BW) of 104 kg, body mass index (BMI) of 30.5 kg/m2 with known history of type 2 diabetes mellitus, hypertension, dyslipidemia and primary hypothyroidism, presented with acute chest pain and heart failure in 2007. Frank pulmonary edema and cardiomegaly were documented from admission chest film (Figure 1). The electrocardiogram (ECG) (Figure 2) showed sinus tachycardia, left atrial enlargement, tall R in V2 with ST depression in V2-4, Q wave and mild ST segment elevation in inferior leads. The cardiac enzymes were elevated, troponin T (TnT) of 1.84 ng/ml, CK-MB of 94.15 ng/ml. Echocardiography revealed severe hypokinesia of antero-apical-lateral, infero-posterior wall, causing low left ventricular ejection fraction (LVEF) of below 0.30. After administration of aspirin, clopidogrel, heparin and glycoprotein IIb IIIa antagonist, he was referred for emergent coronary angiography
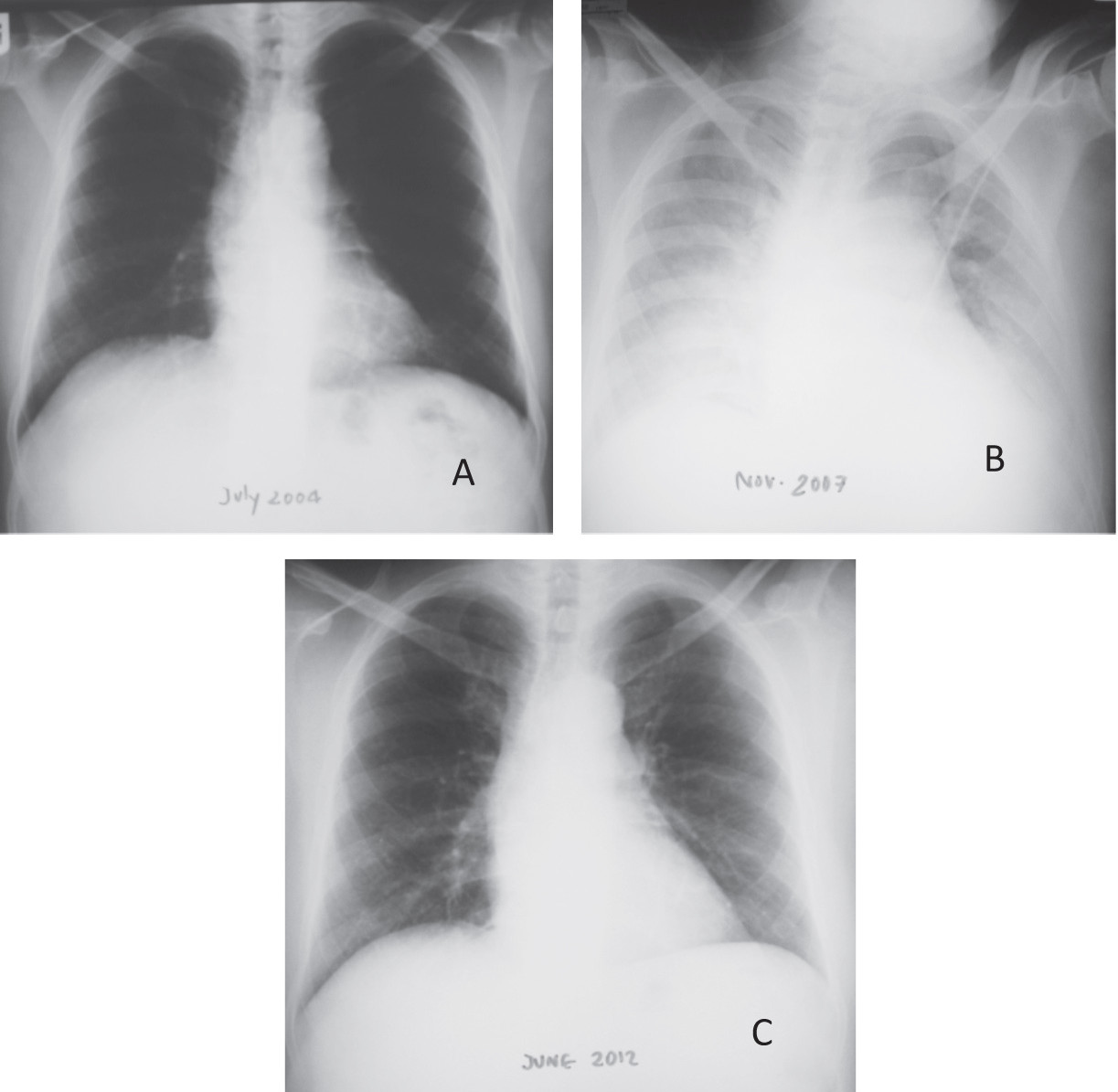
Figure 1: Chest film shows the baseline normal heart size in 2004 (A). Cardiac enlargement and full blown pulmonary edema in 2007 is shown in (B). Reduction of heart size is noted in 2012 (C).
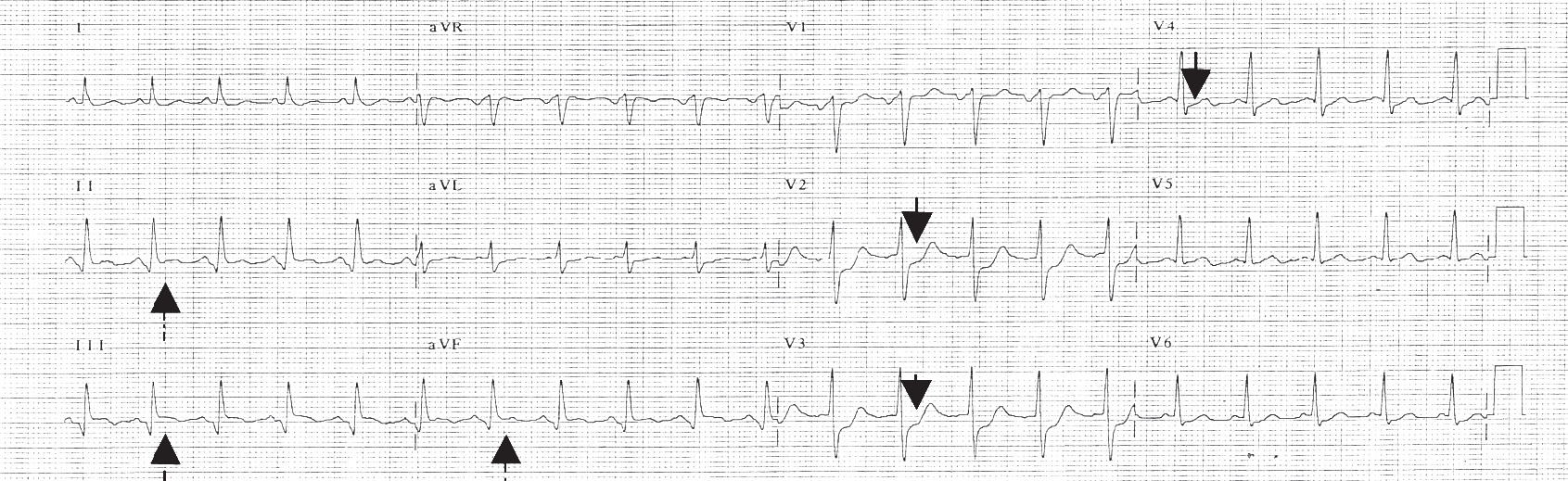
Figure 2: The first ECG in 2007 showed sinus tachycardia, 124/min, early transition (tall R in V2) with depressed ST segment in V2-4 (black arrow). Q wave and mild ST segment elevation (dashed arrow) was observed in inferior leads.
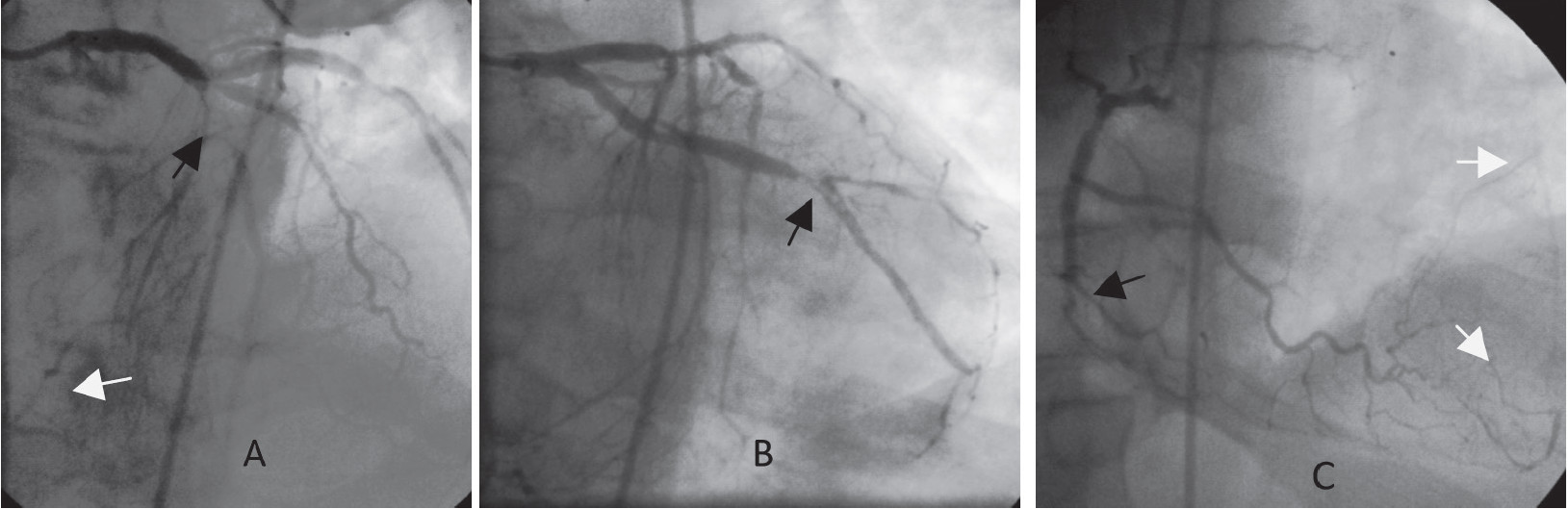
Figure 3: The occluded proximal LAD (A, black arrow) and the RCA (C, black arrow) are illustrated. Collateral supply from the LAD and Cx arteries to distal part of RCA (A, white arrow) and from RCA to distal part of LAD (C, white arrows) suggested remote obstruction of both vessels. The thrombus containing lesion in mid Cx/OM artery (B) was likely the culprit lesion
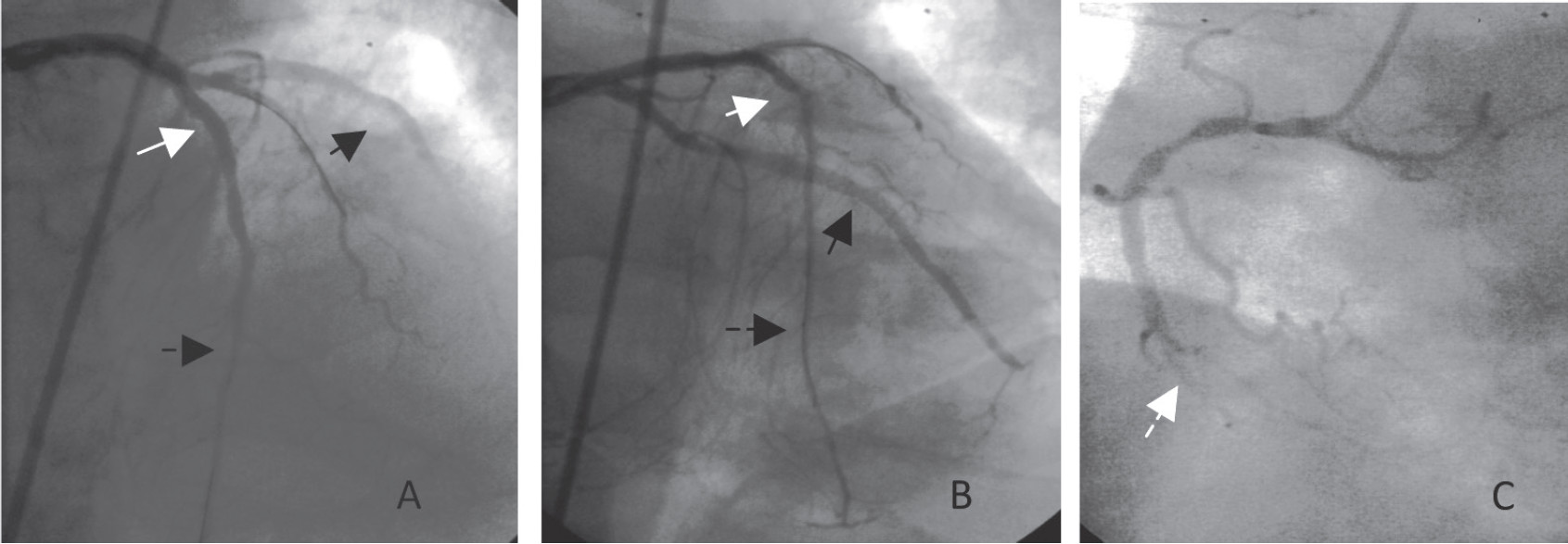
Figure 4: Final results of stent implantation in the Cx/OM (A&B, black arrow) and the LAD arteries (A&B, white arrow) were illustrated. The diffuse small irregular lumen of the distal LAD artery (A&B, dashed black arrow) was also noted. The old occluded RCA (C, white dashed arrow) was left for medication.
Emergent coronary angiogram (Figure 3) illustrated severe 3-vessel coronary artery disease (CAD) with two totally occluded vessels, the proximal left anterior descending (LAD) and the dominant right coronary artery (RCA). Collateral supply from the left coronary artery to RCA and vice versa was noted suggesting a chronic occlusion of these arteries. In addition, there was a thrombus containing lesion, causing subtotal stenosis of the mid part of circumflex (Cx) artery which caused this event.
To support the depressed left ventricle, an intra-aortic balloon counter-pulsation (IABP) was performed and did improve his condition. The heart rate decreased from over 120 to 108 bpm. Coronary bypass surgery (CABG) was recommended to the patient and his family members. All of them insisted to have emergent coronary angioplasty for this critical event. Balloon dilatations, following by metallic stents implantation were successfully performed, first at the mid Cx/OM and later at proximal LAD arteries (Figure 4 A-B). The chronically occluded RCA (Figure 3 C) was left for medication. After intervention, he recovered well and was discharged home on the 7th day. The home medication included aspirin, clopidogrel, statin, eltroxin, diuretic, anti-diabetic, angiotensin converting enzyme inhibitors and beta-blockade. The elective CABG surgery was recommended whenever he had recurrent ischemic symptoms, either spontaneous or after stress test induction
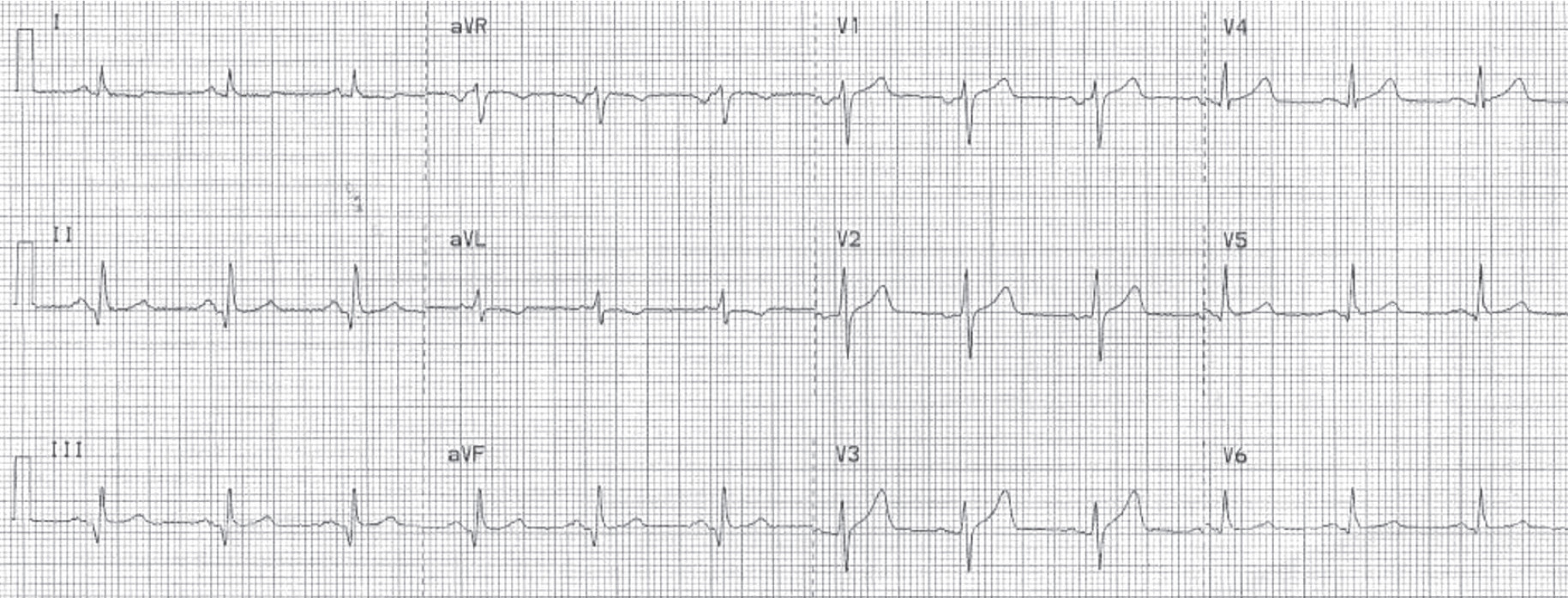
Figure 5: The ECG in 2012 shows no new ischemic changes. Both Q wave with mild ST elevation in inferior leads and subtle ST depression,
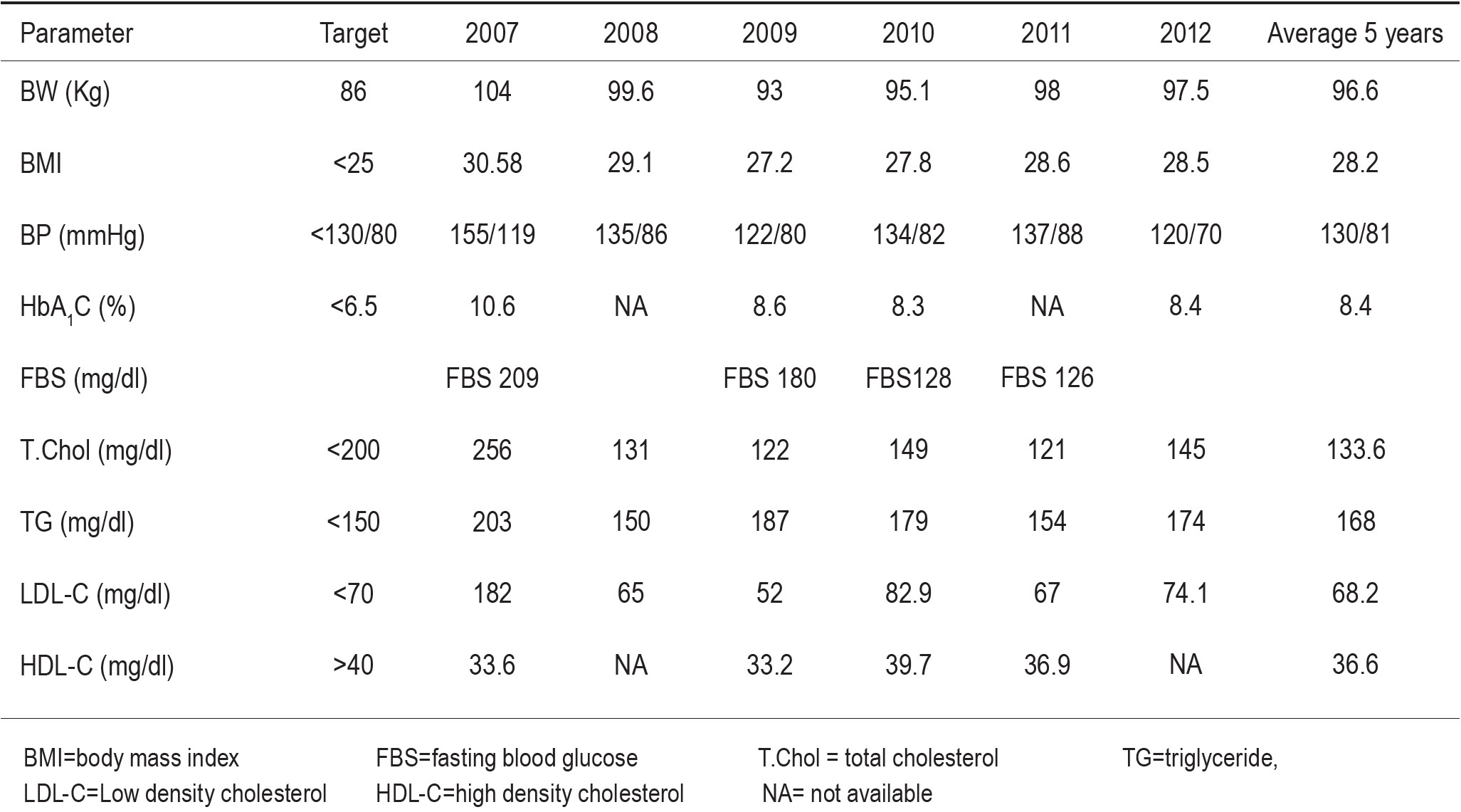 Table 1: Most of his biochemical profiles improved from 2007-2012
Table 1: Most of his biochemical profiles improved from 2007-2012
After being discharged, he intentionally changed his life-style. As a vegetarian, he reduced multiple meals to twice a day. Under his wife’s care, no fried, salty food and no late dinner beyond 19.00 were allowed. He regularly walked, for 30-45 minutes, nearly every day, and consistently took all medication. His dedication resulted in declining of BW, at least 0.5 kg/month. By the year 2009, his BW had decreased 10.5 %, from 104 to 93 kg. The total cholesterol was reduced from 256 to 122 mg/dl. The LDL-C reduced from 182 to 52 mg/dl. The HDL-C increased from 33.6 to 36.9 mg/dl in 2010 (Table 1).
In 2012, he had a brief episode of post-prandial epigastric discomfort, lasting for only few minutes, and decided to come for a checkup. ECG (Figure 5) showed sinus rhythm (75 bpm) and unchanged pattern of inferior Q wave and subtle (< 0.5 mm) ST depression in leads I, aVL. Echocardiogram showed eccentric LVH, normal wall motion except posterior wall hypokinesia. The LV systolic function increased from below 0.30 to 0.57. However, the TnT was mildly elevated, 0.093 ng/ml, so he was referred for repeat coronary angiography.
Coronary angiogram showed the well-patent stented LAD and Cx arteries with no re-stenosis, see Figure 6. No new lesion had developed. Although the proximal RCA lesion was unchanged, the occluded mid vessel was re-canalized (Figure 6C). This allowed a successful balloon dilatation and stent implantation of the distal RCA (Figure 6D). The patient was discharged home with no complication.
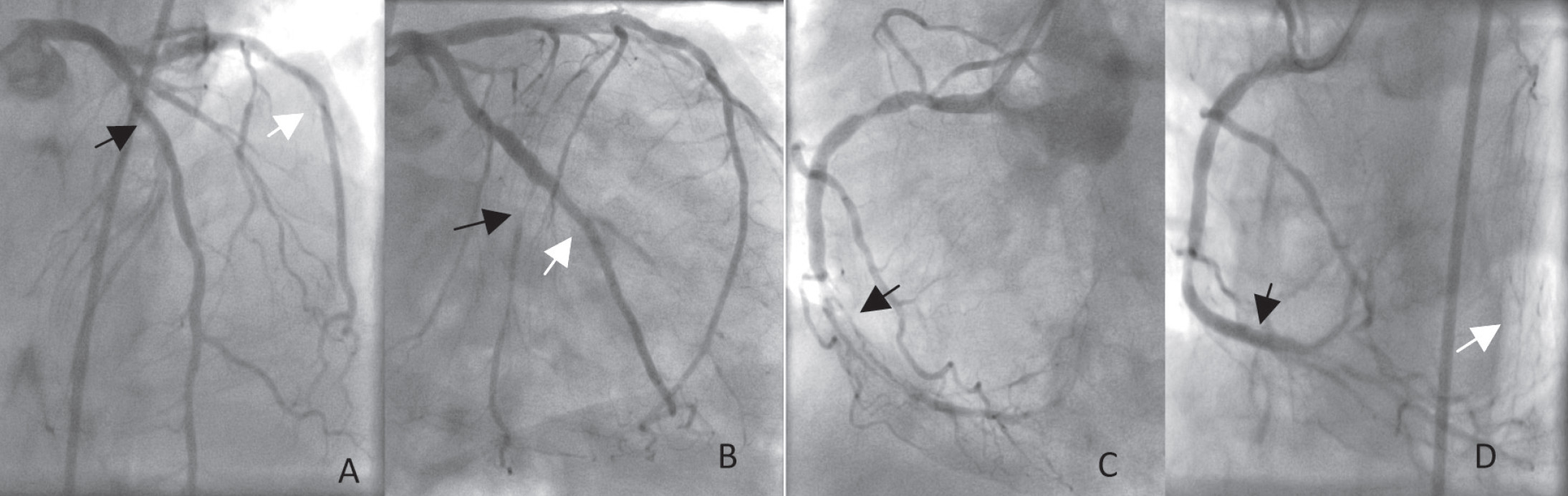
Figure 6: The stented LAD (A, black arrow) and Cx/OM arteries (A&B, white arrow) were patent with no restenosis. The occluded distal Cx (B, black arrow) and RCA (C, black arrow) were spontaneously re-canalized. PTCA with stent implantation of the RCA (D, black arrow) was performed. Increased collateral supply from RCA to distal Cx artery (D, white arrow) was noted after stent implantation
The high mortality candidate
The presence of myocardial infarction, heart failure and poor left ventricular systolic function (EF below 30%) placed our case in a high-fatality subset. According to the Global Registry of Acute Coronary Events (GRACE) study, the calculated risk score was high as 181 and the predicted in-hospital mortality was 9%.1 The GRACE score over 140 indicated urgent (within 24 hours) coronary angiography and revascularization as recommended by the current European Society of Cardiology (ESC), the European Association for Cardio-Thoracic Surgery (EACTS)2 and American College of Cardiology Foundation (ACCF)/American Heart Association (AHA) 2011 guidelines.3 The angiography in 2007 (Figure 3) clearly explained the 1st ECG manifestations. The well-developed collateral supply to the LAD and RCA not only nourished the underlying ischemic but viable myocardium but also indicated the remote occlusion of these two arteries. The recent thrombus-containing lesion in the mid Cx artery compromised the collateral flow to inferior wall causing re-elevation ST segment of the inferior wall and ST depression in pre-cordial leads. With severely stenotic lesions in all three coronary arteries, the calculated SYNTAX score4 was 28.5. This intermediate score (ranging from 23-32) predicted a non-significant but higher major adverse clinical events (MACE) at 12 months if he underwent revascularization by percutaneous coronary intervention (PCI) with drug eluting stent (DES), as opposed to the MACE of coronary bypass surgery (CABG), 16.6% vs. 11.7%, p = 0.1.4 Nevertheless, in accordance with the family’s wishes, bridging PCI with metallic stent implantations of the LAD and the Cx arteries was successfully performed. He recovered well and was discharged home within 7 days. The estimated 6-month mortality by GRACE score, was 13% and the rate of death or myocardial infarction (MI) was high as 40%.1 Although an elective CABG was strongly recommended for better long-term outcome, he did well with no recurrent chest pain for five years.
Benefits of diet, exercise, and weight reduction in CAD cases
Being overweight (BMI > 25-29.9) and obese (BMI > 30) increases cardiovascular disease development and its mortality5,6 as presented in our case. Obesity flourished metabolic syndrome7 produces pro-inflammatory cytokines8 , furnishing pro-thrombotic states9 and accelerates atherosclerosis. Reduction of initial body weight by 5-10% has been shown to improve cardiovascular risk factors and other health benefits.10 This modest body weight reduction can be achieved by combining dietary control and regular exercise.11
Regular aerobic exercise decreases myocardial oxygen demand12, increases coronary flow to microcirculation and improves endothelial function.13 Exercise-based cardiac rehabilitation has been associated with improvement of cardiovascular risk profiles and reduction of all-cause, cardiovascular mortality.14,15 Current secondary prevention guidelines recommend a moderate intensity of physical activity, for at least 30 minutes, continuously or intermittently (preferably 60 minutes) at least 5 days/week.16
Along with walking 30-45 minutes a day, our patient reduced multi-meals vegan diet to twice a day. Generally a vegetarian diet contains less energy, lower percentage of fat and cholesterol but is richer in fiber and folate content if compares with a regular mixed diet.17 The inverse relation between fruit, vegetable and fiber consumption and myocardial infarction has been observed in a large Italian epidemiologic study of 46,693 subjects.18 In one single blind randomized control trial of 406 post-MI Indian patients, the vegetarian assigned group was associated with a significant reduction of total cardiac events including fatal or non-fatal MI and sudden death when compared with the regular diet assigned cases.19 The benefit of low-fat vegetarian diet and intensive lifestyle modification including aerobic exercise had been shown to provide more atherosclerosis regression when compared to the control group.20 By 2009, our patient achieved 10% BW reduction (from 104 to 93 kg; BMI decreased from 30.58 to 27.2 kg/m2 ). His enlarged heart size reduced (Figure 1C) and LVEF became normalized.
An improved angiographic finding in 2012
The very brief episode in 2012 was less convincing for myocardial ischemia. The admission ECG showed no new ischemic changes on top of the old findings in inferior and high lateral leads. Echocardiogram showed improved LV systolic function with normal LVEF of 0.57. While other abnormal wall motion became normalized, hypokinetic posterior wall persisted. This was not surprising since the RCA was occluded for at least five years. However, the mildly elevated TnT, 0.09 ng/ml, indicated repeat angiographic study in patient with known 3-vessel CAD. It was interesting that there was no significant restenosis in all stented arteries and no new lesion was observed. The improvement in luminal diameter of the distal LAD was quite impressive, as much as the re-canalized distal Cx (6B) and the mid RCA (6C) since more progressive lesions would be expected in most diabetic CAD patients. Owing to the small luminal size of the distal Cx, the only intervention was performed in the mid RCA (7D).
Atherosclerosis regression and mortality reduction
Retardation21,22 and regression of the atherosclerotic process23-30 by angiography had been formerly reported in CAD patients treated with lipid lowering agents23,26,27,30 and life-style modification (i.e. physical exercise and low-fat diet).24,28,29,31 Angiographic regression although occurred in modest degree, 3- 10% of diameter stenosis, had been consistently observed23-30 and associated with reduction of clinical events.26,31 However, reduction of both clinical events and mortality had been only shown in the large trials with cholesterol lowering drugs studies.32-36 For example, in 4S studies, there was a 42% reduction in coronary deaths and a 37% reduction in cerebrovascular events in patients treated with simvastatin in comparison with a placebo treated group.32 Recently, plaque regression has been confirmed by a series of cross sectional studies of intravascular ultrasound imaging with simvastatin37, rosuvastatin38,39 and atorvastatin.39 In ASTEROID trial, patients treated with rosuvastatin 40 mg/day achieved significant plaque regression from 64-78% and the mean LDL-C level achieved in this study was 61 mg/dl.38 This result supported the recommended target for lowering the LDL-C in known CAD cases to below 70 mg/dl.40 Along with BW reduction, our patient’s lipid profiles consecutively improved as listed in Table 1. Total cholesterol decreased from 256 mg/dl to 122 mg/dl and the average LDL-cholesterol over the past five years was 68.1 mg/dl. The HDL cholesterol increased from 33.6 to 39.7 mg/dl in 2010. All of these parameters contributed to the angiographic improvement in 2012.
We presented a high risk acute coronary syndrome case with multiple coronary risk factors who had angiographic improvement of coronary stenosis after five years of combined medication and life style modification. Although we did not perform a comparative analysis with digital angiographic measurement, it was clear that there was no new lesion formation observed and two occluded arteries were re-canalized. This case reminds us about the significant role of modest aerobic exercise, controlling diet and good compliance in medication which is the core recommendation in current secondary CAD prevention.