Neonatal jaundice is an important problem occurring in neonates.Approximately 80% of premature and 60% of full-term infantspresent with clinical jaundice during the first few weeks of life.1Inadequate breastfeeding is considered the major cause of jaundice.2,3 Morethan 50% of newborns who have jaundice have this condition due toinadequate breastfeeding.3,4 Low intake of breast milk reduces gastrointestinalmotility, which decreases the excretion of bilirubin by stool output andincreases the intestinal re-absorption of bilirubin into the blood. Thus, theunconjugated bilirubin levels are high and these high levels play an importantrole in aggravating neonatal jaundice.5,6
Generally, bilirubin levels in breastfed neonates have peak values occurringbetween the third and fifth days of life and elevating to the second level thatusually peaks between the tenth and fifteenth days of life. Prolonged neonataljaundice over this period would suggest an etiology other than breastfeedingjaundice.7-9 Thus, the mechanism of breastfeeding and jaundice is notclearly understood. However, some research has consistently identified thatfailure to establish adequate breastfeeding is a leading factor contributing tohigh levels of bilirubin in breastfed neonates9 and 8-11% of these infants candevelop severe neonatal jaundice that can cause long-term damage and anincrease in neonatal death.10
Additionally, increasing numbers of neonatal re-admissions for jaundiceare associated with inadequate breastfeeding.11 During the first two weeks oflife, 85% of breastfed infants are re-admitted to the hospital due to inadequate breastfeeding jaundice. Furthermore, the incidenceis reported to be on the rise.12 Re-admission for jaundice causesmany negative effects on both neonates and their families.These effects include emotional stress, delayed growth anddevelopment, interruption of routine family activities andhigher medical costs.13,14 Therefore, the prevention ofneonatal jaundice due to inadequate breastfeeding, particularlyduring the first two weeks of life, requires health careprofessionals’ urgent attention. Providing appropriate supportwith an emphasis on higher BFF each day may ameliorate theproblem.10,15
Several previous studies have reported that the optimalBFF is at least eight times/day. Optimal BFF is associated withdecreased serum bilirubin levels, increased breast milk intake,weight gain, and frequency of defecation in neonates.16-18According the recommendations from the AmericanAcademic of Pediatrics (AAP) and the American College ofObstetricians and Gynecologists (ACOG),15 the frequency ofbreastfeeding during the first few weeks after birth should beat least eight times/day. Since breastfeeding at least eight times/day leads to successful establishment of breast milk volume,this feeding schedule would be helpful in the management ofinadequate breastfeeding jaundice.
Despite the numerous studies conducted on the relationshipbetween breastfeeding and neonatal jaundice, investigation ofBFF and re-admission for jaundice during the first two weeksof life has not been previously studied. Most previous studieshave focused on describing the link between BFF and bilirubinlevels during the first week of life.19,20 However, the incidenceof re-admission for inadequate breastfeeding jaundice in thefirst two weeks of life is reported to continue to rise.12 Thus,studying these variables might offer a solution to this problem.In this study, the researcher was interested in exploring andcomparing bilirubin levels and re-admission rates for jaundicein neonates with different frequencies of breastfeeding duringthe first two weeks of life. The results from this study couldbe useful for health care providers as preliminary informationfor prevention of inadequate breastfeeding jaundice inneonates.
Descriptive research design was used to explore and comparebilirubin levels and re-admission rates for jaundice during thefirst two weeks of life between neonates who received low andhigh-BFF. The study was conducted in the general and privatepostpartum units at a University Hospital, Bangkok, Thailand,from February to April 2018. Consecutive sampling was usedto enroll the samples who met the inclusion criteria. Thesample consisted of 100 mothers and their term neonates.
The inclusion criteria for the mothers:
The inclusion criteria for the neonates:
Instruments
The following four instruments were used to collect datain this study:
Data collection
After the consent form process, the researcher collectedthe demographic data and measured TcB at the foreheads ofthe neonates using a bilirubinometer at 24, 48 and 72 hoursafter birth. All postpartum mothers were requested to recordBFF, frequency of defecation and amount of formula milkgiven per day and to record these data from Day 1 until Day14 of neonate life in the BFF record form.
When the mothers and full-term neonates were dischargedfrom the hospital, the researcher phoned to ask the data of BFFand re-admission for jaundice in neonates on day 6, 9, 12 and14 of neonate life. The total time required for the telephonefollow-ups was estimated at 5-minutes for each call.
Data analysis
The samples were assigned to two groups due to their meanof BFF during the first two weeks of life. The low-BFF grouphad a mean BFF score of < 8 times/day during the 14-dayperiod, and the high-BFF group had a mean BFF of ≥ 8 times/day during the 14-day period.
Descriptive statistics, namely, frequency, percentage,mean, and standard deviation (SD) were used to describe thedemographic characteristics of the study. The Chi-square wasused to compare demographic characteristic of the subjectincluding parity, induction of labor, level of education, occupation,neonatal gender, method of delivery, whereas independentt-test was used for maternal age, GA, BW, Apgar score, BFF, and amount of formula milk. Comparing personal data, weightloss, frequency of defecation, bilirubin levels and re-admissionsfor jaundice in neonates in the low and high-BFF groups werealso computed by independent t-test and Chi-square. An alphalevel of 0.05 was set as the level of significance. All of the dataobtained by this study were analyzed with the StatisticalPackage of the Social Sciences (SPSS).
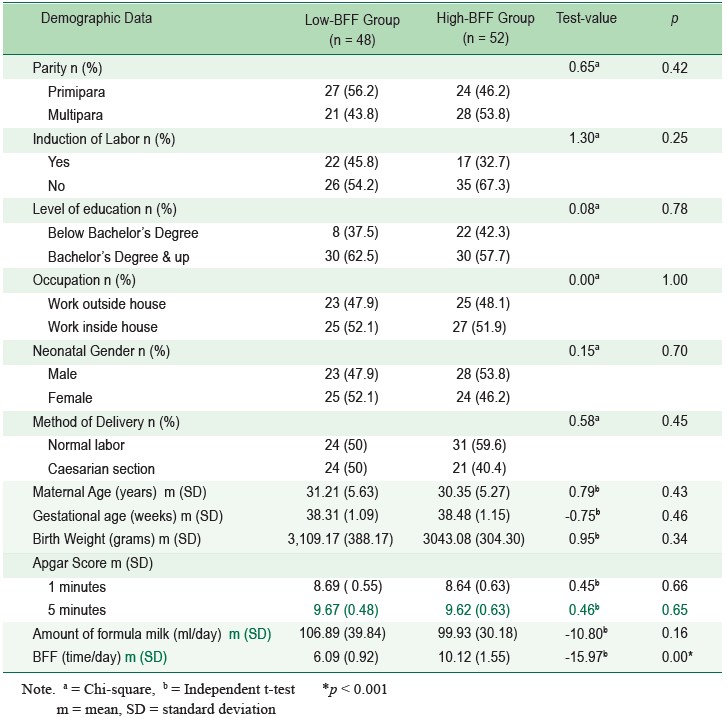
One-hundred mothers and full-term neonates wereincluded in this study. Of these, 48 of them were assigned tothe low-BFF group and 52 were assigned to the high-BFFgroup. The demographic data (parity, induction of labor, levelof education, occupation, neonatal gender, method of delivery,maternal age, gestational age, birth weight, Apgar scores at 1and 5 minutes and amount of formula) of both groups did notdiffer with statistical significance (p > 0.05). However, BFFbetween the neonates in the low and high-BFF groups weredifferent with statistical significance (p < 0.001) (Table 1).
Table 1: The demographic characteristics of the sample (n = 100).
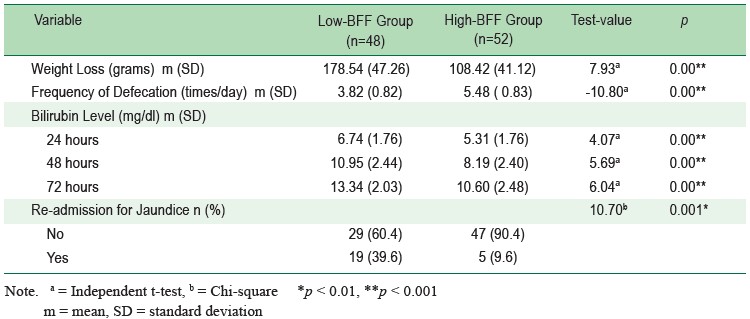
The bilirubin levels of neonates were significantly higherin the low-BFF group when compared with the high-BFF groupat all 3 times of measurement. At 24 hours, TcB levels in thelow-BFF group (6.74 ± 1.76 mg/dl) was significantly higherthan the high-BFF group (5.31 ± 1.76 mg/dl, p < 0.001). At48 hours, TcB levels in the low-BFF group (10.95 ± 2.44 mg/dl) was significantly higher than the high-BFF group (8.19 ±2.40 mg/dl, p < 0.001) and at 72 hours, TcB levels in thelow-BFF group (13.34 ± 2.03 mg/dl) was significantly higherwhen compared with the high-BFF group (10.60 ± 2.48 mg/dl, p < 0.001) (Table 2).
With regards to re-admission rates for jaundice, 24% ofthe neonates were admitted to the hospital for jaundice during the first 2 weeks of life. The readmission rate for jaundiceduring the first 2 weeks of life in the low-BFF group (39.6%)was higher than the high-BFF group with statisticalsignificance (9.6%, p < 0.01) (Table 2).
Additionally, weight loss in the low-BFF group (178.54 ±47.26g) was significantly higher than the high-BFF group(108.42 ± 41.12g, p < 0.001). The frequency of defecation ofthe low-BFF group (3.82 ± 0.82 times/day) was significantlylower when compared with the high-BFF group (5.48 ± 0.83times/day, p < 0.001) (Table 2).
Table 2: Comparison of weight loss, frequency of defecation, bilirubin levels and re-admission rates for jaundiceduring the first two weeks of life between neonates in low-BFF group and high BFF group (n = 100)
The demographic data between the low and the high-BFFgroup had no statistical significance difference except BFF.According to recommendations from the American Academicof Pediatrics (AAP) and the American College of Obstetriciansand Gynecologists (ACOG)15 BFF should be at least eighttimes per day, as high BFF is associated with successfulbreastfeeding. The researcher used the lower limit of eighttime per day as the cut-off point. In the present study, thebilirubin levels and re-admission rates for jaundice werehigher in relation to decreasing BFF per day. The literaturereview showed that lower frequency of breastfeeding duringthe first 24 hours of life results in decreasing intestinalmovement, thereby reducing the excretion of bilirubin outsidethe body as stool output and increasing the intestinal bilirubinreabsorption into the blood. As a result, the unconjugatedbilirubin levels are high.2,5-6 In addition, breast milk containssubstances helping neonates to defecate. Lower frequency ofbreastfeeding during the first 24 hours of life diminishesstimulation from this substance.21 Thus, neonates in the lowfrequency of breastfeeding group also had significantly lowerfrequency of defecation per day. According to the study of Chen YJ, et al.,16 BFF during the early postpartum period hasan impact on the level of bilirubin and frequency of defecation.Thus, the bilirubin level and frequency of defecation per dayare significantly higher and lower, respectively, amongneonates who breastfeed less than eight times/ day. YamauchiY, et al.,19 found that infants who fed less than seven timesduring the first 24 hours had significantly decreased frequencyof meconium passage and increased incidence of severeneonatal jaundice (TcB ≥ 23.5) when compared to those whofed more frequently (22.8% vs. 7.7%). Another study byOkechukwu and Okolo 20 reported that lower frequency ofbreastfeeding per day was significantly correlated with higherserum bilirubin levels and lower passage of meconium duringthe first 24 hours of life.
Additionally, it has reported that frequency of breastfeedingduring the first 24 hours of life is related to lactogenesis.22Since the suckling of neonates sends a signal to the anteriorpituitary gland to release prolactin and oxytocin, and these arethe major hormones producing breast milk in the mammaryglands, this helps breast milk ejection from the mammaryglands.23 Lower BFF per day can reduce breast milk volumeand increase body weight loss. The decreased intake of breastmilk and greater weight loss plays an important role in impairing bilirubin clearance by the liver.10 For this reason, the neonatesin the low frequency of breastfeeding group had significantlyhigher levels of bilirubin and greater body weight loss thanthe neonates in the high frequency of breastfeeding group. TheAmerican Academic of Pediatrics and ACOG has also statedthat the frequency of breastfeeding during the first few weeksafter birth should be at least eight times per day. As appropriatefrequency of breastfeeding, at least eight times per day, helpsproduce sufficient breast milk and prevents high levels ofbilirubin from inadequate breastfeeding.15
Although the association of BFF and re-admission ratesfor jaundice during the first two weeks of life has not beenstudied previously, there is evidence that lower BFF iscorrelated with neonatal jaundice in the first few days of life.Ketsuwan, et al.,24 studied the relationship between BFF andneonatal jaundice during the first 48 hours after birth. Datawere collected on 116 neonates who either had or did not havejaundice at 48 hours after birth. The finding showed that thenumber of infants who breastfed < 8 times/day in the jaundicegroup was higher than that the number of neonates who fed
However, this study is a descriptive research in which theresearcher exerted no effort to control extraneous variables.Therefore, the researcher could not conclude definitively thatlower BFF alone leads to increased bilirubin levels andre-admission rates for neonatal jaundice since higher bilirubinlevels may involve other factors beyond lower BFF. Exploringother factors with potential impact on bilirubin levels andusing an experimental design to test the effects of BFF oninadequate breastfeeding jaundice needs to be considered infuture studies.
This study demonstrated that lower BFF < 8 times/dayincreases bilirubin levels and re-admission rates for jaundiceduring the first 14 days of life. These findings may help healthcare professionals in breastfeeding support as it provides aknowledge base for prevention of inadequate breastfeedingjaundice in neonates.
The author would like to thank all of the participants fortheir cooperation in this study. Deep gratitude also goes toRamathibodi School of Nursing, Faculty of MedicineRamathibodi Hospital, Mahidol University, Thailand for thegrant supporting this research.