A topic dermatitis (AD) is perhaps the most common inflammatory skin problem seen in clinics of pediatric allergy, pediatric dermatology and even general pediatric practices. In the International Study of Asthma and Allergy in Children (ISAAC), the prevalence of AD was estimated to occur in around 10% of the pediatric population worldwide1 including Thailand.2 Classically, AD starts early in life, commonly within the first 3-4 months of life.3 However, it is not uncommon for AD to develop during late childhood or even in adults. The term ‘atopic’ denotes a relationship with allergy, particularly with the type I - IgE-mediated mechanism. However, such relationship was found to occur in around 50% of AD cases.4 This may be an underestimated value since a prevalence study of food allergy among AD children seen in a dermatology clinic in Melbourne was found to be as high as 80%.5 In fact, patients with more severe AD was found to be more atopic than in mild AD cases.6 Common allergens found among AD patients are food allergens among younger children and house dust mites in older patients.7 This may relate to an increase in the ability of allergens to penetrate through inflamed skin more than through less damaged skin. Such relationship was confirmed in some AD cases with peanut allergy.8 For AD patients with allergy to aeroallergens such as to house dust mites, it is unclear whether mite allergens and others invade the immune system through respiratory mucosa or via inflamed skin.9 Since protease molecules are major components of dust mite allergens, it is possible that these proteases can up-regulate pro-inflammatory molecules such as damage-associated molecular pattern(DAMP).10These molecules could participate in the initiation and sustaining inflammation in AD skin.
The diagnosis of AD requires certain salient features of AD:11 1) itching mainly occurring nocturnally, 2) characteristic sites of rashes such as face, wrists, ankles among infancy; neck, antecubital fossa, popliteal fossa in early and late childhood and face, around forehead in adults, and 3) relationship with familial or personal occurrences of other atopic diseases such as allergic rhinitis and asthma. Identification of specific IgEs to common allergens (food allergens in infants and aeroallergens in older patients) through a skin prick test or by serology may be used to satisfy criteria #3. The severity of AD could be estimated by various validated clinical scores such as SCORAD-Severe Scoring for Atopic Dermatitis,12 and EASI score.13 The need to accurately document the severity scores is not only important for choosing an appropriate regimen of therapy but also for a follow up and for monitoring the effectiveness of the therapeutic regimen. Remission of AD can occur and has been formally perceived to be around half of the AD cases. However, a recent investigation indicated that this figure may be too high and up to 18% had AD symptoms relapsing every year.3 Major poor prognostic factors for persistence diseases are severity of symptoms and atopic sensitization.
In a large epidemiological scale study (International Study of Asthma and Allergic Disease in Children) conducted in Bangkok, Chiangmai, Khon Kaen and Songkla, the prevalence of atopic dermatitis was found to be around 10% of pediatric population both at 6-7 years old age group and at the 13-14 years old age group.2,14-16 Findings of these observations suggest that the more common infantile form of AD could be even greater than 10% since peak age of AD occurs within the first few years of life and goes into remission in half of the cases at age 5.5
AD is also commonly known as ‘eczema’. This accentuates a nonspecific inflammatory nature of AD and perhaps reflects a more diversified pathogenetic mechanism. Indeed, it was not until recently that the relationship between AD and food allergy was confirmed.17 Reluctance to embrace such association still prevails among dermatologists throughout the world. As indicated above, it is clear that up to 50% of AD patients are atopic and careful investigation among AD patients in a referral dermatology clinic in Melbourne established the frequency of allergy up to 80%.5 From this less than ideal percentage of association, it is clear that other factors participate in the generation of an atopic dermatitis flare. The mostly unique and invariable nature of skin of AD patients presents as dryness of skin although a varying degree of dryness was noted from case to case. In addition, dry skin is associated with a certain degree of itching which further leads into constant scratching. Itching in AD can be severe and very disruptive for sleep to both patients and their families. Some patients not only described itching as only ‘itch’ but also of pain of varying degree and characters (such as piercing, stabbing, burning, etc). Clearly, these sensations derive from stimulus to the C fiber nerve endings by a group of chemical mediators resulting from inflammation and/or increasing degree of their concentrations within the epidermis and to a certain extent within the underlying dermis. Inflammatory that have received recent attention for their association with itching include IL-31,18 TSLP (Thymic stimulating lymphopoietin)19 and other neuropeptides such as substance P and other proteases.20 Itching and severe scratching leads to skin trauma ensuing in further influxes of inflammatory cells and release of inflammatory cytokines together with invasion of surface bacteria particularly with Staphyloccus aereus.21,22 AD skin is susceptible to colonization with S aureus perhaps due its inherent defect in the production of antimicrobial proteins such beta-defensin and cathelicidin.23 Production of staphylococcal toxins particularly S enterotoxin A and B (which are super-antigens) leads to multiplication of inflammatory AD response and further worsening degree of flares.24 The inflammation of AD skin leads to deeper penetration of common allergens such as foods and dust mites to the underlying skin with more complex nature of immunological systems. Further release of cytokines such as IL-4 and IL-13 leads to amplification of allergic inflam- mation while IL-22 leads to further division of skin cells and keratinization of the skin.21 Taken together, the innate dryness of AD skin leads to itch/pain with skin scratching which culminates into acute inflammation with further influx of inflammatory cells, vasodilation, extravascular leakage, oozing and high degree of atopic responses.
With further refined knowledge on the skin barrier protein which acts as water retention in the structure of the skin, several researches were directed towards abnormalities of this group of proteins initially known as a group of ‘ceramides’. It is currently known that these agents represent wide varieties of related glycoproteins such as filaggrin, loricin, etc.21 These agents are produced in the basal cell layer of the epidermis and are transported and later become matured during their transportation to the Stratum corneum.25 In Stratum corneum, this skin barrier protein acts as ‘mortar’ to bridge dead superficially located cornified epithelial cell in Stratum corneum (bricks). With decreased amounts of these structurally immature proteins, skin loses its ability to retain hydration with increasing transepidermal water loss (TEWL) which has been estimated to be up to several folds compared to that of normal skin. As a result, skin in an AD patient became dry and ‘does not respond’ well to moisturizers, particularly those with lotion properties (designed to hold more liquid). Indeed, the defect of the filaggrin gene was demonstrated in certain numbers of AD patients25 which proves that skin barrier defect is a major factor that drives inflammation in AD in the first place. Such a defect leads to a drop in the production of filaggrin and related proteins which become further accentuated during the acute stages of AD (exacerbated with increasing infection and exposure to related allergens).
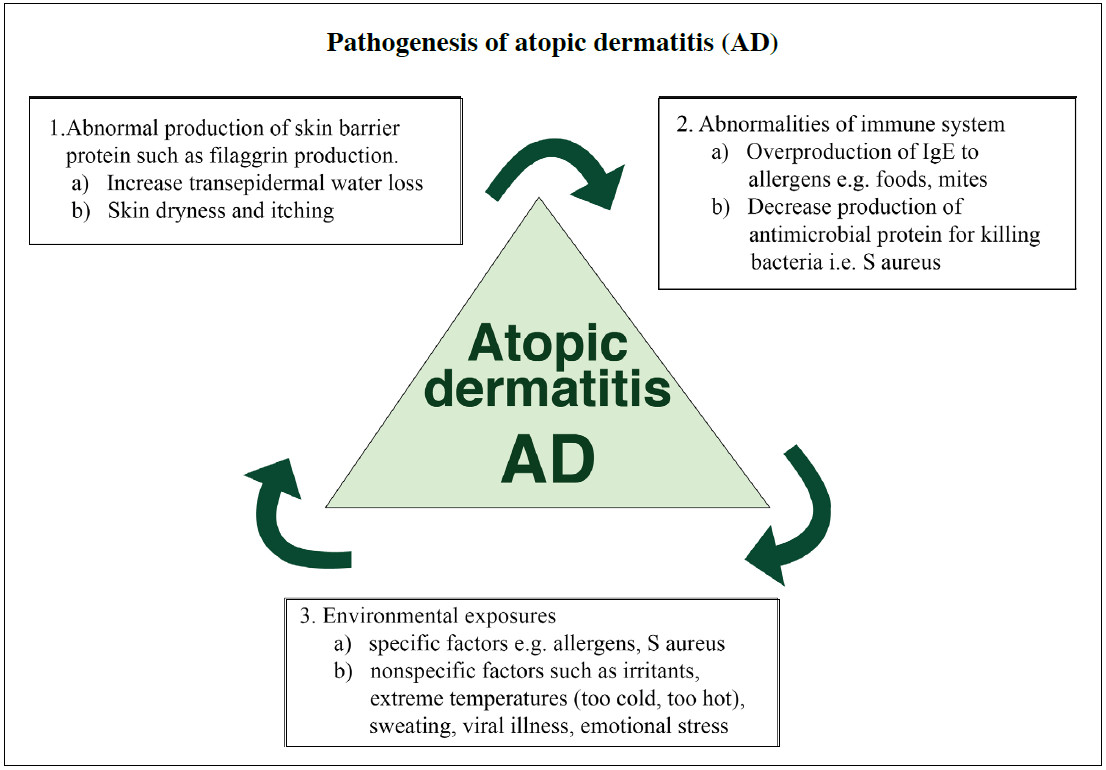
It can be clearly seen that skin barrier defects (perhaps due to genetic defects in skin barrier protein) leads to skin dryness and itching together with underlying immunological defects (IgE-mediated reaction to foods, aeroallergens and stimulation from super-antigens from staphylococcus) and exposure to inciting environmental factors (nonspecific factors such as sweating, irritant factors and specific factors, i.e., allergens) are interrelated factors in the pathogenesis of AD (Figure 2).
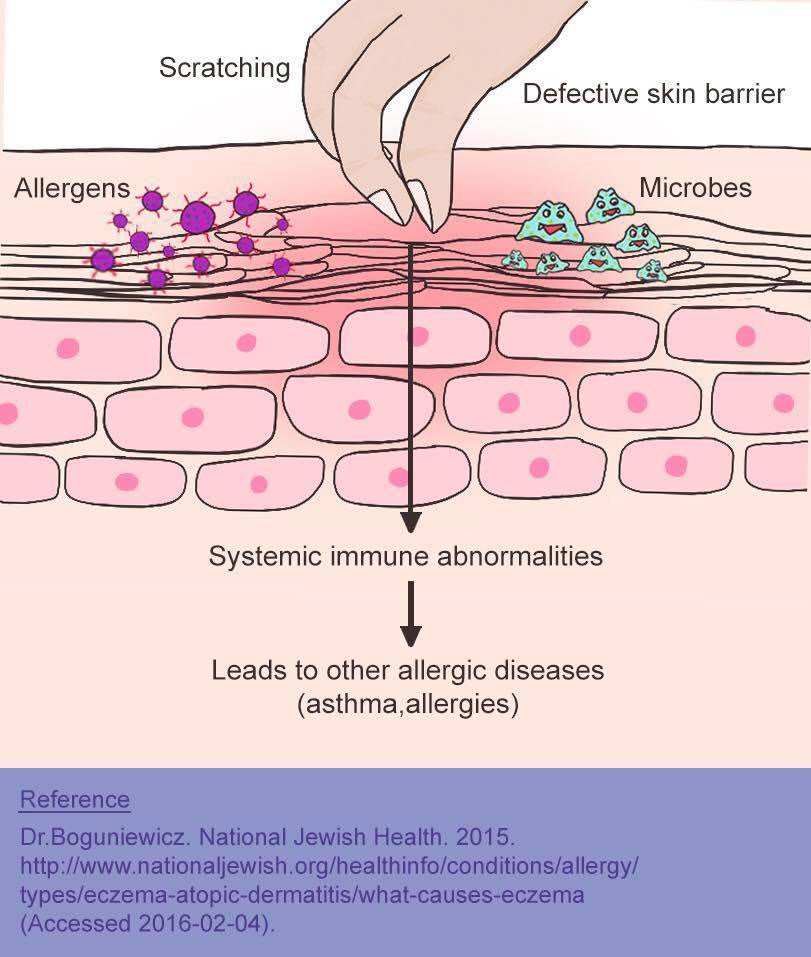
Figure 2: The dry-itch-scratch-inflammation cycle. Increase in transepidermal water loss leads to skin drying, scratching and absorption of microbes and allergens. These result in alteration of immunological response of the skin causing inflammation in AD.
As pathogenesis of atopic dermatitis is complex, treatment of atopic dermatitis involves multimodalities of treatment approach.7 Since the course of disease is chronic and requires continuing care, cooperation from patients and families is of paramount importance. In order to attain such cooperation, a basic and simplified knowledge of AD must be shared with the family prior to the start of the therapeutic regimen to ensure compliance. In most cases, the families have already seen several medical specialists and mostly rely on dermatological preparations (emollients and topical steroids) without proper knowledge of how and when to apply them. Few families had adequately basic knowledge of AD and had become very frustrated with treatment. Several families even had ‘steroid phobia’ and thus did not use this potent group of anti-inflammatory agents to its potential and therefore were not able to bring exacerbating AD to adequate control. A patient education program that is simple and yet comprehensive, requires a well thought-out program with proficient educators which could be either be doctors or specializing nurses.26 This is not an easy task to accomplish in busy dermatological and allergy practices and could be the reason for the failure to bring the disease under control. In general, patients and families should be given a simplified concept of the pathogenesis of the disease which forms the basis of treatment steps. These steps include:
Since the implementation of all of the above steps of treatment is required for a successful control of AD disease severity, most patients do not reach the step of ‘remission’ with just prescriptions of dermatological medications.7 Perhaps the most important step of treatment that has been commonly overlooked is the hydration of the skin. Since varieties of currently available emollients in the market are branded as ‘moisturizers (increasing hydration to the skin)’ and ‘humectants (absorbing water from the external ambience)’, reliance of adequate rehydration of the skin has been placed on frequent use of these ‘emollients’29-31 and increasing oral intake of water. As stated earlier, trans- epidermal water loss is very high in patients with AD and it would rather be impractical to hydrate the patients’ skin without directly hydrating the skin from the external surface. Such comprehensive skin hydration of the skin often requires administration of water to permit absorption of water through short-term occlusion of skin. Such an occlusion regimen is often termed ‘wet-wrap therapy (WWT)’ which has been described in the literature for more than 4 decades.32 However, debates on the efficacy and adverse effects of WWT have been intensive over the past 3 decades. Recently, the clear efficacy and lack of adverse effects of WWT has led to a rise in its popularity particularly among cases of moderate to severe AD.33 Remission can be brought under rapid control with WWT with high efficacy of itch control although direct comparison to a regimen without WWT is lacking. In the past, due to its complexity, WWT often required an initial period of in-hospital intensive therapy. However, due to an increasing availability of wrapping materials and methods, numbers of families could be adequately educated and the patients could go on to receive continuing and successful treatment as out-patients.34 In fact, out-patient daily wrap therapy can be applied to save cost of hospitalization and to allow parents to practice wrapping at home. The next section describes techniques of WWT that are currently employed at Siriraj Hospital and Samitivej Allergy Institute (SAI) in details in order to allow our readers to perceive a clear picture of how WWT is carried out.
Since a large amount of hydration is continuingly lost throughout the day from inflamed skin in moderate-to- severe atopic dermatitis, oral replenishment of these fluids through oral route is not realistic since most of fluid will be loss through gastrointestinal and renal routes before reaching the targeted inflamed skin. The most commonly used hydration techniques that are frequently sought after are via the use of emollients (or moisturizers) which is a large group of dermatological preparations with diverse properties.These properties are designed to preserve hydration of the skin e.g. moisturization (directly apply fluid to the skin as a component of the agent-in the form of lotion), occlusive (to prevent further evaporation of fluid from the skin (in the form of ointment such as petrolatum), humectant (absorbing fluid from the ambient, e.g, urea and lactic acid), anti-inflammatory (tar and newly synthesized components), etc. It would be ideal to produce a filaggrin-like substance for such purpose but this is not achievable on a wide commercial basis for the time-being. For readers who are interested in this area, recent reviews on this topic are recommended for further reading.29,30 With the increasing complex nature of current moisturizers, the cost of these once inexpensive agents is becoming higher and therefore are not readily affordable for use on a wide area of skin in severe atopic dermatitis. In fact, head-to-head comparison of these various moisturizers, particularly on a long-term basis is lacking.30 Petrolatum, as an inexpensive ‘inert’ occlusive moisturizer, was recently found to be associated with increasing amount of antimicrobial peptide in the skin with the upregulation of innate immune genes such as IL-6, IL-8 and IL-1 beta.31 With the abovementioned shortcomings, the premise to directly hydrate skin via bath and wrapping has received much attention and acceptance through the past two decades. Such a treatment modality has been applied in various forms such as bathing in sea water and in highly concentrated salt solution such as in the Dead Sea area.35 Hospital/home intensive hydration therapy often requires tub bathing twice daily followed by rapid toweling and application of emollients and topical inflammatory agents. Such bathing requires a bath tub which is not readily available among homes in Asia. Moreover, bathing young children in small tubs for a long period of time is not an easy task and there is a risk of drowning if babies left unattended in the tubs. With these difficulties, wet wrap therapy (WWT) is designed and intended to replace prolonged bathing. WWT with an application of topical anti-inflammatory lotion also allows prolonged absorption of these medications and thus enhances its activity to bring about more rapid remission of the disease.34 As indicated earlier, initial WWT required hospitalization and intensive nursing care and expertise. This made WWT a less than ideal treatment to be prescribed by most physicians. The techniques of WWT continued to evolve over the years. Despite the fact that WWT has been implemented at Siriraj Hospital for quite some time, our group continued to improve the technique of WWT to be more simple and applicable to a busy dermatology and allergy practice. The following paragraphs detail the technique of WWT currently being use at Siriraj Hospital and Samitivej Allergy Institute (SAI).
Prior to WWT, the skin is cleansed for 10 minutes with a mild wash lotion, most preferably with non-irritative ingredients (currently available in various formulas).

Figure 3: Pictures of an AD patients wet wrap therapy (WWT) (3A) prior to WWT (3B) during and (3C) after one day of WWT – with permission from the family.
Parents are advised to avoid scrubbing since this will lead to more abrasion of the delicate AD skin. The skin is then blotted dry by cotton towel and proceed onto saline WWT. For intensely inflamed skin, topical corticosteroids of appropriate potency is applied prior to WWT.34 The readers are also referred to the rationale selection of topical corticosteroids for various stages and sites of skin involvement in AD.7
The preparation of saline solution can be conveniently made by mixing a ratio of 1 teaspoon of clean salt (10gm) to a 1 litre of clean tap water at room temperature. Wrapping materials are then soaked in salt water thoroughly before applying to the skin. Commercial wrapping materials are available in Europe and in the US. These are made of stretchable tightly fitted cotton tubes which come in varying sizes to fit various parts of the body. They are quite easy to use, can be worn throughout the night and are reusable to certain periods of wrapping (up to 20 wraps). Unfortunately, these items are not available in Thailand at the time of writing which has led our group to design our wrapping techniques using widely available orthopedic and surgical dressings. The advantage of our WWT technique is that adjusted rolling of the dressings over various body sites can be individually performed to meet the patients’ level of comfort and for degree of hydration required. Additional hydration can be applied by spraying saline solution directly on WWT materials. Materials used for 2-3 layers of dressing are (also illustrated in Figure 3):
The undercast cotton roll is ideal for absorbing and retaining large amounts of salt water to come in contact with the skin. Stretchable bandage rolls and net dressing holds the undercast rolls in place (may apply together or as a single holding layer). Additional salt water can be directly sprayed through these holding dressings through to the undercast roll making adequate hydration assured for each individual patient. The duration of WWT is variable and is subject to a supervising physician’s discretion. In general, WWT is left in place for at least 2-3 hours. In severe cases, whole day wrapping can be done with a careful monitoring of body temperature of the patient.34 An aseptic technique during WWT should be strictly followed during the wrapping. In general, AD rash worsens in extreme temperatures (hot in tropical climate and cold in temperate climate). Perhaps, the setting of a room temperature at 23-25ºC is recommended. Figure 4 shows a moderate-severe AD skin prior to wrapping, during WWT and after one day of WWT. The choice of salt water vs tap water is subject to institutional preferences and has not been intensively compared.32,33 As indicated earlier, the use of hypertonic salt bath35 and electrolyte-containing solution has been reported to promote rapid healing of inflamed AD skin.36 The mechanism for water and salt to promote healing of the skin is currently unclear but perhaps involve the alleviation of itching/ scratching and reduction of activation of inflammatory cells at the active AD site. Moreover, a recent report from Korea demonstrated that WWT promoted the production of lamella body with the release of lamella contents in the skin undergoing WWT.36 The release of lamella content is associated with increased skin hydration. In that study, skin hydration was maintained for 1 week after discon- tinuation of WWT.
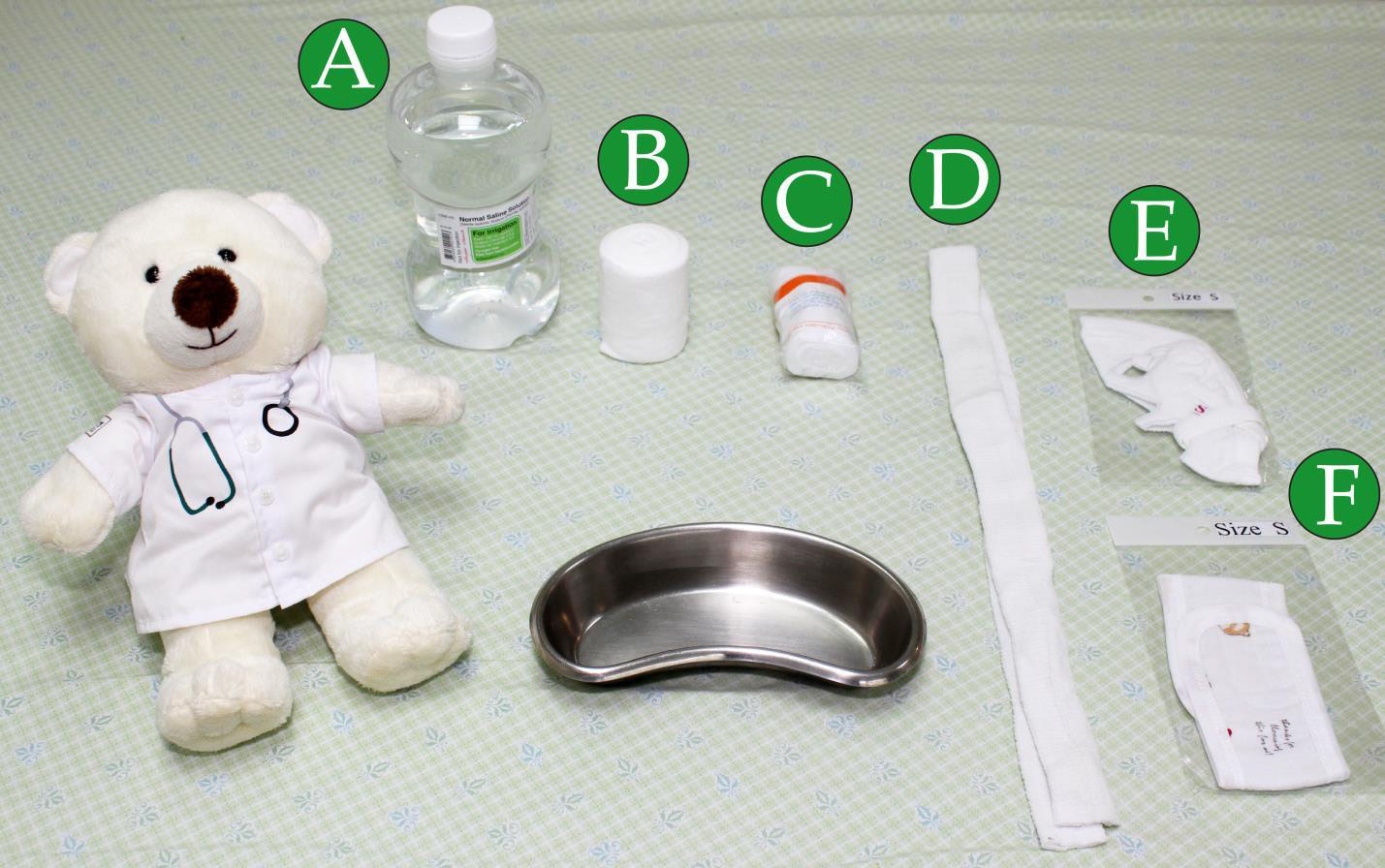
Figure 4: Materials for use in performing WWT. These include (A) Saline (B) Undercast cotton roll (C) Stretchable bandage roll (D) Tubular stretchable net dressing (E) the Duangnetr’s mask (F) hydration arm sleeves
Recently, our group have devised an innovative AD mask using cotton fiber and overcloth stitched together with Velcro wrapping to hold the mask in place – i.e., the Duangnetr’s AD mask (Figure 4). This allows WWT to be done to the facial area, particularly to the cheek and chin areas with relative ease and thus avoiding thick wrapping around this vital area and therefore permitting free movement of head and decreasing patient’s apprehension. Surprisingly, similar efforts in hydrating facial area with a mask in a small number of AD patients was reported to reiterate the need for a new device for hydrating this delicate and sensitive part of the body.37
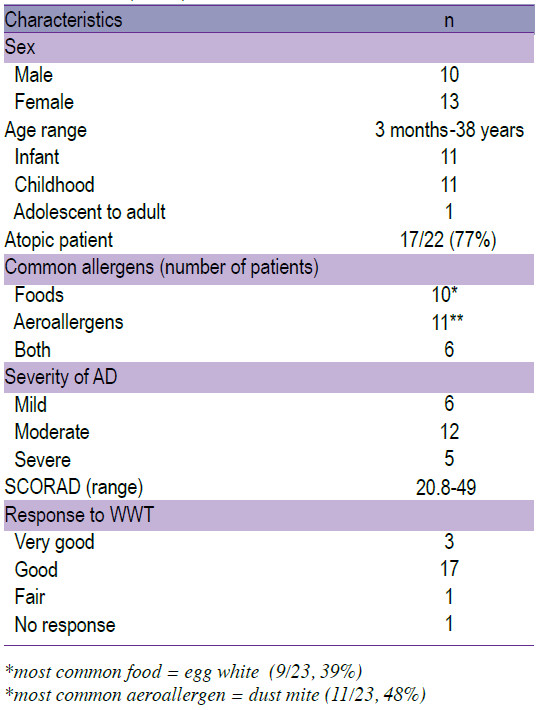
WWT has been used in the Department of Pediatrics, Faculty of Medicine Siriraj Hospital for more than 20 years. The techniques have been further refined and continue to be fine-tuned to achieve optimal efficacy and patient comfort. The Duangnetr’s mask is an example of our continuing improvement of such techniques. More- over, the technique is taught to the parents and caregivers during the period of hospitalization (usually a short-term admission). Within the past year, WWT has been applied and further fine-tuned at Samitivej Allergy Institute (SAI) in a team-based fashion. The therapy is initiated as out-patient with instructions given to the families and the patients are followed up in a visit within a few days to monitor the progress. Twenty three patients were successfully treated in this fashion with only 2 patients required for further in-hospital therapy (see Table 1). These patients included infants, children and even some adults. Most of these patients were quite atopic to foods or dust mites (see Table 1). Most patients responded within a few days post-WWT treatment and required intermittent WWT, thereafter. The length of WWT as a long term therapy for AD to maintain remission has not been adequately studied.
Table 1 : Characteristics of AD patients who underwent WWT at SAI in 2015 (n =23).
Atopic dermatitis is a common allergic skin condition caused by a complex pathogenetic mechanism. Despite the term ‘atopic’, not all AD patients are allergic to allergens. Common allergens found associating with AD were foods (for infants) and house dust mites (older children, with adolescent and adults). Recently, abnormalities of skin-barrier proteins were demonstrated in patients with AD. Such abnormalities lead to increase transepidermal water loss, itching/scratching, skin infection, increase absorption of allergens and finally increasing inflammation of the skin. In this review, we discuss a multimodalities approach needed to bring about a successful treatment of exacerbated inflamed areas. In particular, the article describes the role and importance of comprehensive skin hydration using WWT. Techniques for WWT are discussed more fully. A description of the innovative Duangnetr’s AD mask is given. WWT, together with proper patients’ education, the use of moisturizers and topical anti-inflam-matory agents, is an integral part of treatment for severe AD to bring about a rapid remission and for a long-term control of AD.