Hypertension is a major risk factor for coronary heart dis- ease and stroke. Globally, hypertension is the leading non- communicable diseases (NCDs) risk factor that accounted for 13% of global deaths, followed by tobacco use (9%), raised blood glucose (6%), physical inactivity (6%), being overweight and obesity (5%).In the South-East Asia Region, where cardiovascular diseases alone accounted for 25% of all deaths, hypertension presents in approximately 35% of the adult population and accounted for nearly 1.5 million deaths or 9.4% of all deaths annually.1 For the survivors, there is a high burden of chronic care as patients become dependent on care as a result of the effects arising from cardiovascular complications.
Many hypertension management guidelines have been devel- oped and revised. All guidelines emphasize the need to consider blood pressure levels and the associated clinical profiles. These include the presence of cardiovascular risk factors to other related diseases and evidence of both clinical and sub-clinical end organs involvement. These have given us better rational management of arterial hypertension aimed to reduce future complications and disease burden as much as possible.2-8
The Hypertension Registry at the Bangkok Hospital Medical Center started up in June 2012. We have previ- ously reported on the first 7 months of 647 registry cases in the Bangkok Medical Journal of February 2013.9 The registry has been continued and regularly audited every 6 months. The primary goals of the Hypertension Registry are: (i) to create data as a tool for quality control (QC) for improving future quality services and planning, (ii) to create public awareness particularly among patients with hypertension and among clinical providers regarding other associated medical conditions that are potential risk factors beyond blood pressure levels, (iii) to utilize electronic medical records (EMR) to improve hypertensive care, and (iv) to optimize service efficiency and continuing education of clinical staff and physicians by creating feedback data reports. The intent of this article is to review and highlight the Hypertension Registry profile after 2 years of operation.
New patients with hypertension are being recruited to the Registry. The recruitment and registration process has been described previously.9 The majority of new registrants were enrolled from the Hypertension Clinic. The registry data were audited every 6 months in order to update new data input. Cases who had failed to follow up for more than 12 months after the first registration were discharged from the Hypertensive Registry program. The characteristics of the updated registrants were compared to the registrants of the first 7 months.
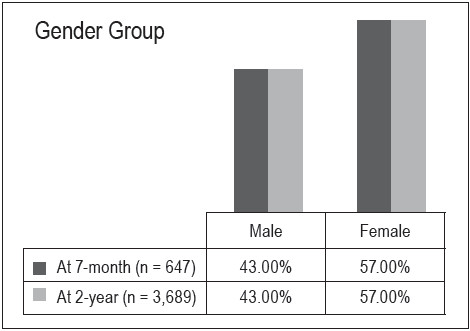
There were more female cases than male (57% vs. 43 %) and this matches the same proportion as reported after the first 7 months of the Hypertension Registry (Figure 1). The most common age group (between 51 to 80 years old) comprised 69.6% of the registrants compared to 86.7 % in the previous report. There were also registrants aged less than 21 years, and this age group had not been represented in the previous report at 7 months after the Registry started up (Figure 2). More than half of the registrants had excess body weight (BMI > 25 kg/m2) i.e. 57.8% of the registrants at the end of second year compared to 52.9% of the first 7 months registrants(Figure 3).
![]()
![]() Figures 1: Comparing gender distribution of the hypertension registry cases at the first 7 months and at the end of 2 years.
Figures 1: Comparing gender distribution of the hypertension registry cases at the first 7 months and at the end of 2 years.
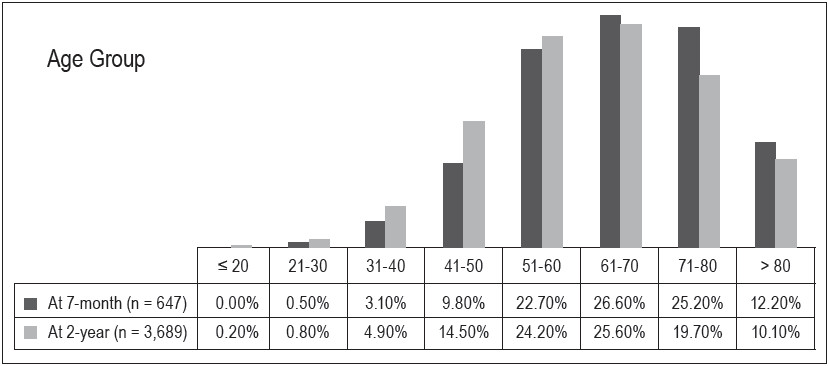
![]() Figures 2: Comparing age distribution of hypertension registrants after 2 years compared to first 7 months.
Figures 2: Comparing age distribution of hypertension registrants after 2 years compared to first 7 months.
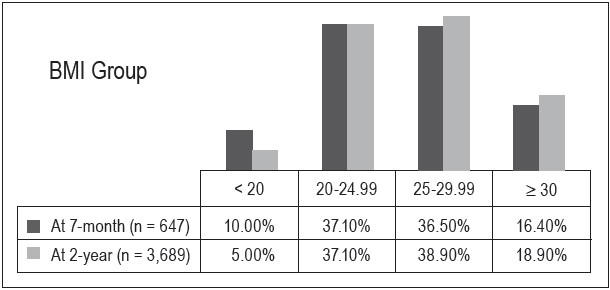
Figures 3: Body mass index distribution of hypertension registrants.
Dyslipidemia (57.8% of the registrants) was still the most common associated cardiovascular risk factor followed by diabetes mellitus (DM) (29.7%), heart disease (4.0%) and kidney diseases (3.0%) which all exceed stroke (2.7%). The comparative prevalence of cardiovascular risk factors between this 2 years’ summary and the first 7 months of registry is demonstrated in Table 1. A plain film of chest x-ray was ordered more often than EKG (26.0% vs. 22.9%) which was reversed compared to the first 7 months report. A vascular assessment (ankle-brachial index (ABI) and cardio-ankle vascular index (CAVI) by machine model VS-1500N, Fukuda Denshi) was performed in 16.7% of patients. The urine microalbumin/creatinine ratio (UACR) test,an easy test in detecting early renalab normality, was ordered in a higher percentage of cases compared to those reported on after the first 7 months of the Registry had started (22.4% vs. 18.1%) (Table 2).
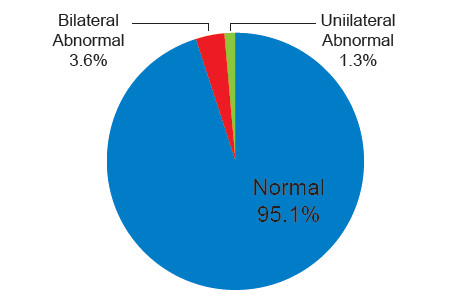
From the EKG reports,3.1% of cases were found to develop left ventricular hypertrophy(LVH) and 68.5 % showed a normal study. According to chest x-ray, LVH, left ventricular enlargement (LVE) was reported in 0.9% of cases, cardiomegaly in 20.1% of cases. CAVI were normal in 61.2% of cases, unilaterally abnormal in 9.5%, bilaterally abnormal in 29.2%. These were very different from ABI’s results which displayed normal in 95.1% of cases, unilaterally abnormal in 3.6%, and bilaterally abnormal in 1.3%. There was no protein detected in urine analysis in 69.9% of cases, micro- albuminuria (UACR 30-300 mg/gm) in 23.1% and macro- albuminuria (UARC > 300 mg/gm) in 7.0% (Figure 4-8).
Table 1: Associated risk factors
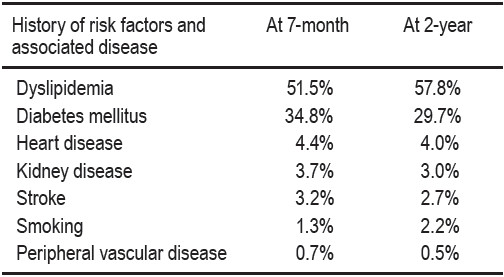
Table 2: Investigations ordered for the hypertension registrants.
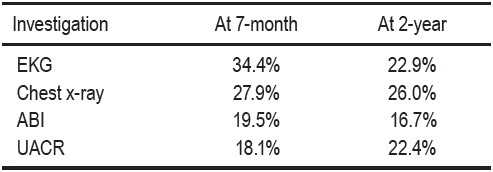
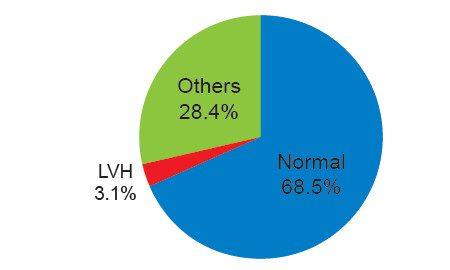
Figures 4: EKG findings (n = 848, 22.9% of total registrants)
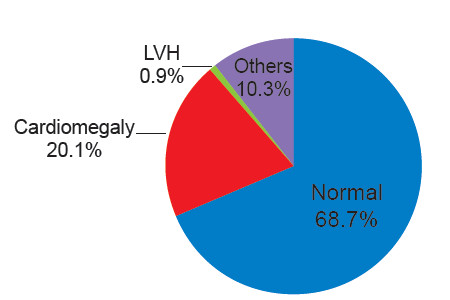
Figures 5: Chest X-ray findings (n = 962, 26% of registrants)
Figures 6: CAVI measurement for vascular stiffness assessment (n = 619, 16.7% of registrants)
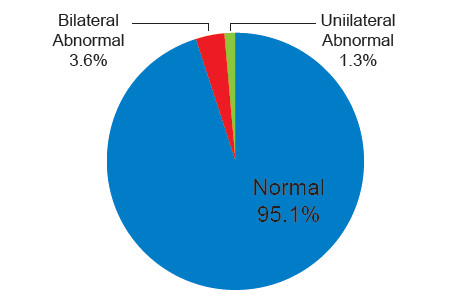
Figures 7: ABI measurement (16.7% of whole registrants)
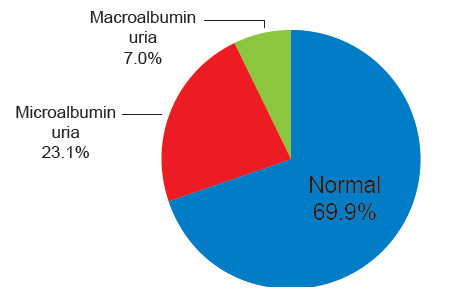
Figures 8: Results of urine microalbumin/creatinine ratio (UACR) (n = 830 cases, 22.4% of registrants)
With more registrants, a greater percentage of hyper- tension patients not taking any medications was discovered (18.2% vs. 3.9%). Those who did take 4 or more medications also presented in higher percentage terms (13.1% vs. 2.2%) when compared to data from the first 7 months report and 3.1% of registrants were using more than 4 medications (Table 3).Similar to the last report,angiotensin receptor blocker(ARB) was the commonest medication used at a lower percentage (29.1% vs. 35.6%), followed by dihydro- pyridine calcium channel blocker (CCB) in 28.2% and beta blocker in 17.0% (Table 4).
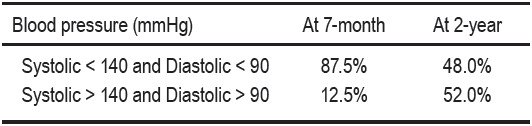
In terms of blood pressure (BP) control, 48% of the registrants were able to achieve BP under 140/90 mmHg. This percentage was much lower than at the time of reporting after the first 7 months. This updated figure probably indicates a more realistic picture now that we are gathering data from a larger sample of registrants and given the greater number of physicians providing hyper- tensive care. (Table 5)
Table 3: Number of antihypertensive medication use.
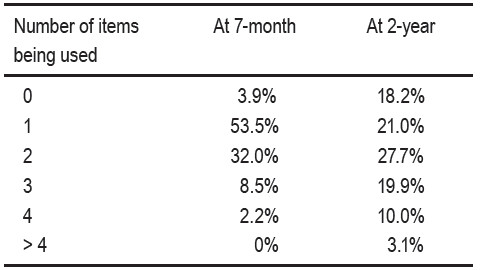
Table 4: Group of antihypertensive medications use.
ARB = angio tensin receptor blocker
CCB = calcium channel blocker
ACE = angiotensin-converting enzyme
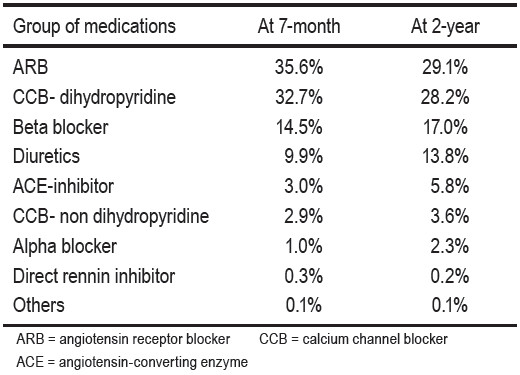
Table 5: Blood pressure goal achievement.
The Hypertension Registry has provided information that is useful for improvement plans to hypertension services by advocating for lifestyle changes and multi- dimensional management. More than half of registrants with hypertension were overweight and 18.9% met the criteria of obesity (BMI > 30 kg/m2). This percentage was higher than that noted after the first 7 months of the Hyper- tension Registry (16.4%). Measurement of the abdominal circumference, to identify abdominal obesity, another risk factor influencing prognosis in hypertension cases,6,7 should be added as a later step. Although dyslipidemia was the most common associated risk factor (57.8% of the regis- trants), the prevalence was not so different from that seen in the general population. The prevalence of DM in our hypertension registry (29.7%) showed a higher percentage than that seen in the general Thai population (< 10%).10 Buranakitjaroen P11 also reported a higher prevalence of DM (35%) in Thai hypertension patients from the out-patient clinical practice based on 2007 data.
In comparison, the number of patients presenting with a history of risk factors and associated diseases has increased from those reported at 7 months and 24 months. The statistical data on dyslipidemia, diabetes mellitus, heart, kidney diseases, stroke and peripheral vascular disease are not significantly different but in contrast the rate of smoking as a cause of hypertension increased significantly. Although smoking cessation by lifestyle changes was only suggested in the management of some hypertension guidelines4,7 and not suggested in other guidelines,3,6 we feel it should always be placed as another item in the lifestyle changes recommendation list to emphasize the importance of smoking cessation given that smoking is a major risk factor for atherosclerotic cardiovascular diseases.
For investigations, EKG was the second most ordered after chest x-ray. Left ventricular hypertrophy was reported in 3.1% of those who had an EKG report. In a community physician network hypertension registry of 710 African Americans in 2005, 37% of patients achieved the goal of blood pressure control, the left ventricular hypertrophy was reported as 8%12 comparable to our registry where blood pressure goal achievement was 48%. It is interesting also that LVH or LVE were reported only in 0.9% of those who had a chest x-ray done and cardiomegaly was as high as 20.1% by chest x-ray, although no specific guidelines recommended its use for cardiac findings found in chest x-ray as a criterion of asymptomatic organ damage detected in EKG.
For the vascular quality assessment, the model VS-1500N (Fukuda Denshi) was used and it yielded ABI and CAVI. The CAVI was reported as a parameter of arterial stiffness that was less affected by systolic blood pressure than carotid-femoral pulse wave velocity and demonstrated good reproducibility.13 There were relation- ships between CAVI and carotid intima-media thickness.14,15 The CAVI values were significantly higher in patients with reduced LV diastolic function than those with normal LV diastolic function and in metabolic syndrome patients than in non-metabolic syndrome patients.16,17 Arterial stiffness measured by CAVI also yielded better predic- tions for coronary artery diseases.18,19 In our registry the abnormalities revealed by CAVI were more commonly detected using ABI alone. Normal ABI values were found in 95.1% while only 61.2% of CAVI values were normal in the cases that had vascular measurements done. This observation might be useful to convince patients to comply with treatment adherence to potentially reverse vascular stiffness if managed well in the earlier stages of hypertension.20,17 In 325 obese Japanese, weight-reduction therapy through diet and exercise over a 3-month period significantly decreased CAVI values in parallel with an increase of adiponectin.17
Screening for albuminuria is recommended in all hypertensive patients4-7, 21,22 due to its benefit of cardio- vascular events prediction beyond its signaling of early kidney problems.23-28 In this registry, only 22.4% of registrants had the spot urine sample tested for albu- minuria and results showed 69.9% with no albuminuria, 23.1% with microalbuminuria (UACR 30-300 mg/gm) and 7.0 % with macroalbuminuria (UACR > 300 mg/gm). The prevalence of albuminuria was cited to be from less than 10% to more than 50% in hypertensive cases.29-33 Prujim et al.31 reported the prevalence of microalbuminuria was found in 5% of cases with no diabetes and hypertension, 20% with either condition, and 41% with both conditions. The presence of albuminuria should be another tool to alert hypertensive patients to be more concerned about effective hypertension management adherence and achieving blood pressure goals. Given this information, more cases of urine microalbumin screening will be recommended at the hypertension clinic service.
Diuretics, beta-blockers, calcium antagonists, angio- tensin-converting enzyme (ACE) inhibitors and angio- tensin receptor blockers (ARB) are recommended for ini- tiation and maintenance of hypertension treatment. Other groups of anti-hypertensive medications such as central acting agents, alpha blocker etc may be used alone or in combination for specific conditions. Combination therapy of drugs from different classes was found to be more effective than doubling the dose of one drug and may reduce the risk of treatment discontinuation especially with the single-pill combination.34-36 In this registry, most of the registrants were using 2 medications (27.7%) followed by those who used 1 medication (21.0%) and 3 medications (19.9%). Approximately 18.2% of registrants did not use anti-hypertensive medication,10.0% were taking 4 medi-cations and 3.1% were taking more than 4 medications. ARB was the most common group of anti-hypertensive medications prescribed by physicians and it was the same group prescribed at the first 7 months report.
The controlled rate of hypertension (SBP < 140 and DBP < 90) in this registry was achieved in only 48% of the registrants. This percentage is likely to be more repre- sentative of the true picture as it was drawn from a higher number of registrants when compared to findings from the first 7 months report of 87.5%. This challenges the care provider team to aim for a higher rate of success.
Hypertension Registry in the Future
The hypertension registry provides wider information beyond individual case treatment in hypertension clinics and should still be continued. Seminars to raise awareness of the benefits of healthy lifestyle changes and the importance of hypertension treatment were held usually on a Sunday afternoon in a relaxed atmosphere, once every 4 months or so. The team has touched on “diet approach to stop hypertension”, “weight management”, “exercise guide”, “mental health care” and “antihypertensive drugs” in the past seminars and found that these were good learning opportunities for both the staffs’ team and those attending which included hypertension patients, their relatives and friends.
The hypertensive registry after 2 years of experience provides us with more information than at the 7 months juncture. Interesting findings include the comparison of the history of risk factors and associated diseases to the previous study after the first 7 months the Registry was in operation, as after 2 years, the number of patients increased 4 times. Yet, there are no significant changes to the levels recorded of underlying dyslipidemia, diabetes mellitus, cardiovascular, kidney and stroke conditions. In contrast, however, smoking as a cause has increased significantly. We have to be aware of and emphasize the hazards of smoking to hypertension patients.
I would like to thank Mrs. Suchanya Sukhopuet and Mrs. Jitraporn Khankam, who heads the Department of Medicine, Mrs. Naphat Benjakhunprasit and Mrs. Puncharat Kiratikornpisut the nurse coordinators who, beside their routine work and patient outreach education, have put much effort into continuing the hypertension registry. I would like to thank also Mr. Puttipong Sawatasuk and Mr. Pornchai Tantivanon who helped build links from routine service data to informative data and finally, thanks to the support received from the information technology team.