Sepsis is an inflammation syndrome which is caused by severe infection. This severe inflammation is characterized by vasodilatation, leukocyte accumulation and increased microvascular permeability. The pathophysiology of sepsis is believed to be due to the dysregulation of the inflammatory response. The human body generates and releases a massive uncontrolled amount of proinflammatory mediators into the blood stream which causes cellular and tissue injury. This injury leads to the development of multiple organ dysfunction syndromes (MODS), and causes life-threatening conditions.
The normal host response to infection involves the activation of circulating and fixed phagocytic cells, the generation of proinflammatory and anti-inflammatory mediators. When the body releases massive cytokines beyond the infection site, sepsis occurs. These mediators cause fever, hypotension, acute phase protein response, induction of interleukin 6, coagulation activation, increased endothelial permeability and so on. These large quantities of proinflammatory mediators will cause cellular damage and lead to multiple organ failure.
In conventional therapy for sepsis, the priority is to eradicate infection by using appropriate antibiotics and surgical interven- tions, and to initiate supportive care in order to correct physiologic abnormalities such as hypoxemia and hypotension.1-4 Despite optimal treatment and close monitoring in intensive care units, the mortality rate due to severe sepsis and septic shock is approximately 40% and can exceed 50% in the sickest patient.5-8
A study from Nakada TA, et al.9 in 2008 showed a decrease of interleukin 6 and procalcitonin correlated with survival during sepsis. The innovative idea to reduce proinflammatory cytokines led to the development of the extracorporeal blood purification technique. Extracorporeal blood purification can be performed in different ways. The treatment restores the normal balance of the targeted substances within the patient’s body.
Coupled plasma filtration adsorption (CPFA) is a therapeutic extracorporeal blood purification tool combining 3 techniques namely plasma filtration, adsorption and hemofiltration. CPFA is suitable for illnesses involving renal failure together with large molecules, especially if these have a molecular weight close to that of albumin such as inflammatory substances found in sepsis and in liver failure. The CPFA technique has been performed in animal experimentation and in clinical settings worldwide since 1998. Some CPFA studies have been reviewed (Table 1).
Table 1: Coupled plasma fi ltration adsorption (CPFA) studies review.
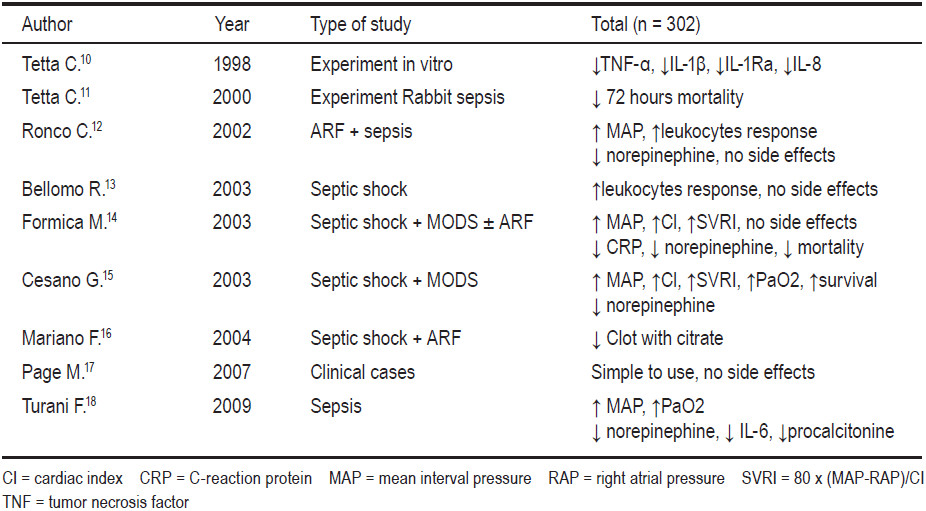
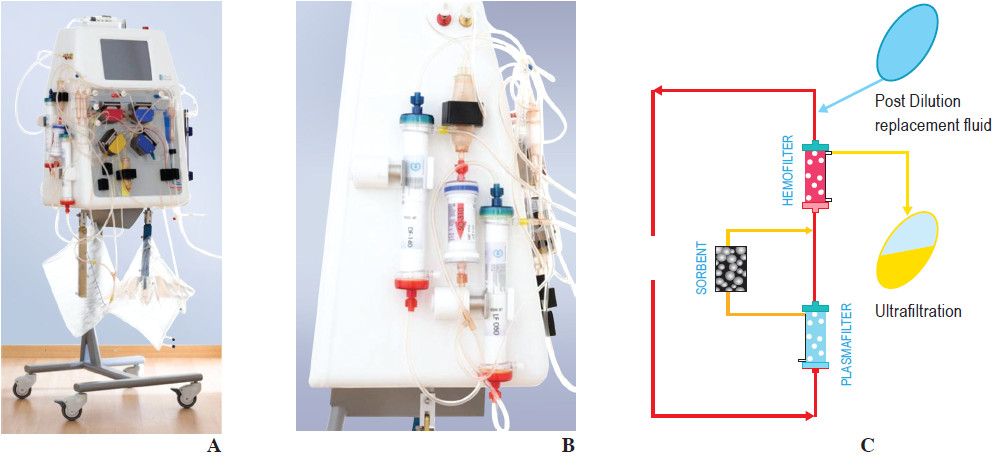
Figure 1: Shows CPFA Machine (A-B) and the third fi lter (Hemofi lter) (C)
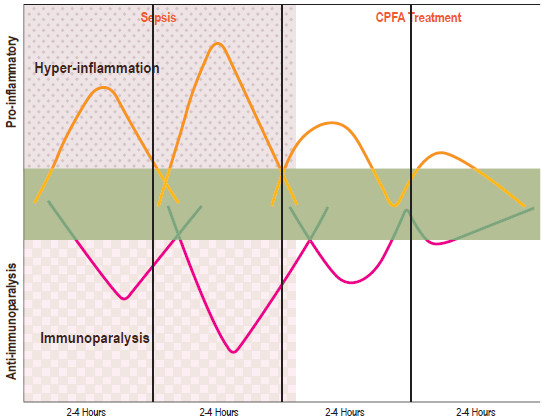
Figure 2: The innovative idea to reduce infl ammatory substances in sepsis by CPFA treatment.
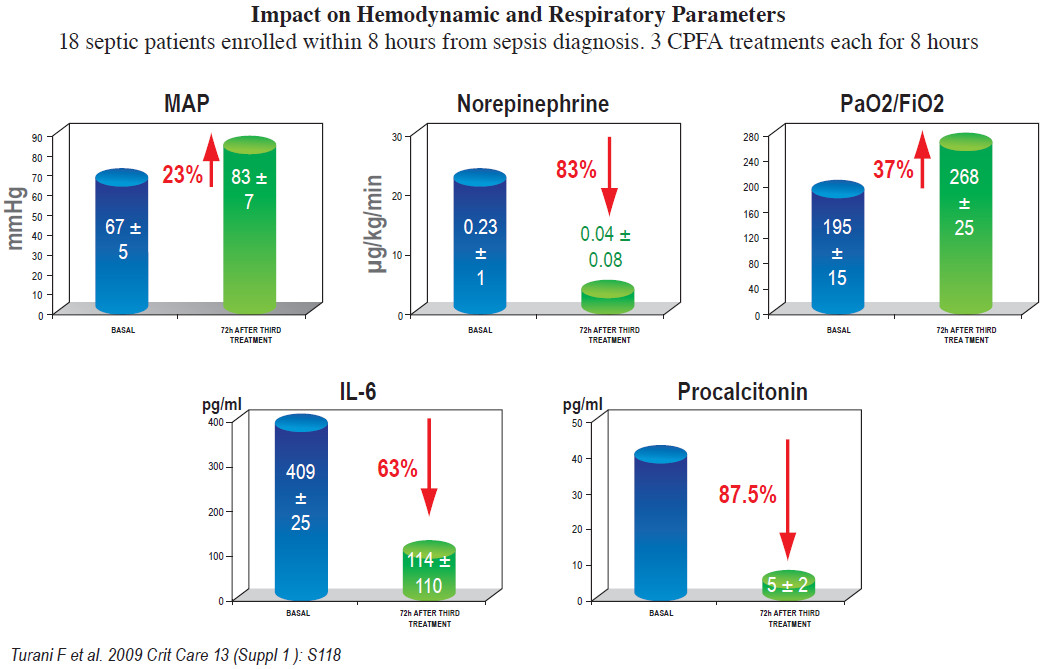
Figure 3: This Turani F. study showed the improvement of mean interval pressure (MAP). The decrease of norepinephrine dosage use, the increase in oxygenation, and the reduction of interleukin 6 and prolactin in 72 hrs after the 3rd CPFA treatment
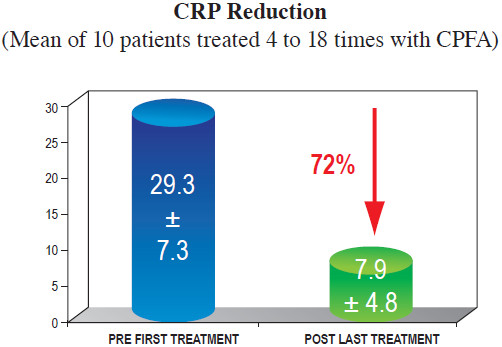
Figure 4: Laboratory data shows a sharp decline of C-reaction protein (CRP) throughout the treatment time (from before the fi rst treatment to after the last treatment).19
CPFA is designed to remove some specific large substances by plasma perfusion in-line with continuous veno-venous hemofiltration (CVVH) which replaces kidney failure. The CPFA machine (blood purification HF 440, Infomed, Switzerland) contains 5 blood pumps and 3 filters (Figure 1A-B).
There are 3 steps to the technique. First, blood is passed through a plasma filter. The plasma is filtered and sent to a second filter (a sorbent cartridge). This sorbent cartridge is important because it absorbs large molecules, in particular interleukin 1β, interleukin 6, interleukin 8, interleukin 10, macrophage inflammatory proteins (MIP-α, MIP-β), tumor necrosis factor (TNF-α), endotoxin, peptidoglycan, bradykinin, angiotensin, leptin, retinol binding protein, prostanoids, complement factors, coagulation components, nitric acid, oxygen radicals, and bilirubin. The obtained plasma returns to the blood, and together passes through the third filter (hemofilter). The hemofilter placed on the blood flow allows hemofiltration to be performed which compensates for the kidney failure often associated with the main disease (Figure 1C).
In late 2012, at the Bangkok Hospital Medical Center (BMC), a 60-year-old man with a past medical history of diabetes and end stage renal disease on hemodialysis was admitted due to an infected diabetic foot. During hospitalization, he had an ischemic bowel requiring surgery. Later on, he developed sepsis and multiple organ dysfunction syndromes, including acute respiratory distress, hemodynamic instability, liver injury with high bilirubin levels, and bleeding disorders. His proinflam- matory cytokines were very high especially interleukin 6, procalcitonin, and C-reactive protein.
A BMC medical team decided to perform blood purification by CPFA technique in order to reduce proinflammatory cytokines and bilirubin levels. However, he had abnormal coagulopathy so the team decided to use a citrate substrate for anticoagulation instead of heparin.
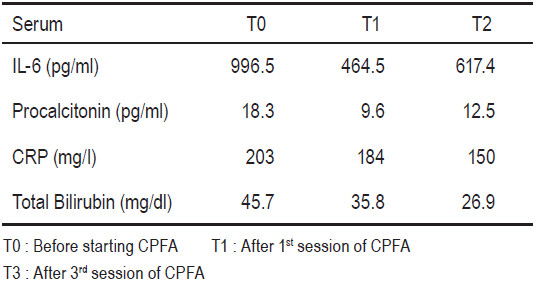
After 3 sessions of 10 hours CPFA with 0.22l/kg/d of plasma purification, the level of interleukin 6, procalcitonin, C - reactive protein, and bilirubin had declined drastically (Table 2).
Table 2: Coupled plasma fi ltration adsorption (CPFA) studies review.
In Thailand, this was the first case time a coupled plasma filtration adsorption treatment was used to reduce cytokines in sepsis. The cooperation between the Bangkok Hospital Medical Center and Infomed gave the team the required knowledge, learning experience, and the necessary additional tools to fight this life-threatening disease.
Acknowledgements
The author thanks doctors and staff at Bangkok Hospital, Bangkok, Thailand: Dr. Paithoon Boonma (Infectious Disease Clinic), Dr. Chanwit Wuttichaipradit, Dr. Somsit Tancharoen (Colorectal Clinic), Dialysis Nurses, Intensive Care Unit (ICU 1) Nurses. Thanks also to Econtech Supply of Thailand and Infomed of Switzerland.