Radiofrequency ablation (RFA) is a new, alternative treatment for Brugada Syndrome.1 Radiofrequency ablation, using two catheter navigation systems (CARTO and EnSite), offers advanced ablation therapy for complex arrhythmias. In this technique, the Multi-Detector Computed Tomography (MDCT) images are shown as three dimensional (3D) images constructed to localize the target area. In case of Brugada syndrome, the target for ablation is RVOT. In Brugada syndrome patients, coronary artery disease should always be assessed before ablation operation. MDCT scanning with contrast for RVOT and for coronary artery evaluation may be requested. Although a double CT scan (two separate scans) can provide all necessary information, however the large dose of radiation and iodinated contrast exposure and indeed the cost are matters of concern. In this article, we detailed the modified double-purpose technique of CT scan which could reduce the radiation and contrast exposure dose in RVOT and coronary artery imaging whilst maintaining acceptablereadable image quality
Between 2009 and 2012, a total of 13 cases of Brugada syndrome were scheduled for RFA and underwent 256-slice MDCT scan for RVOT and coronary artery structure demonstration. Exclusion criteria included patients at risk for severe iodinated contrast agent allergy, severe asthma with bronchodilator dependence or elevated serum creatinine > 1.5 mg/dl. To verify the effectiveness of the modified, minimally added contrast volume technique, we retrospectively assessed the image quality of RVOT and coronary artery in terms of CT attenuation value ≥ 250 HU which is the minimum requirement value for MDCT diagnostic image.2
CT angiography (CTA) for RVOT and coronary artery
CT studies were performed on 256-slice MDCT (Brilliance ICT, Philips, Netherlands) scanner with bolus tracking protocol. A bolus volume of iodinated contrast injection was calculated by the formula of scan time (5 -6 sec. for pulmonary artery scanning) plus post threshold delayed time (~5 sec.) and multiplied by flow rate (4.5- 6 ml/sec.) as per Philips company protocol. Five to fifteen (5-15) milliliters of contrast agent was added to the calculated volume. A contrast bolus was injected into brachial vein at a flow rate of 4.5-6 ml/sec. , followed by 50 ml. saline solution injection. The tracking position was placed at the pulmonary trunk and scan started automatically at 5 sec. after reaching the threshold (100 HU.). Cardiac scan length covered from the carina angle to 2-3 cm. below the diaphragm using the following parameters: x-ray tube potential 120-140 kV, tube current 471 MA, slice collimation 128x0.625 mm². , table speed of 44 mm/sec., and pitch 0.16. The slice thickness was of 0.625 mm. The mean RVOT- coronary artery scan time was 5 sec. The retrospective electrocardiographic gating was routinely used for cardiac phase selection. The CT attenuation HU value of the ascending aorta was used to represent the HU value of the coronary artery. The CT attenuation HU value was measured at the RVOT itself. The MDCT image data was independently and blindly analyzed by three experienced cardiac CT specialists. The acceptable/readable RVOT and coronary artery image quality for pre-ablation CARTO sound image-merging process and assessment was determined using CT attenuation value > 250 HU as a cutoff criteria. The patient’s body weight (kg), calculated and actual contrast use (ml), the total added volume of contrast (ml), the CT attenuation value of RVOT(HU) and of ascending aorta–coronary artery (HU) were reported in range.
In our study, thirteen Brugada syndrome patients were recruited. The average age of the patients was 53.8 years old and the average weight was 63.6 kilograms (range 51- 78 kg). The heart rate of all patients ranged from 52-91 beats per minute. All of these patients were planned for RVOT catheter ablation, using CARTO sound navigator. The 256-slice MDCT scan with contrast injection was requested for RVOT and coronary structure demonstration in all patients. Nine patients (9/13) underwent 256-slice CT scan using the modified double purpose technique. All of RVOT structures and coronary artery segments were studied. The MDCT image quality of the right ventricular outflow tract (RVOT) and coronary artery as acceptable/readable use a cutoff criteria of CT attenuation of the region of interest that is equal or more than to 250 HU (Hounsfield unit). CT attenuation value of 250 HU is the minimum requirement value for diagnostic images.2 Four patients (4/13) underwent the conventional technique for CT angiography for pulmonary artery. The CT attenuation value of the RVOT and ascending aorta-coronary artery of all nine patients (100%) who underwent 256-slice MDCT scan with the modified, minimally added contrast volume technique met the cutoff point criteria (Table 1, Table 2).
Four patients who underwent conventional technique of CTA (CT angiography) for pulmonary artery did not meet the acceptable readable criteria in a single scan as shown in Table 3. The averaged contrast volume used in the conventional technique was as calculated volume. The averaged contrast volume use in modified technique was the calculated volume plus 5-15 ml in any heart rate. By the result of CT attenuation value analysis, the recommended volume of contrast use was calculated volume plus 10-15 ml for the patient’s weighs less than 80 kg regardless of the heart rate and the total volume should not be less than 60 ml. For the modified, minimally added contrast volume technique, we used the same protocol as for pulmonary artery scanning and added some contrast agent. The radiation dose exposure of the patients who underwent 256-slice MDCT using the modified technique was the same as the dose needed to perform ECG-gated 256-slice MDCT scan for pulmonary artery.
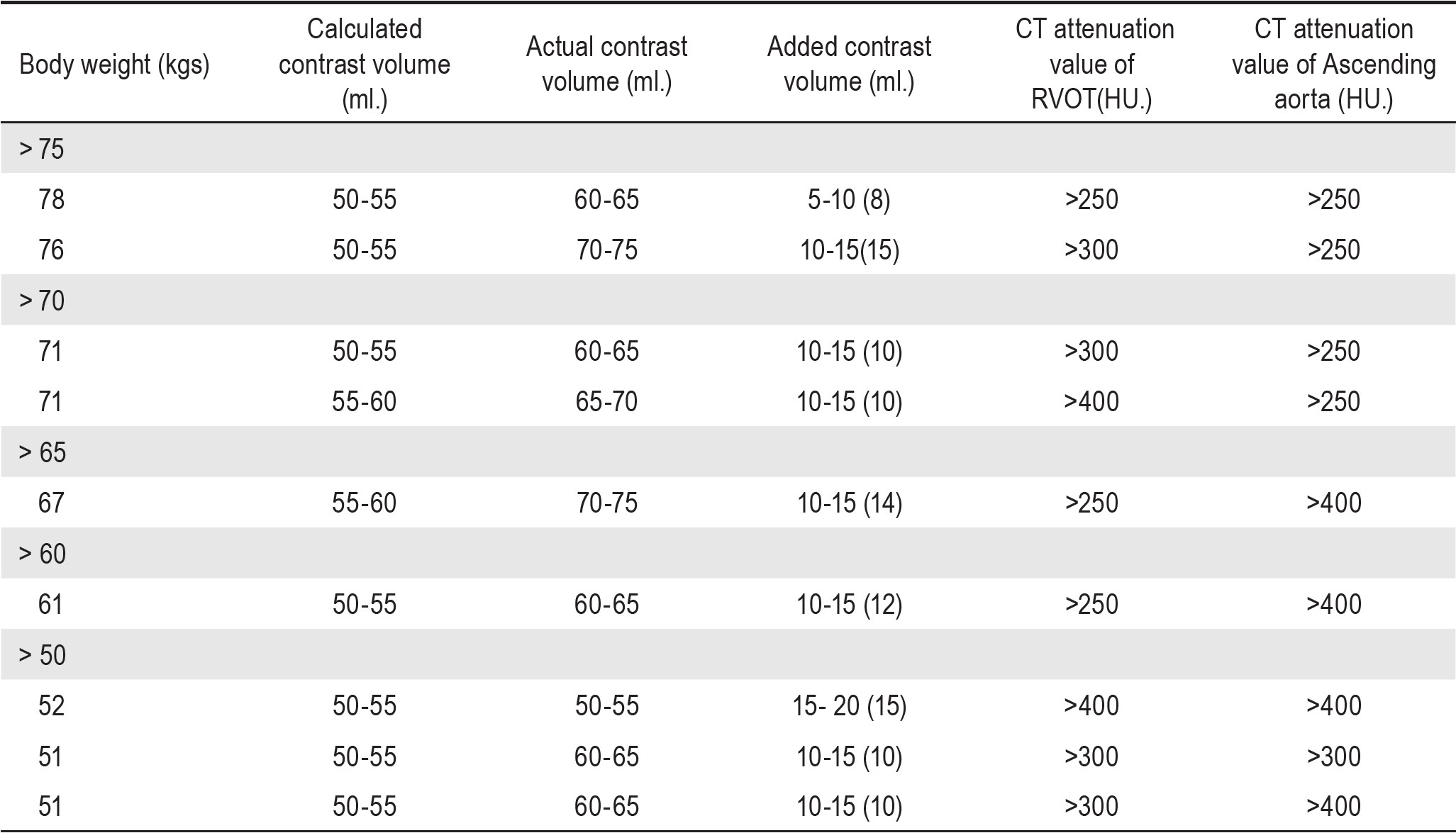
Table 1: Demonstration of CT attenuation value of RVOT-Coronary artery image evaluation using modified technique (9 cases)
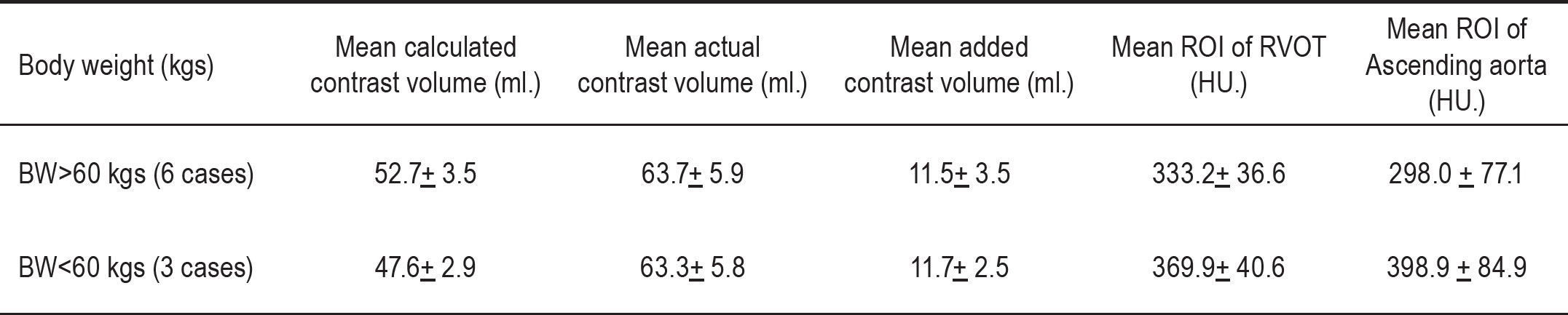
Table 2: Demonstration of Average CT attenuation value of RVOT - Coronary artery images using modified technique (9 cases)
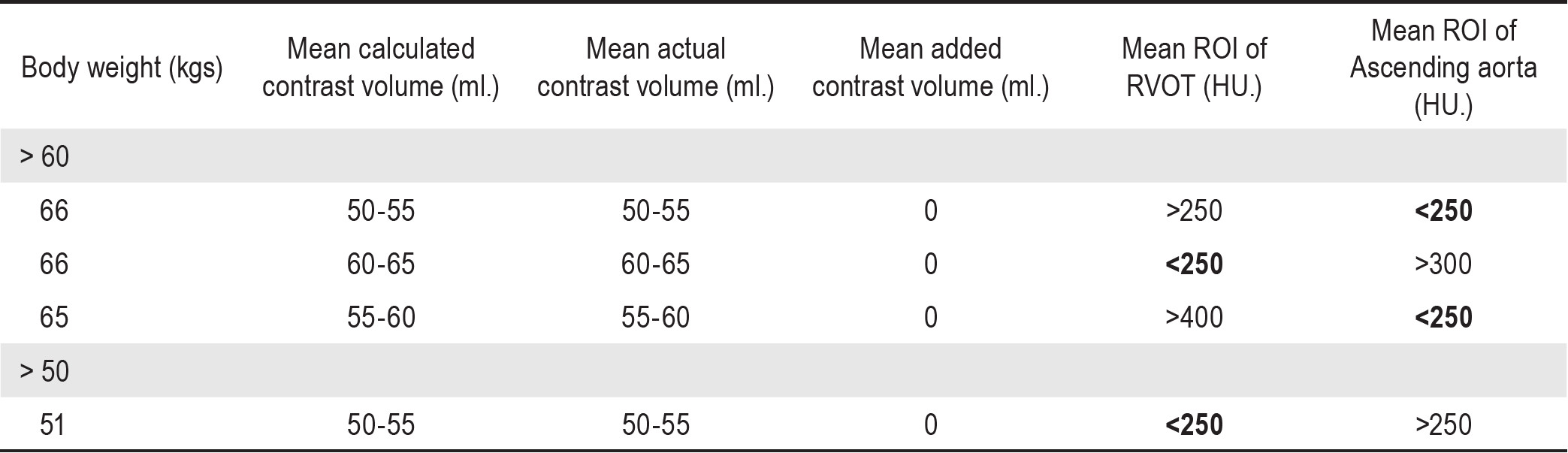
Table 3: Demonstration of Average CT attenuation value of RVOT - Coronary artery images using modified technique (9 cases)
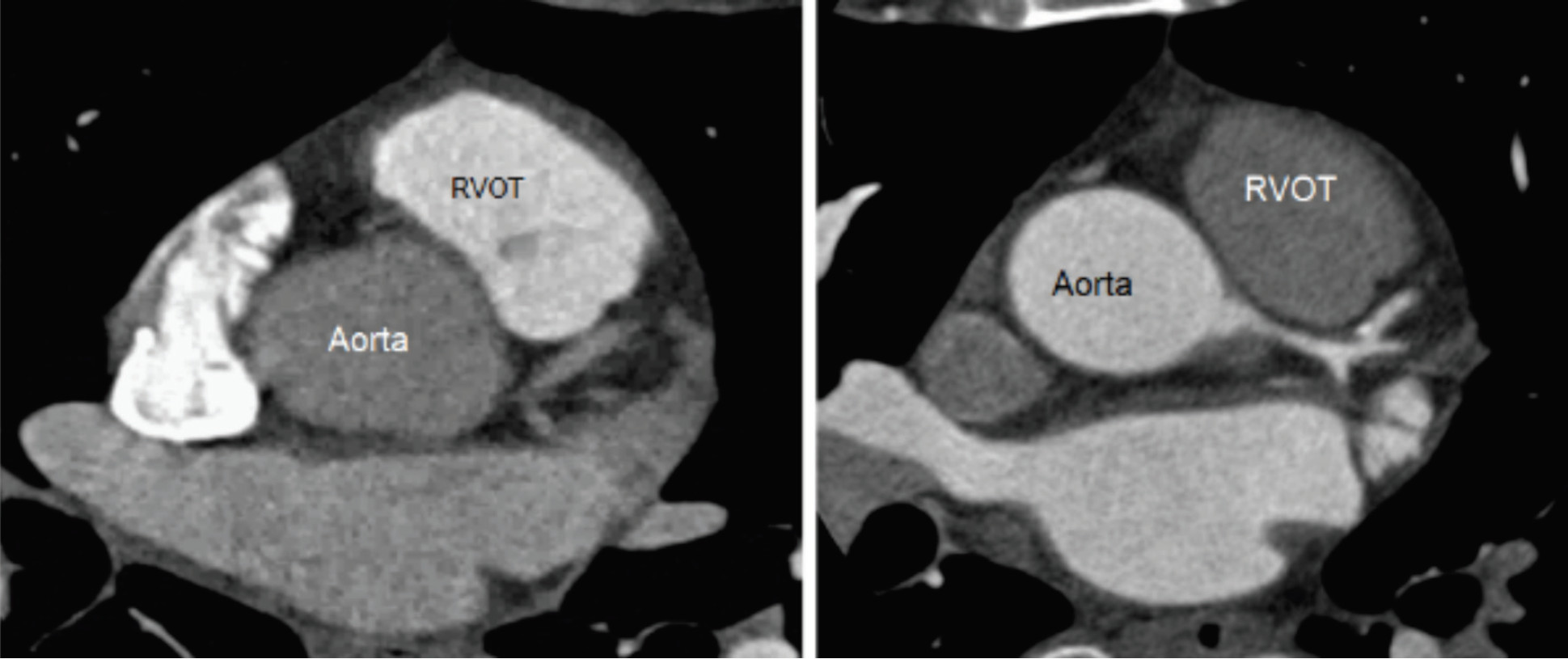
Figure 1: Demonstration of the RVOT images and ascending aorta-coronary arteries obtained from 256-slice MDCT using conventional technique
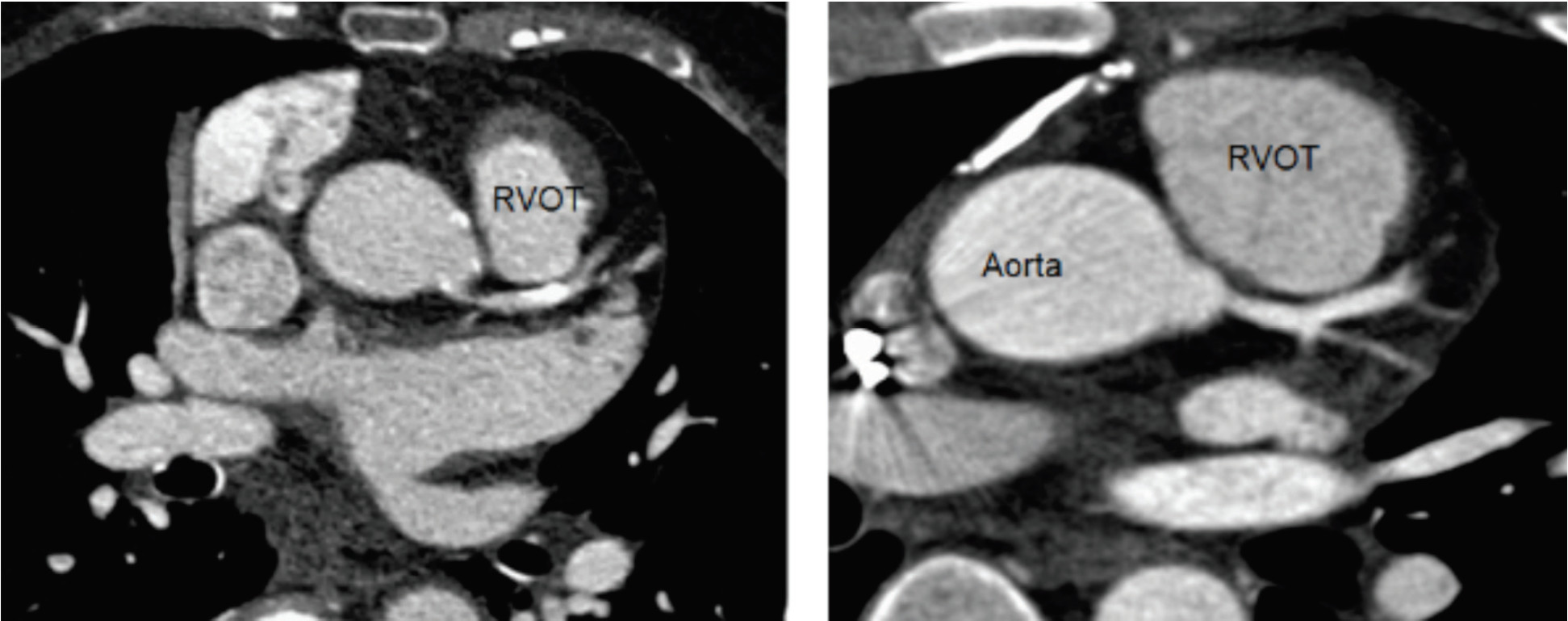
Figure 2: Demonstration of the RVOT images and ascending aorta-coronary arteries obtained from 256-slice MDCT using modified minimally added contrast volume technique
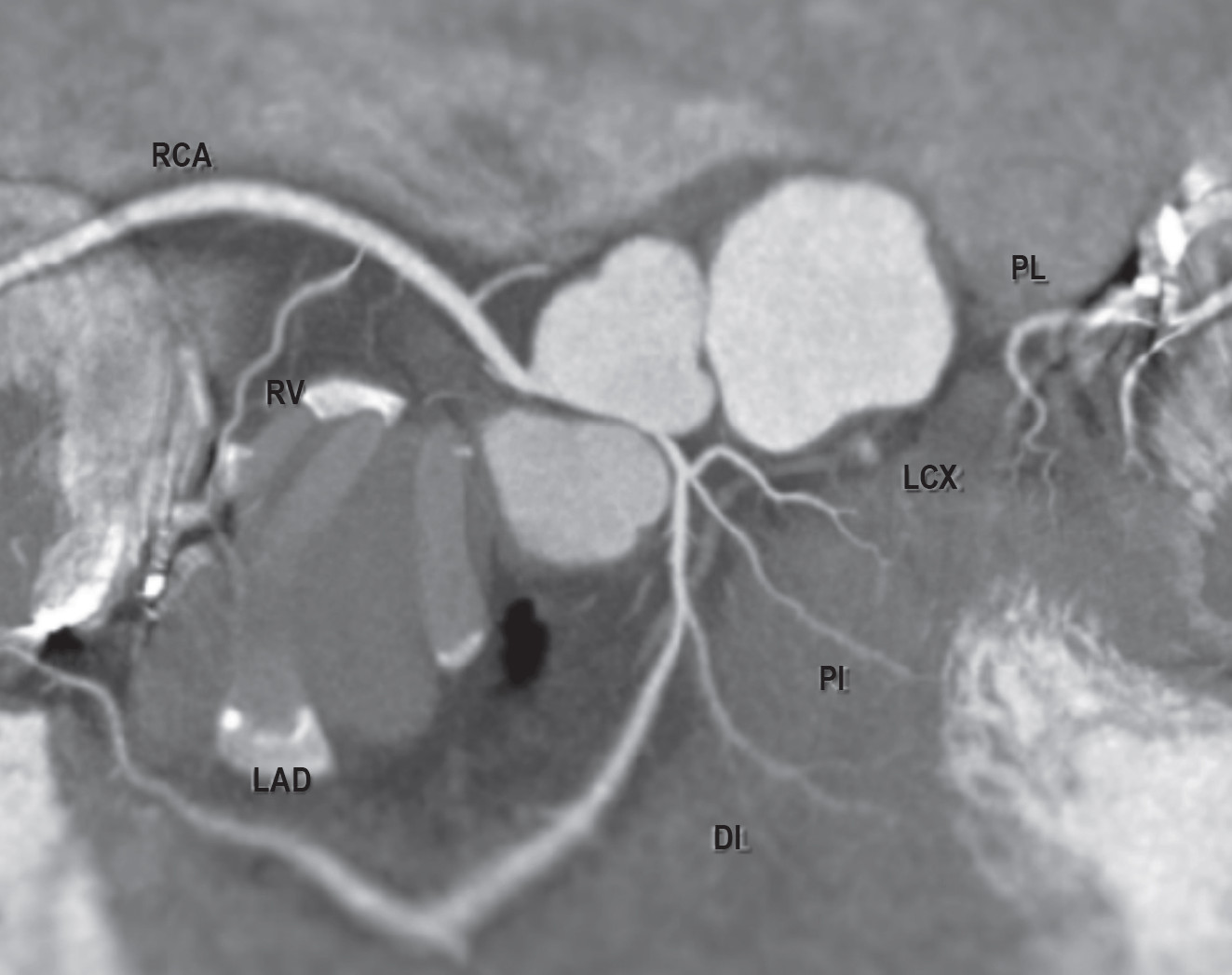
Figure 3: Multiplanar reconstruction (MPR) image of all coronary arteries obtained from 256-slice MDCT scan with using modified, minimally added contrast volume technique
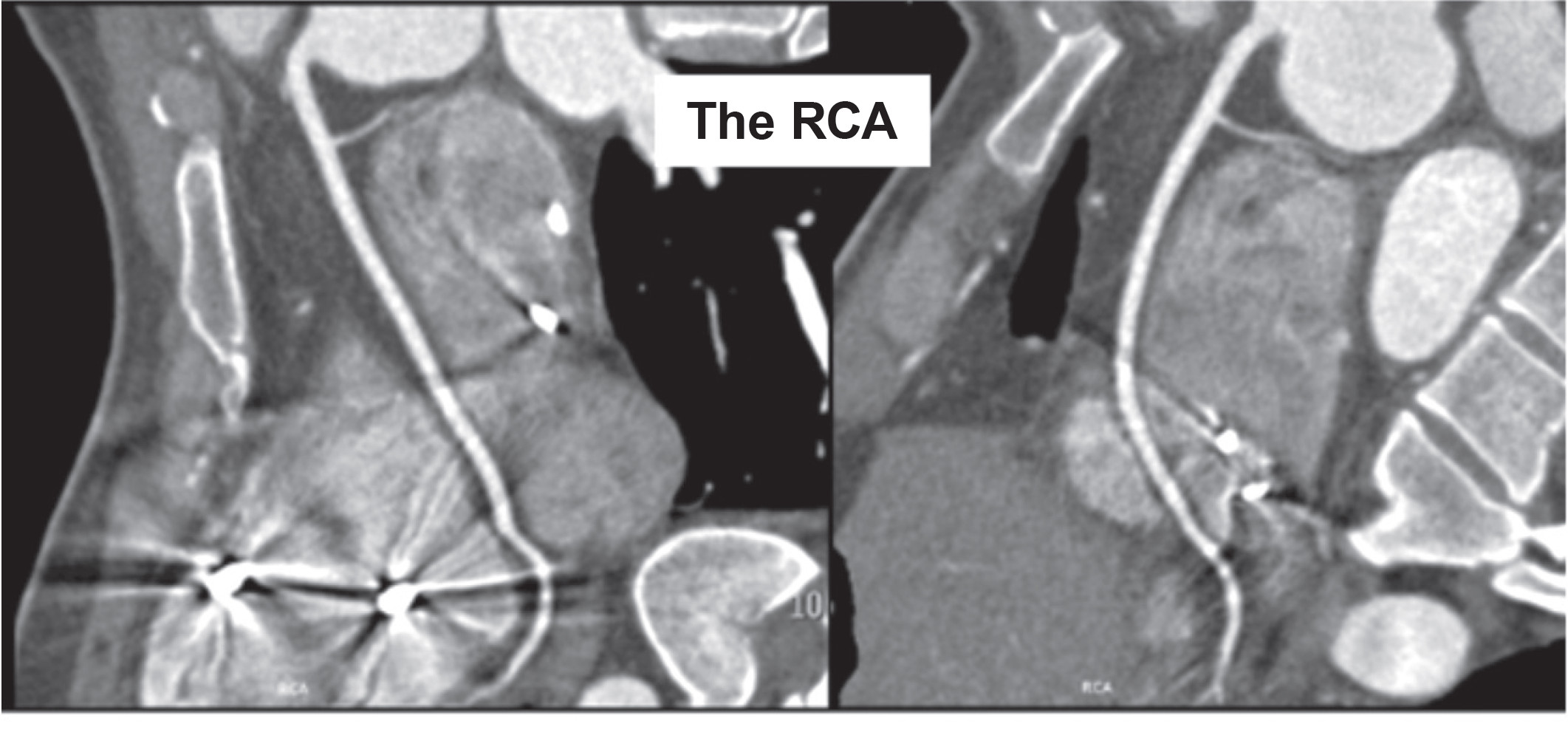
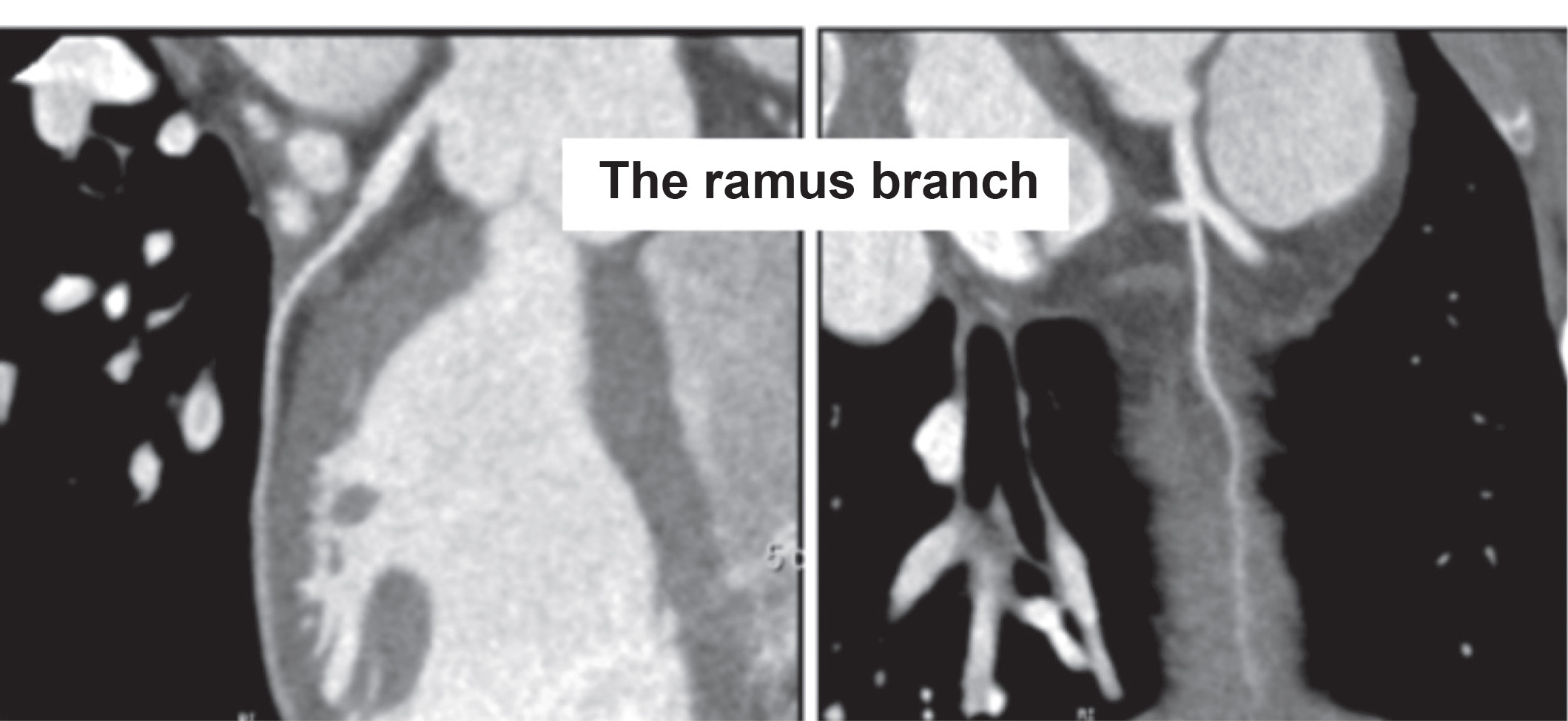
Figure 4: MPR image of all coronary arteries obtained from 256-slice MDCT scan using modified technique
The 256-slice MDCT scan with modified, minimally added contrast volume technique is a single MDCT scan technique which can be used effectively in demonstrating RVOT and coronary artery for pre-RVOT ablation planning with acceptable and readable image quality in Brugada syndrome patients whose body weight is in the range of about 50-75 kilograms. The proposed calculated formula for contrast volume is scan time (5-6 sec. for pulmonary artery scanning) plus post threshold delayed time (~5 sec.) and multiplied by flow rate (4.5-6 ml/sec.) plus 10-15 ml.
According to the results from our relatively small number of subjects, the proposed calculation for contrast volume use in the modified technique cannot be extended to the patient who has a body weight of more than 75 kilograms without corresponding decrease in image quality. All of our subjects were Thai people, who have on average a lower body weight than Caucasians.
The authors thank to all doctors, radiologic technologists and nurses of cardiac imaging team for their great support