Odontoma is a calcifying benign tumor composed of various dental tissues such as enamel, dentin, cementum, and pulp and representing the second most common odontogenic tumor of the jaw bones.1 They present with a similar gender distribution.2-7 Usually these tumors are asymptomatic, but are often discovered as a cause of retention of a primary tooth or impaction of a permanent tooth. The cause of odontoma is still unknown. According to WHO’s histological classification of tumors of the oral cavity and oropharynx, there are two recognized histological types: compound odontoma and complex odontoma.8 Compound odontoma appears as numerous, sometimes hundreds of small teeth while complex odontoma appears as a single amor- phous mass enclosed in a fibrous capsule. Compound odontoma is diagnosed more commonly in the first or second decade but the complex odontoma may be seen later in life.2-5,9,10 The most common location of compound odontoma is the anterior region of the maxilla. However, complex odontomas are frequently found in the posterior region of the mandible.2,3,11 The impacted tooth involving compound odontoma is usually the maxillary incisor or canine while complex odontoma usually involves an unerupted molar.2,3 Generally, the involved teeth are permanent teeth while a few deciduous teeth have also been reported.6,12-14 Nevertheless, odontomas have been reported to be linked to missing or super-numerary teeth.6
A radiograph plays an important part in the discovery of odontoma and is usually the diagnostic tool of choice for the odontoma. This tumor is more often seen as an incidental radiographic finding with atypical appearance. The radiographic characteristic is a uniform opaque mass situated adjacent to the crown of an unerupted tooth with a radiolucent line of uniform width surrounding the mass, separating it from the normal adja- cent bone.15 The differential diagnosis of complex and compound odontoma is that the radiographic appearance of compound odon- toma is tooth-like structures of varying number, size and shape whereas complex odontoma appears as a calcified mass with tooth structure radiodensity. However, an immature odontoma which shows up as a pale radiolucent area containing small foci of radiopaque materials with a well-defined margin may be difficult to diagnose radiographically.6
Microscopic features of complex odontoma contain all mature elements of dental structure: dentin, dentinoid, enamel, enamel matrix, pulp tissue and cementum. These are laid down in a bizarre and haphazard fashion, and there is no semblance of normal tooth arrangement. The mass of hard dental structure is surrounded by a connective- tissue capsule which could be linked to the periodontal membrane of an unerupted tooth.4,5 Immature odontomas have little hard tissue formation, consisting of weak pulp tissues, dentin, and enamel matrix.6 Treatment of the lesion can involve a simple local excision or enucleation, with no recurrence of odontoma reported after a follow- up of 1 to 15 years.2 Hisatomi M et al.6 reported of two cases of untreated odontomas that did not change the location, size, or radiographic findings during the follow-up period (from 14 to 21 years old and from 11 to 15 years old). However, these odontomas were not associated with the impacted teeth. They also found that after the removal of the odontomas that had interfered with tooth eruption, the unerupted teeth tended to erupt, although some teeth showed malposition.6
In this report, a case of very large complex odontoma located in the area of the left maxillary molar is presented.


Figure 1: A 16-year-old female showed no extraoral swelling. The overlying skin appeared normal.

Figure 2: Bone expansion of the left posterior maxilla from the second premolar to tuberosity was detected, at both the buccal and palatal side. The upper left second and third molars were absent. The overlying gingiva and other teeth in the affected region appeared normal.
The panoramic radiograph revealed a unilocular homo- genous radiopaque lesion with a well-defined margin and a radiolucent rim involving the left maxillary second premolar to the tuberosity. The lesion occupied the alveolar crest and extended to maxillary sinus. The left maxillary second molar was displaced superiorly into the sinus and the left maxillary third molar was not detect- able (Figure 3). The periapical radiograph showed a radiopaque lesion with well-defined margin surrounded by a radiolucent rim. The left maxillary second premolar had an intact lamina dura and normal PDL space without evidence of root resorption. However, the root of the left maxillary first molar could not be detected (Figure 4).
The cone beam computed tomography (CT) images of coronal and axial planes, demonstrated a well-defined radiopaque mass, homogenous opacity, sized 3.0x3.0x3.5 cm3, extending from the apex of the left maxillary second premolar to the tuberosity. This mass involved alveolar bone crest and elevated the floor of the left maxillary sinus. The left maxillary second molar was displaced above the mass to be near the orbital floor. The evidence of buccal cortex expansion with a slight deviation of the lateral nasal wall was shown. The lesion was surrounded by a radiolucent line (Figure 5).

Figure 3: Panoramic radiograph showed a well-defined, unilocular homogenous radiopaque lesion, surrounded by thin radiolucent rim. The lesion extended from the left maxillary second premolar to the tuberosity and from the alveolar crest to the left maxillary sinus The root of maxillary first molar seemed to be involved. The maxillary second molar was displaced nearly to floor of orbit. The left maxillary third molar could not be detected.

Figure 4: The periapical radiograph showed a radiopaque lesion with a well-defined margin and a thin radiolucent rim. The root of the left maxillary second premolar had no resorption with a normal lamina dura and PDL space. However, the root of the left maxillary first molar could not be detected.
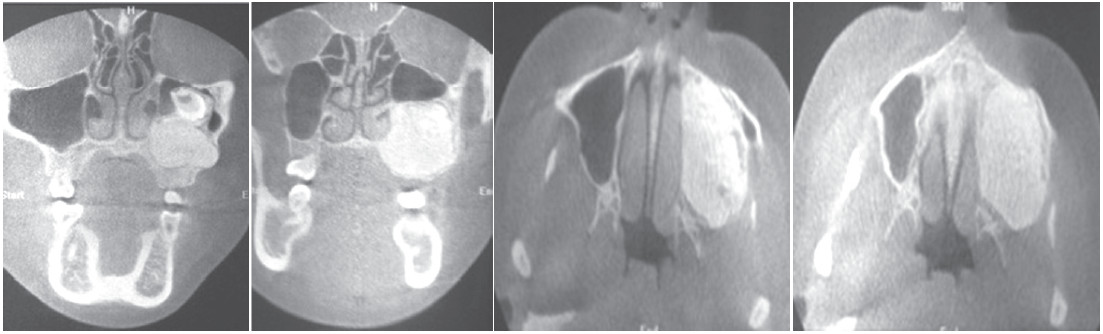
Figure 5: Coronal and axial dental computed tomography showed a well-defined, homogenous radiopaque mass, measuring 3.0x3.0x3.5 cm3 inside the left maxillary alveolar process. The floor of the left maxillary sinus was elevated and the maxillary second molar was displaced superiorly. The mass expanded antero-posteriorly and bucco-palatally, causing a slight deviation of the left lateral nasal wall and perforation of the buccal alveolar bone plate.
An incisional biopsy was performed under local anesthesia, by approaching at the buccal site, starting from the distal of the left maxillary first molar. After the muco-periosteal flap was reflected, the egg-shelled buccal plate was seen and then removed. The thin fibrous capsule covering a whitish-yellow hard mass resembling mature odontogenic tissues was discovered. This abnormal calcified mass was picked up by using a trephine bur (Figure 6).
Microscopically, of all the sections showed a conglo- merate of tooth structures as dentin, cementum and enamel matrix haphazardly arranged in a normal anatomical orien- tation (Figure 7). The diagnosis was complex odontoma.
Thus the patient underwent surgical removal of the lesion under general anesthesia. Access to the mass was achieved via intraoral approach. After the mucoperiosteal flap was raised from the left second premolar area to the left tuberosity, the thin overlying bone was easily visualized and removed (Figure 8). A window was created from the anterior wall of the left maxillary sinus at a level above the root apices of the left maxillary first molar and second premolar. Surrounding bone was removed to further expose the calcified mass. Then the capsule overlying the odontoma was removed (Figure 9). Sectioning of the odontoma was performed with a fissure surgical bur under continuous saline irrigation and chisel to split it. The large lesion was divided to multiple small pieces. All of the odontoma was completely removed, together with the displaced left maxillary secondary molar (Figure 10). After the lesion was removed, it was found that the left maxillary sinus was perforated. The entire remaining capsule was removed by curette, and the sharp bony edge was smoothened. The operative site was then irrigated with normal saline solution. In order to obtain hemostasis, a surgical suture was applied. The mucoperiosteal flap was repositioned and the soft tissue was closed by primary intention with an interrupted 3-0 resorbable suture.
Postoperative recovery was satisfactory, without development of oroantral fistula. The patient had no sign of sinusitis. She had no pain or abnormality in the affected area over a 3 year follow-up period. Radio- graphic examination at 1 and 3 year after odontoma removal did not reveal any signs of recurrence (Figure 11). However, a periapical radiograph taken 3 years after the operation showed that the affected first molar had pulpal obliteration, a short root and showed loss of lamina dura.
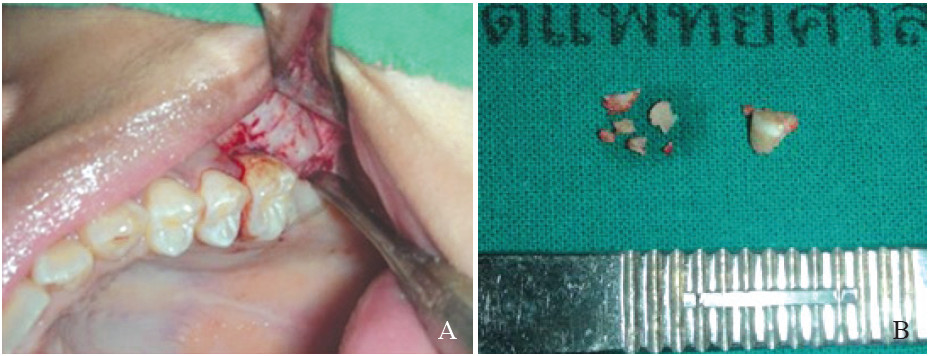
Figure 6: (A) An incisional biopsy was performed in the buccal area, starting from the distal of the left maxillary first molar. (B) The surgical specimen, consisting of several pieces of whitish-yellow hard mass resembling tooth structure, was sent for histological study.(A) Low power view of a disorganized dental hard tissue consisting of dentin,enamel and pulp tissue.(B) High power view of the enamel showing enamel rods.(C) Higher power view demonstrating dentinal tubules in the dentin.
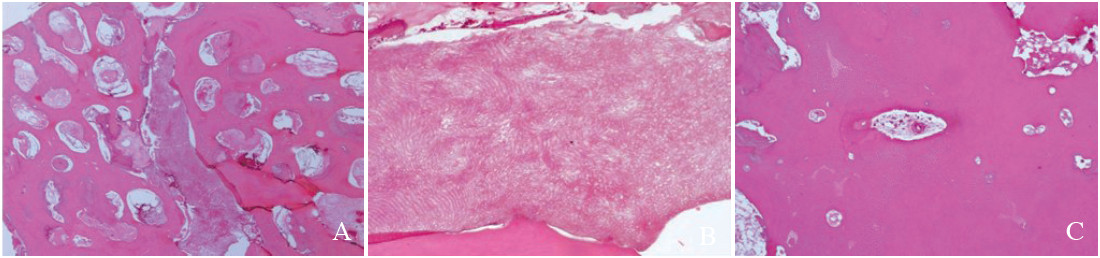
Figure 7: Histological section

Figure 8: A full-thickness trapezoid mucoperiosteal flap was reflected to expose the mass.

Figure 9: A thin layer of overlying bone was removed, revealing the odontoma.

Figure 10: The mass was completely removed in multiple pieces, together with the left maxillary second molar.
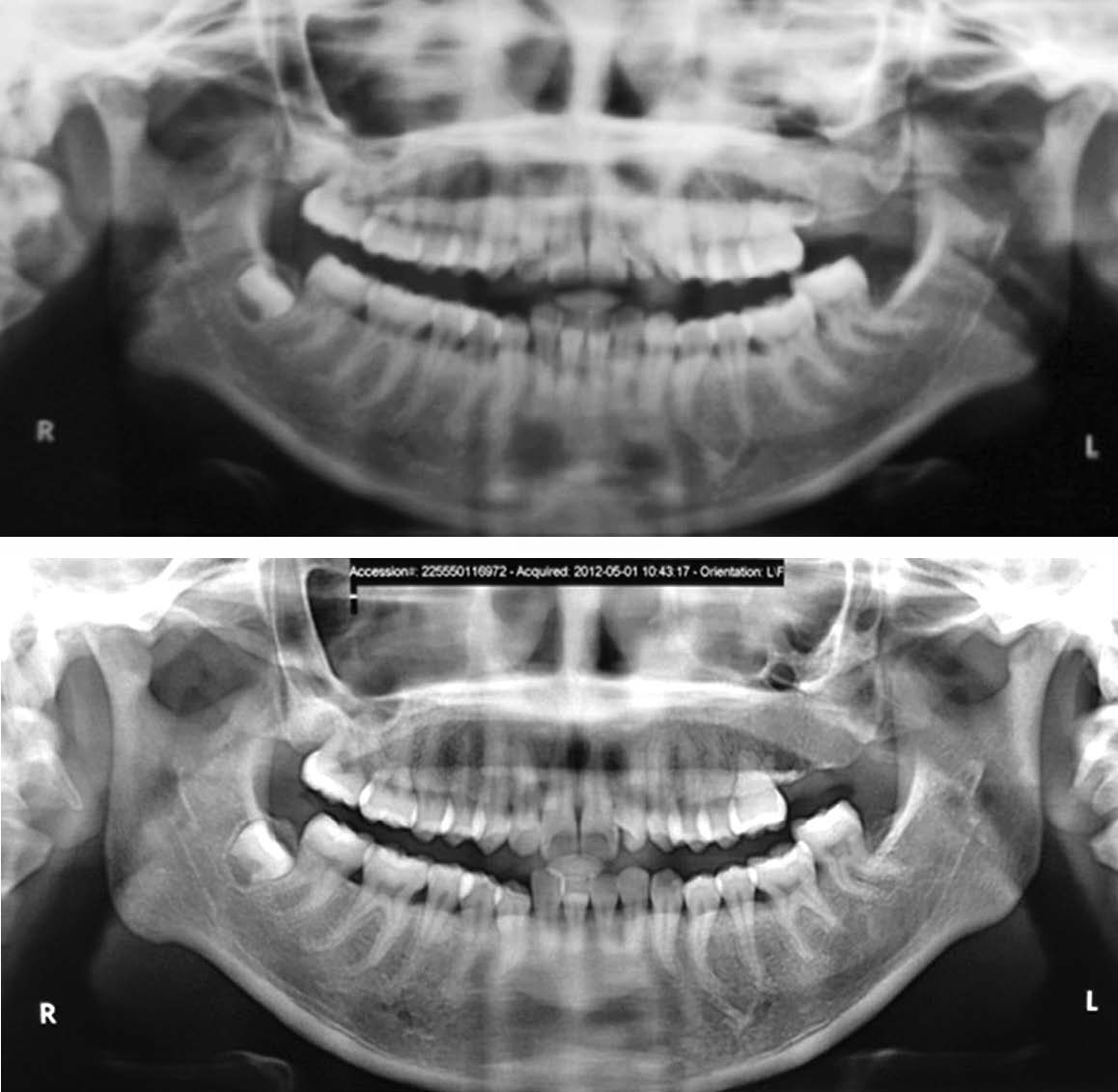
Figure 11: Radiographic examination at the 1st year (A) and 3rd year (B) after odontoma removal did not reveal any signs of recurrence.

Figure 12: Periapical radiograph at the 3rd year after odontoma removal showed normal root of the left second premolar. However, the first molar seemed to have dental pulp obliteration, short roots and lost its lamina dura.
Our case had the same presentation of most complex odontomas which commonly do not present any symptoms, and are often discovered during routine dental care.16,17 Although, the most common location for complex odon- toma is the posterior region of the mandible, several cases of complex odontoma have occurred in the maxillary sinus.16,18-22 Pain, chronic sinusitis, distortion of maxilla, nasal obstruction and a chronic draining sinus tract are some of the signs and symptoms of these cases.
Odontomas frequently interfere with tooth eruption, in addition, large lesions can cause tooth displacement. The case we reported here had an unerupted maxillary second molar which should have been detected at the normal erupting age (around 12 years old). Dentists should be aware of unerupted teeth and promptly investigate if a tooth does not erupt at the proper time. There are some reports of early removal of odontoma, that have been interfering with tooth eruption, but then resulted in normal eruption.6, 23 The involved tooth in our case was displaced to be near the orbital floor, therefore, we decided to remove it.
Most odontomas are small but occasionally they can reach a large size to cause bony expansion and swelling. Very large lesions can cause facial disfiguration. Large lesions in the maxilla can cause nasal obstruction, dis- placement of the lateral nasal wall, the maxillary antral floor, and the orbital wall.18, 19 Our case presented a very large lesion that occupied nearly the entire maxillary sinus but no symptoms were present or felt by the patient herself. The lesion affected not only the second molar displacement but also the root resorption of the first molar. The literature review revealed very few reports of root resorption in complex odontoma.19, 24
Generally speaking, the conventional 2 dimensional radiographs are sufficient to diagnose and to plan the treatment of small lesions. However, CT scans provide more details of the extent of the lesion and its relation- ship with adjacent structures.24 We performed a CT radio- graph in our patient to evaluate the boundary of pathology and the location of the displaced tooth. Removal of this lesion by sectioning into multiple small pieces saved the surrounding bone. Therefore, the operation was accom- plished smoothly without any complications.
The radiographic features and the age of occurrence in our case were quite similar to ossifying fibroma features. Therefore before any definite treatment plan could be determined, we needed to differentiate the complex odontoma from other aggressive tumors including odontoameloblastoma and ossifying fibroma. Odontoma is non-aggressive, and recurrence is uncommon3-5,10 therefore, it might have been a hamartoma rather than real tumor.25 The treatment of choice is enucleation and curettage. In contrast, a more aggressive tumor should be treated by block resection.4, 5
We present an unusual large mature complex odon- toma that occupied nearly the entire maxillary sinus and caused displacement of the permanent tooth. The definitive treatment was performed after the histological report was analyzed and after careful assessment of the size and location of the lesion. Skillful surgical removal resulted in non-disfigurement of the face and fewer associated complications.