Transverse myelitis syndrome most often occurs as an autoimmune phenomenon after an infection, vaccination, autoimmune disease or acquired demyelinating disease. It is characterized by bilateral motor weakness, clearly defined sensory level and autonomic spinal cord dysfunction. Investigations demonstrated spinal cord inflammation, either by magnetic resonance imaging (MRI) or cerebrospinal fluid (CSF) inflammatory change.1 Initial high dose steroid therapy is recommended to reduce the inflammation. If possible, etiologically specific therapy should also be instituted.
Primary infection with varicella zoster virus (VZV) causes chickenpox and may result in acute cerebellitis and stroke in childhood. It becomes latent in cranial nerve and dorsal root ganglia and can reactivate later in life to produce herpes zoster or shingles. Severe neurological complication are often found during this reactivation phase, such as cerebral vasculitis and encephalitis.2 Prompt antiviral treatment is strongly recommended to prevent morbidity and mortality.
A previously healthy 30-year-old woman was admitted to an outside hospital due to a varicella skin eruption lasting seven days. It was followed by paraplegia and urinary retention. She had good awareness and cooperated well. Three days later, she became lethargic, had fever and dysphagia within 24 hours. Then, she was intubated and was referred to our hospital. Physical examination upon admission revealed high fever, vesicular rash with hyperemic base and some crusted rashes on the whole body. Neurological examination showed drowsiness, absence of nuchal rigidity and normal cranial nerve function. Muscle power of upper extremities was at grade 4 (Medical Research Council (MRC) scale), except the deltoid at grade 3, but there was no movement at all in the lower extremities (grade 0). Sensory level was found at 4th thoracic level. Hyperreflexia, positive Babinski’s sign and loose anal sphincter tone were present. She had no previous history of chickenpox and had never had a chickenpox vaccination. Additionally, her husband developed chicken pox at the same time.
Computed tomography (CT) scan of the brain with contrast, MRI brain and chest x-ray were unremarkable. MRI of whole spine revealed long segmental ill-defined hyperintense T2 change with patchy enhancement extending along the entire spinal cord from the cervicomedullary junction to the conus medullaris. It mainly involved central gray matter and some peripheral white matter. There was diffused mild enhancement of the cauda equina nerve roots (Figure 1).
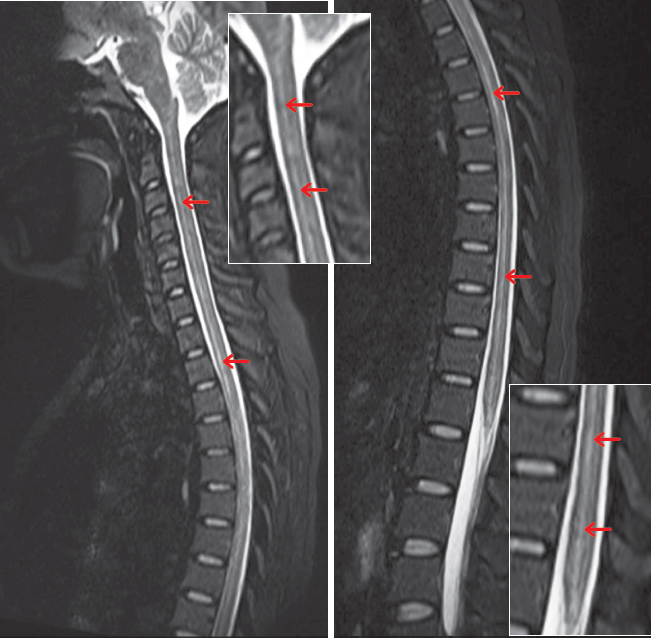
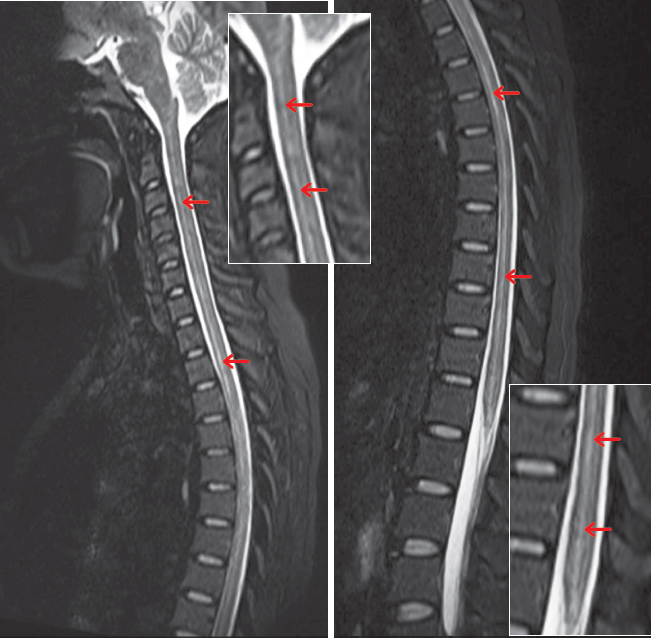
Figure 1: Magnetic resonance imaging of whole spinal cord revealed long segmental ill-defined hyperintense T2 change extending along the entire spinal cord from cervicomedullary junction to conus medullaris, which mainly involves central gray matter.
Laboratory revealed the following: anti HIV was negative, complete blood count showed leukocytosis, mild elevation of liver enzymes. CSF was clear and colorless, WBC 30 cells / μL (mononuclear 98 %, PMN 2 % ), RBC 450 cells/ μL , protein 62 mg/dL, sugar 54 mg/dL ( blood sugar 115 mg/dL ). Urinalysis showed evidence of urinary tract infection. Hemoculture and urine cultures showed no organism. Serological test for varicella-zoster virus was positive for IgM antibody.
The patient also had an EEG done which showed generalized background slowing in theta range, without epileptiform discharges. The CSF examination also revealed pleocytosis which suggests inflammatory response. Therefore, coexisting encephalitis cannot be totally excluded. Hence, the diagnosis could be encephalomyelitis. The patient was treated with intravenous methylprednisolone 1 g/ day for 3 days and followed by oral prednisolone 1 mg/kg/day and intravenous acyclovir 30 mg/kg/day divided three times per day for 2 weeks. Intravenous antibiotics were used to treat sepsis and urinary tract infection. She had partial neurological improvement from the second day of admission until 10th day of admission. Then, she developed another sepsis episode which leaded to septic shock and death on 11th day of admission. Unfortunately, we were not given consent to perform an autopsy.
Neurological complications secondary to chicken pox is rare. It may occur during or after rash eruption. Cerebellar ataxia, meningitis and encephalitis are much more common than isolated myelitis.3 Myelitis due to VZV infection is scarce, especially from chickenpox. It is more common in immunocompromised patients.4,5 Clinical presentation of myelitis was different between immunocompetent and immunocompromised patients. Typical presentation started with skin lesions, followed by myelopathy at the corresponding level. Some patients do not have skin lesion.4 When it comes to immunocompromised patients, especially those with AIDS or cancer, they are prone to have an atypical presentation and poorer outcome. This may be due to deeper tissue penetration of the virus with resultant myelitis, small vessel vasculopathy, ventriculits and meningoencephalitis.5,6 In immunocompetent patients, myelitis may complicate acute varicella or zoster, usually one to two weeks after the development of rash.4
The clinical recovery is variable; many immunocompetent patients improve significantly, whereas immunocompromised patients tended to have poorer outcomes. Hung et al4 reported outcomes from 31 cases of varicella zoster virus myelitis, outcomes were good (ability to walk independently or with an aid) in all of the immunocompetent and almost half of the immunocompromised patients. Those with persistent weakness presumably have greater degrees of spinal cord necrosis and neuronal loss. Unfortunately, anti-herpetic agents had no statistically significant effect on outcomes in immunocompromised patients, but could reduce mortality rate in AIDS patients.
Despite the availability of effective vaccines, VZV infection is still prevalent worldwide.8 Centers for disease control and prevention (CDC) recommends two doses of chickenpox vaccine for children, adolescents, and adults to protect against chickenpox. The vaccination is especially important for healthcare professionals and other risk groups, such as teachers, people who care for or are surrounded by immunocompromised people, residents and staff in nursing homes, inmates and staff of correctional institutions, etc.8 Children should receive two doses of the vaccine—the first dose at 12 through 15 months old and a second dose at 4 through 6 years old. For adolescent and adults, 2 doses should be given 4 to 8 weeks apart. As one of the few treatable viral infections, VZV infection should be ruled out essentially in suspicion of central nervous system (CNS) viral infection by assaying VZV DNA or antibody. Aggressive treatment with intravenous antiviral agent such as acyclovir may improve the outcome.
This case of transverse myelitis related to acute varicella infection was diagnosed through its closed temporal relation to typically chickenpox rash, the MRI findings and serum contained anti-VZV antibodies IgM.
Conflict of interest: None