Under severe mental or physical stress, elderly patients can present with chest pain and ST segment elevation despite having no significant coronary artery obstruction. This condition was described in early 1990’s, known as “stress induced cardiomyopathy” (SIC), but its underlying pathophysiologic mechanism remains unknown.1,7 Owing to a reversible course, SIC used to be viewed as a benign form of left ventricular (LV) dysfunction but more recent study indicates that SIC victims shared the same risk of death and complication with acute coronary syndrome (ACS) patients.7 We reported a 73-year-old lady who had pneumonia of right lower lung that triggered SIC and manifested with acute anterior ST segment elevation myocardial infarction-like condition. The clinical presentation, ECG changes, pathophysiologic mechanisms, treatment and prognosis have been discussed in detail.
A 73-year-old lady, presented with no known underlying disease, and experienced low grade fever, dyspnea and non-productive cough for two days. She was treated at a local clinic with some improvement but the treatment detail was not available. At 03.00 am of December, 21, 2015, she developed shortness of breath and arrived at Chandrubeksa hospital at 05.20 am. It was found that she was tachypneic (respiration rate of 36/min), hypoxic (room air O2sat was 89%) so she was later intubated. Blood pressure was high, 188/95 mmHg, and heart rate was 100/ min. Crepitation and rhonchi were audible at both lower lungs. Supine chest film showed parenchymal infiltration at right lower lung field and calcified aortic knob with mild pulmonary conges- tion (Figure 1). Her temperature was 37.5 degree Celsius, white blood cell count was 9.8 K/unit with predominant neutrophil of 88%. The platelet count was slightly low, hemoglobin was 11.6 mg/ dl and the MCV was 65.9 Fl.
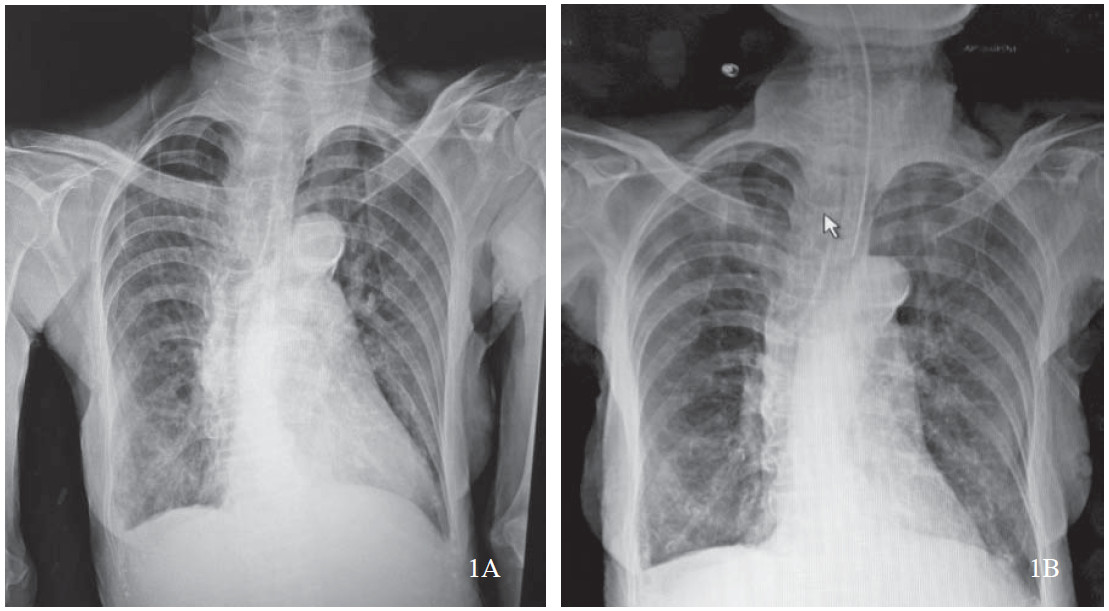
Figure 1A-B: 1A: The first chest film showed some degree of body rotation, calcified aortic knob and infiltration at right lower lung field with mild pulmonary congestion. 1B: Chest film after endotracheal intubation showed improves lung expansion, proper tube position and unchanged right lower lung lesion.
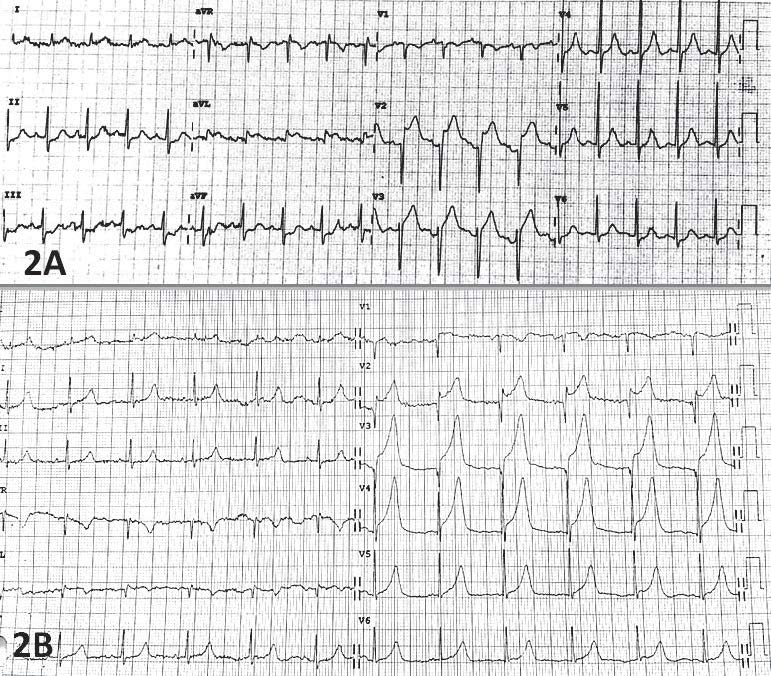
Figure 2A-B: 2A: The 1st ECG showed sinus rhythm with ST segment elevation (STE) in leads V2-3, aVL and tall T in V4, 5.It should be noted that there was no STE in lead V1 which is common in the setting of acute anterior STE myocardial infarction. 2B: Serial ECG, 7 hours after symptom onset, showed more STE in V1-4, tall T in V5-6 and the serum potassium level was normal.
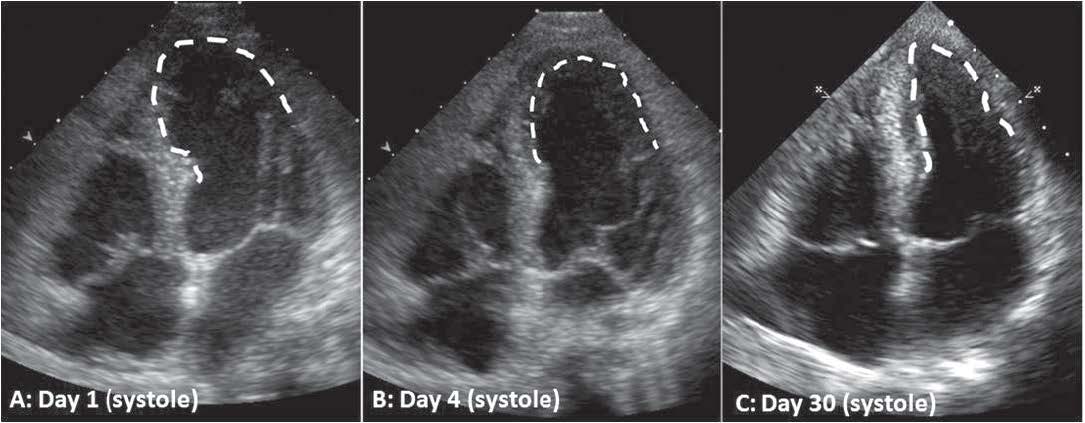
Figure 3A-C: The first echocardiogram showed an akinetic wall beginning from distal septum to apical region, causing depressed left ventricular systolic function, LVEF of 0.35. Figure 3B: Serial echocardiogram on day 4 showed markedly improved apical wall and LVEF increased to 0.45. Figure 3C: On day-30, all wall motion appeared normal and LVEF was 0.60.
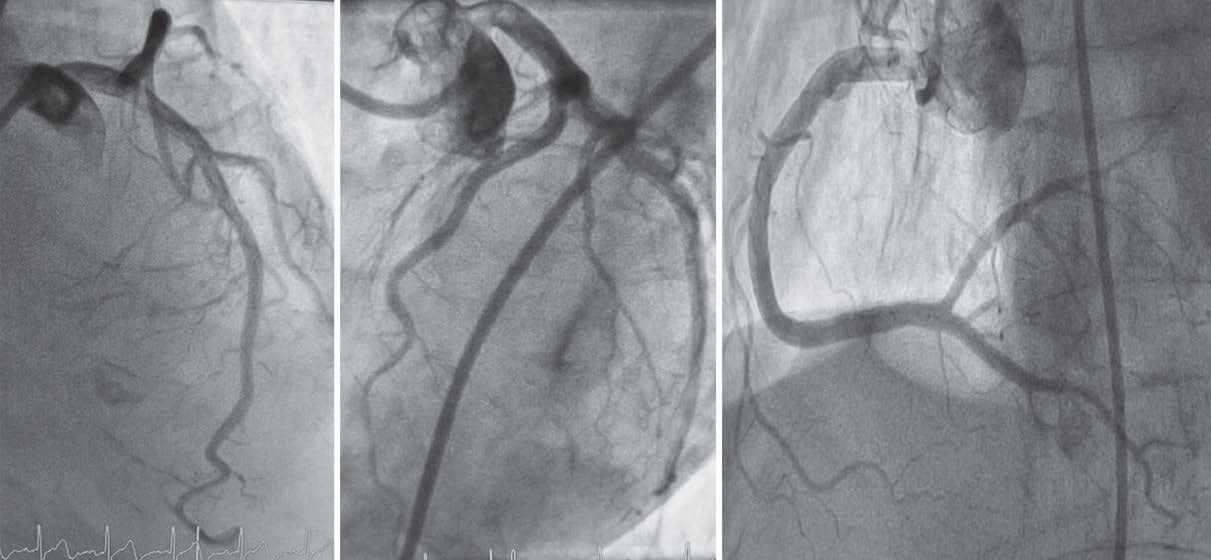
Figure 4A-C: Coronary angiogram showed no significant luminal stenosis along the left main, left anterior descending, circumflex arteries, and the dominant right coronary arteries (4C).
The first ECG at 06.22 am showed sinus tachycardia with ST segment elevation (STE) in muliple leads (V2,3,I, aVL), and relative tall T in leads V4-5. ST depression in leads III, aVF and T wave inversion in lead aVR were also noted (Figure 2A). The first troponin T (cTnT) remained within normal range. Echocardiogram showed akinesia of mid septal, apical walls and depressed left ventricular (LV) systolic ejection function, LVEF of 0.36 (Figure 3A). These findings suggested the diagnosis of an acute evolving anterior wall ST segment elevation myocardial infarction, in addition to pneumonia and possible iron deficiency anemia. Owing to the large ischemic area, the team referred her to the emergent cardiac catheterization laboratory at Bhumibol Adulyadej hospital. Aspirin, clopidogrel, intravenous heparin and ceftriazone were given before transfer.
After risks and benefits were explained and informed consent was obtained, coronary angiography was per- formed through right femoral artery, under local anes- thetic drug. It was found that the LM trunk, circumflex and right dominant coronary arteries were all unob- structed and the contrast flow was normal. The left an- terior descending artery was patent and had only mild luminal irregularity with no significant lesion (Figure 4). The left ventricular diastolic pressure (LVEDP) was high, 32 mmHg and was compatible with an elevated serum NT-PRO BNP, 3,520 pg/ml. The diagnosis was then changed to stress-induced cardiomyopathy (Takotsubo) causing heart failure and the patient was medically treated in the coronary care unit.
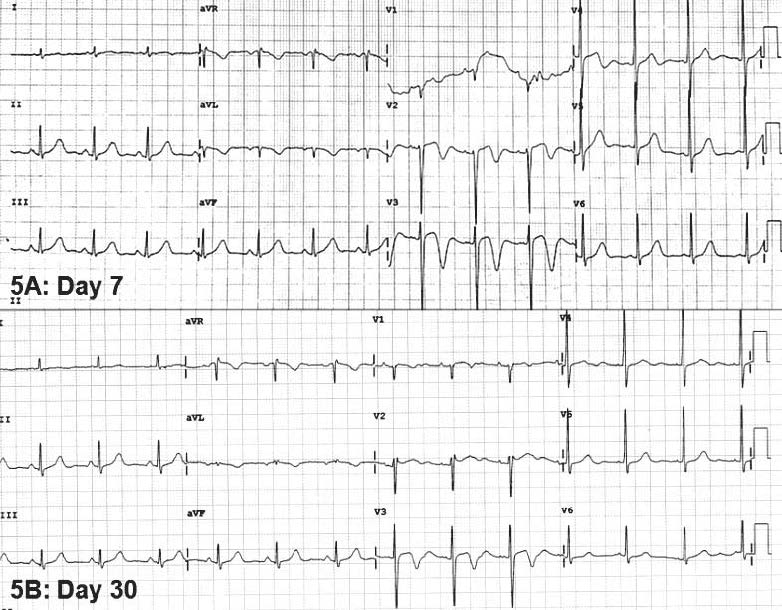
Figure 5A, B: Serial ECG showed and resolution of precordial ST segment elevation and T inversion on day-7 and day-30 with no Q wave development.
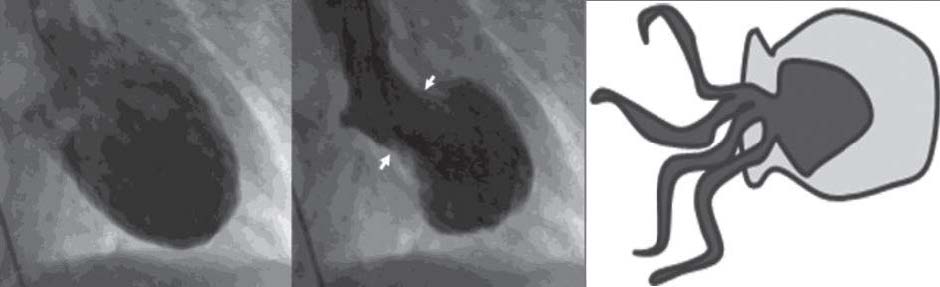 Figure 6A, B, C: left ventricular diastole of another case. Figure 6B: apical ballooning during systole. Figure 6C: Japanese octopus pot.4
Figure 6A, B, C: left ventricular diastole of another case. Figure 6B: apical ballooning during systole. Figure 6C: Japanese octopus pot.4
With antibiotic and diuretic treament the patient was clinically improved and was extubated within 72 hours. Although blood culture remained with no growth observed, sputum culture was positive for pseudomonas aeruginosa andthesensitivedrug, ceftazidime, wasstarted. Thethyroid function test was within normal range. Despite the second rise of hs-cTnT to 236.7 (normal < 14 ng/L), subsequent ECGs illustrated resolution of elevated ST segment with no Q wave development (Figures 5A,B). Serial echocardio- gram on day 4, showed improved LV systolic function and apical wall motion with LVEF of 0.45 (Figure 3B). She was discharged in one week and did well. On follow-up, day-30, all wall motion appeared normal and LVEF was 0.60 and there was no apical thrombus noted, see Figure 3C.
Takotsubo, reversible stress-induced cardiomyopathy (SIC)
In 1990, Sato and colleagues reported a group of Japanese patients, mostly post-menopausal women, who had emotional stress and developed transient apical akinesia without significant coronary obstruction.1 The term “Tako-tsubo” (fishing pot to capture octopus) was used to describe the shape of left ventricular (LV) apex that balloons out during systole, relative to normal contractile basal part, see Figure 6B. Since then, this unique syndrome has been recognized worldwide under various names, including transient apical ballooning syndrome, stress-induced cardiomyopathy (SIC), broken heart syndrome, adrenergic cardiomyopathy, Takotsubo cardiomyopathy.2-6 Although apical ballooning is the most common finding (81.7%), other forms of wall motion such as mid ventricle (14.6%), basal (2.2%) and focal type (91.5%) are also reported.7
Because of its reversible nature, SIC was initially considered a benign condition. SIC predominantly affected female (80%) elderly patients (age ranges from 61-76 years), who had prior emotional or physical stress.2-6 Recent data from the international registry of 1,750 takotsubo cases (collecting from 25 heart centers of 9 countries, during 2011-2014), confirms the same age and sex distribution. The majority of SIC patients are still women (89.8%) with a mean age of 668 years and the two most common presentations are chest pain (75.9%) and dyspnea (46.9%).7
Stress-induced cardiomyopathy (SIC) vs acute coronary syndrome (ACS)
Data from the sex and age matched cohort study of 455 SIC and 455 ACS cases shows no statistical difference in age, sex distribution, median troponin level, systolic blood pressure, cathecholamine use, cardiopulmonary resusci- tation, cardiogenic shock and death, between these two syndromes.7 Owing to the overlapping age range, presenting symptoms, ECG changes, abnormal wall motion and troponin T leakage, it is quite challenging to differentiate SIC from acute coronary syndrome (ACS) cases.2-7 In addition, SIC is not a benign syndrome since its complication and mortality rates are not different from ACS cases.7
By analyzing ECG, ACS cases trends to have more STE (51.2% vs 44%, p = 0.03), and ST depression (31.1% vs 8.3%, p < 0.001). Konsuge and colleagues observed that the ST depression in lead aVR and the absence of STE in lead V1 supported the diagnosis of SIC, with the sensitivity and specificity of 91% and 96% respectively.8 Our case did not have ST depression in aVR but there was no STE in V1 (Figure 1A) and no Q wave development on the serial ECG (Figure 5A, B) which would be expected in acute anterior wall myocardial infarction cases.
In practice, like our case, performing a coronary angiography is mandatory to diagnose SIC and to exclude ACS. However, concomitant but not relevant coronary artery disease can be found in 21% of SIC patients.7 In comparison to ACS cases, SIC victims had more abnormal left ventricular systolic function (LVEF 40.7 vs 51.5%,p < 0.001) and diastolic dysfunction (LVEDP 22.1 vs mmHg, p = 0.001).7 Despite having the worse systolic (LVEF of 0.35) and diastolic dysfunction (LVEDP of 32 mmHg), our case recovered well within 72 hours.
Pathophysiology
The underlying mechanism of SIC has remained unclear for the past 25 years. Three major mechanisms have been proposed: 1) vasospasm of epicardial artery, 2) acute coronary microvascular dysfunction causing ischemic myocardial stunning and, 3) cathecholamine mediated direct myocardial injury and stunning.9 Multi-vessel coronary spasm had been reported in 5 apical ballooning cases but this finding was quite rare, only 1.2% among 415 ACS cases.10 In addition, spasm could be a secondary symptom resulting from administration of epinephrine in SIC patient who presented with bradycardic arrest.11 Although abnormal myocardial perfusion defects have been reported in the affected wall of SIC cases,12,13 the precise role of coronary microvascular dysfunction is not yet established.9
Recent data suggested the role of stress-induced cathecholamine mediated myocardial injury. First, data from an international study7 indicated that two-thirds (63%) of SIC cases had physical (36%) or emotional stress (27.7%) and only one third had no stress (28.5%). Second, SIC was associated with several stress condi-tions including pheochromocytoma,14 sepsis, non-cardiac surgery, bronchial asthma exacerbation, Guillain-Barre’ syndrome,15 subarachnoid hemorrhage (SAH),16 acute ischemic stroke,17 head injury,18 psychiatric illness19 and electro-convulsive therapy.20 For example, 20-30% of SAH victims had reversible LV wall motion abnormalities in the absence of coronary obstruction.21 In addition, SIC victims had higher prevalence of psychological or neurological disorders than ACS cases, 55.8% vs 25.7%, p < 0.001.7. Of those, 27% of SIC cases had either acute or chronic neurological disorders, 42.3% had psychiatric illnesses and half of these were affective disorders.7 All of these stress conditions might create a significant amount of stress hormone such as cathecholamine for the develop- ment of SIC. In our reported case, the most likely physical stress that triggered SIC was pneumonia.
Third, high levels of the stress hormone and devel- opment of SIC has been documented. Wittstein and colleagues found that the level of cathecholamine and its metabolites in SIC victims from sudden emotional stress were 2-3 times higher than those of acute myocardial infarction cases who had a similar degree of heart fail- ure.22 Cherian J and colleagues23 reported the first fatal apical ballooning during dobutamine stress test in an 85-year-old lady who had planned hip surgery. After given 40 μg/min of dobutamine, her heart rate reached 91% of age predicted maximal heart rate. During recovery, the patient developed chest pain, STE in inferior and lateral wall and apical ballooning with systolic anterior motion of anterior mitral valve leaflet, causing LV outflow track obstruction and low cardiac output. Coronary angiogram showed no evidence of coronary obstruction. Despite administration of beta-blocker, the patient developed pulseless electrical activity and expired.23 Lastly, the histology from cardiac biopsy in SIC victims and patients died from epilepsy and subarachnoid hemorrhage shared the common feature of contraction band necrosis (myocy- tolysis) which was known as cathecholamine toxicity.9,24 Molecular mechanisms of SIC was studied in rat models.25 After induced emotional stress, rapid activation of p44/p42 mitogen-activated protein kinase was observed in the heart, followed by transient up-regulation of genes in smooth muscle and endothelium cells of coronary arteries, induction of heat shock protein 70 in the aorta, coronary arteries, myocardium and up-regulation of natriuretic peptides gene. The author concluded that activation of alpha and beta adrenoreceptors were the primary trigger of emotional stress-induced molecular changes in the heart.25
Treatment and prognosis
Data from the latest SIC registry7 showed that only angiotensin converting enzyme inhibitors (ACEI) and angiotensin receptor blockers, but not beta-blockers, were associated with good outcomes. In addition, SIC victims shared similar in-hospital complications with ACS patients, including cardiogenic shock (12.4 % vs 10.5%, p = 0.39) and death (3.7% vs 5.3%, p = 0.26). Other severe SIC complications were ventricular tachycardia (3%), intra-ventricular thrombus (1.3%) and ruptured ventricle (0.2%).7 The types of SIC had no influence on complications. Older age and emotional stress are good prognostic predictors, while younger age, male gender, physical stress either neurological or psychiatric disor- ders, high initial cTnT above 10 times of upper limit and low LVEF < 0.45 were associated with high complication rates.7 The 30 days major adverse outcomes of SIC including death, stroke or TIA were 7.1% and men had more adverse events than women, 13.7% vs 6.3%, p = 0.002).7 Although our case had some bad predictors such as physical stress (pneumonia) and lower LVEF (0.35), she also received ACEI late (on day 3) but recovered well. The good prog- nostic factors in this case were an elderly female patient with an initial negative troponin.
Stress-induced cardiomyopathy (Takotsubo, SIC) is a transient ventricular systolic and diastolic dysfunction in the absence of relevant coronary artery obstruction. With the overlapping age range, STE, apical akinesia, depressed LV systolic and diastolic function, it is mandatory to perform coronary angiography to rule out ACS. We reported a 73-year-old woman who developed SIC after having pneumonia of the right lower lung. Although our case recovered well within 72 hours, most SIC patients from the registry study shared the same in-hospital complications as ACS cases including cardiogenic shock, ventricular dysrhythmia, stroke and death. Current data has suggested the role of stress-induced catecholamine mediated myocardial injury. We hope that this case will raise clinical attention among colleagues to promote the early detection and successful treatment of this potentially fatal condition.