Spinal stenosis is found frequently in the elderly, especially after the age of 55. The condition has become increasingly symp tomatic of longer life expectancy and a more active life style in the senior age group. Symptoms can range from an occasional, spontaneously reversible backache and claudication to full blown severe walking difficulties. More severe presentations of this condi- tion frequently lead to a more rapid advancement of other existing co-morbidities such as Diabetes Mellitus and Ischemic Heart Diseases, which require the ability to regularly exercise in order to maintain good control over the condition.
Some of the reversible symptoms of spinal stenosis can be addressed by a structured life style change and regular prescribed exercise program, frequently supplemented with occasional use of patient compatible anti-inflammatory medication. More severe presentations however need to be fully evaluated for possible surgical treatment. The primary aim of surgery is to alleviate the nerve root (s) compression producing the symptoms. The secondary aim is to correct or stabilize any instability that may have contributed to the development of the stenosis or could possibly aggravate the stenosis in the future along with producing additional symptoms on its own.
Procedure has been found to provide the needed decompression and still allow a full interbody stabilization.
The correlation between the presence of lower lumbar spinal stenosis and claudication symptoms in the affected nerve roots has long been well established. Documentation of the stenotic part of the lower lumbar spinal canal was originally done with the use of myelography and cadaver study. With the development of the Computerized Tomography (CT Scan) and later the use of Magnetic Resonance Imaging (MRI Scan) the pathology could be fully evaluated and understood without any invasive procedure. As a result, since the 1960’s, a standard wide multi-level decompression though bilateral laminectomies and partial facet resections became the accepted standard of surgical treatment. By the mid 1970’s it became apparent that there are surgical consequences to such an extensive approach.
Mostly in women patients, and predominantly at the L4-5 interspace the incidence of post operative progressive instability can be as high as 35%. This can lead to a recurrence of the stenosis, now a result of misalignment and other symptoms related to the instability.
The deeper understanding of lumbar spine stability, the availability of limited exposure surgical techniques through the use of microscopes in surgery and the development of muscle splitting instruments along with a more conscious philosophy of preserving the natural stabilizing structure as much as possible, led to a reconsideration of the surgical choices in the treatment of lumbar spinal stenosis. In several settings these resulted in a structured surgical treatment plan that directly addressed the patients’ main symptom and reduced the associated undesirable surgical consequences.
For patient without instability as defined by a lack of any misalignment and no excessive motions on dynamic spine films, it has been well established that the incidence of postoperative instability is between 8-13%.5, 17, 18 Less than half of this instability has been found to contribute to adverse decompression has a direct relationship to the possibility of instability.5, 8 As a result, Sonntag and Marciano, Grob, Kristof and Shenkin recommend no prophylactic fusion in any cases with less than a Grande I Spondylolisthesis. With the use of more limited decompression techniques, the incidence of postdecompressive instability is further reduced. In addition, microsurgical and minima exposure tech- niques, some using a muscle splitting incision appear to reduce the problem of surgically induced instability further while delivering the expected improvement from the nerve root decompression.12, 13, 17, 19 In 1995, Aryanpur and Ducker pioneered the concept of limited unilateral decompression that proved to be very useful in relieving the stenotic symptoms bilaterally.
In the presence of less instability (usually defined as less than a Grade II Spondylolisthesis) associated with limited back pain on motion, many authors have presented evidence indicating that concurrent prophy- lactic fusions of any type may not be indicated. 2, 10, 13, 18 Conversely, there are some reports of the benefit of pedicle screws immobilization in reducing motion related back pain after decompressive surgery: unfortu- nately, this does not directly correlate to the existence of solid bony fusion. There are fewer questions regarding the value of concurrent fusion at the time of decompres- sion in cases where the presence of presurgical instability is well established .2, 3, 12, 18 The type of fusion and the approach have evolved technically to the present stage where minimally invasive exposure and interbody implant placement are simpler and safer. 7, 8, 19 Here again, the less invasive.
In the author’s personal experience, careful evalu- ation of the inherent instability associated with degen- erative spinal stenosis allows for a structured surgical treatment plan. In the presence of minimal preexisting instability associated with predominantly unilateral radiculopathy, a limited unilateral laminotomy over the involved segment (s) will result in a significant relief of the main presenting symptoms, while reducing the risk of surgically induced additional instability to a minimum. The use of microsurgical techniques and a conscious attention to preserving as much facet stability as possible will result in a functional lumbar spine. Staging the laminotomy decompressions by performing the decompression on the more symptomatic side first to be followed with the less symptomatic side several weeks later, sharply reduces the incidence of additional insta- bility. In certain settings it became clear that unilateral microdecompression can significantly relieve bilateral symptoms and eliminate the need for additional opposite side surgery. The need for additional opposite side surgery in the author’s experience range is about 10%, in other words 90% of the patients can do very well with a simple unilateral decompression using minimally invasive techniques with the known benefit of a much reduced risk and shortened recovery.
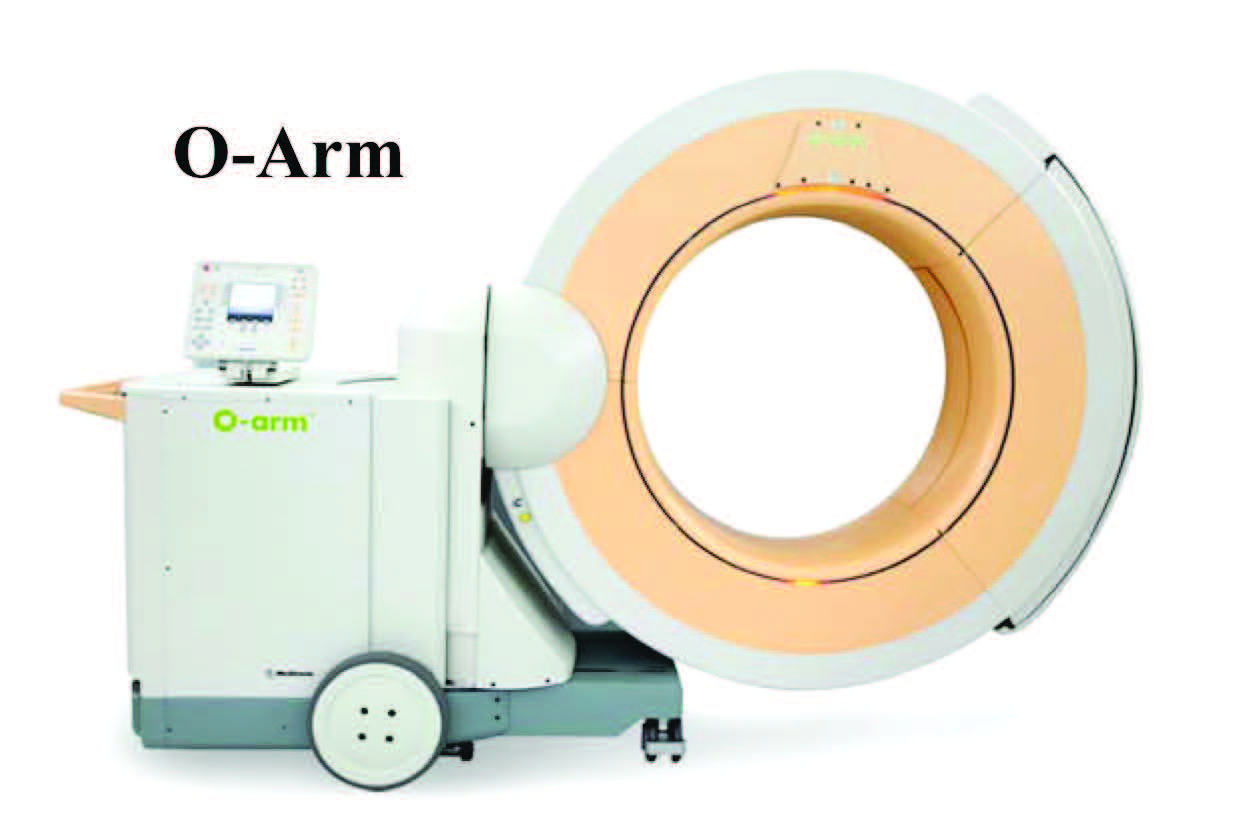
This staged surgical treatment requires a full detailed disclosure to the patient, at the beginning of consider- ation of surgical treatment. Somes patient are not willing to accept the possibility of additional surgery and may not instead for a more extensive bilateral decompression and even possibly a prophylactic fusion/ instrumentation as the definitive surgery, despite the additional scope, risks, expense and a longer recovery period. For patients with some instability, a full assessment of the origin of the stenosis is necessary. Stenosis which is the result of a collapsed slightly displaced disc space involving one or two segments can now be corrected with a direct realignment and restoration of the sagittal dimension of the nerve root foramen, by a stand alone direct anterior interbody fusion with a secured femoral ring equivalent implant that provides both the stability and the spacing restoration. This technique has the advantage of preserv- ing the posterior elements necessary for stability and allows for additional percutaneous placement of addi- tional instruments if felt to be necessary. This recently developed technique does require additional surgical skills and specially designed implants, as well as incur- ring increased expense related to new technology. For severely unstable spine with stenosis, the traditional approach of wide, multi-level decompressions supplemented by fusion and instrumentation remains accepted. In this setting, again the advent of minimally invasive techniques, specially designed implants and dedicated surgical instruments allowed the surgeon to choose appropriate approaches. Transforaminal Lum- bar Interbody Fusion through a unilateral exposure and contralateral percutaneous instrumentations is becoming more accepted. Once surgeons training and appropriate skill levels become widespread, the benefits of the new techniques will be routine. These newly developed pro- cedures and the use of real time imaging (O-Arm intra-operative CT) and navigation (Stealth Spine Navigation) have greatly increased the level of safety.
Spinal stenosis is especially common in the elderly. The purposes of surgical intervention are to alleviate the nerve root compression and correct any instability. The inherent instability associated with degenerative spinal stenosis should be evaluated carefully prior to surgical treatment. Despite the improvements in the results of surgery for spinal stenosis, one can never overlook the fact that symptomatic improvement is never complete and can be short lived.
Many factors are involved in the deterioration of the result, not the least of which is the patients’ own general aging process and the natural progression of the spi- nal stenosis and intervertebral joints degeneration with time. The possibility of additional surgery at a later date always exists
Spine surgeons therefore should rethink the traditional approach to the treatment of spinal stenosis, the concept of prophylactic fusion may not be as applicable as be- fore, and the choice and extent of the surgical procedure should be selected based upon current updated data, with the patients’ full participation after detailed discussion. The inherent increased risks with more extensive surgery can be avoided and reserved for cases where the need can be well defined. The primary objective in treating spinal stenosis by surgery remains the relief of enough symptoms to allow the patient to lead a reasonably active life while using up the least amount of time and resourc- es to reach that point, and incurring the least possible treatment risks along the way.