Pilomatricoma is a benign subcutaneous neoplasm having a propensity to occur in the head and neck region in children. Originally, it was thought to be of a sebaceous gland origin and was named “Calcifying Epithelioma of Malherbe” in honor of Malherbe and Chenantias who first described the lesion in 1880.1Later more investigations revealed that this neoplasm was derived from hair follicle cortex cells, and subsequently it was renamed “Pilomatrixoma” by Forbis and Helwig in 1961.1 Based on this etymology, this neoplasm is now called “Pilomatricoma”.
The objective of this article is to report an additional case of pilomatricoma of the cheek in a 14-year-old Asian child, displaying an unusual histopathologic feature and to provide a relevant discussion of the head and neck pilomatricoma.
A 14-year-old Asian female presented at the dental clinic for evaluation of an asymptomatic mass of her right cheek of several years’ duration. The child’s parent reported the slow growing mass had been present since a young age, which the child was not disturbed by. Clinical examination revealed an oval shaped, 1 x 1 cm2 mass with normal appearing overlying skin at the right mid-cheek. On palpation, the mass was hard, but not tender. Intraoral examination revealed an oral mucosa within normal limits. An oral surgeon performed a surgical excision of the entire lesion and observed that this non-encapsulated mass was located in the subcutaneous layer of the skin. The clinical impression provided by the clinician was of a non-specific “calcified mass from right buccal mucosa”. The specimen was submitted to the department of Oral Pathology for histological evaluation. Microscopic examination revealed a well-defined lesion consisting of irregular islands and sheets of keratinized ghost cells juxtaposed with peripheral ossification (Figure 1A and 1B). These islands and sheets were occasionally surrounded by foreign body type multinucleated giant cells. The supporting stroma contained abundant large foamy cells and adipose tissue (Figure 1C). Immunohistochemical investigation of sections of the specimen was performed using antibodies against CD68 to confirm the origin of the foamy cells. Diffuse CD68 positivity of moderate intensity was observed in the foamy histiocytes (Figure 1D). Based on these results, a final diagnosis of pilomatricoma was made. At a 3-year follow-up, there was no evidence of recurrence.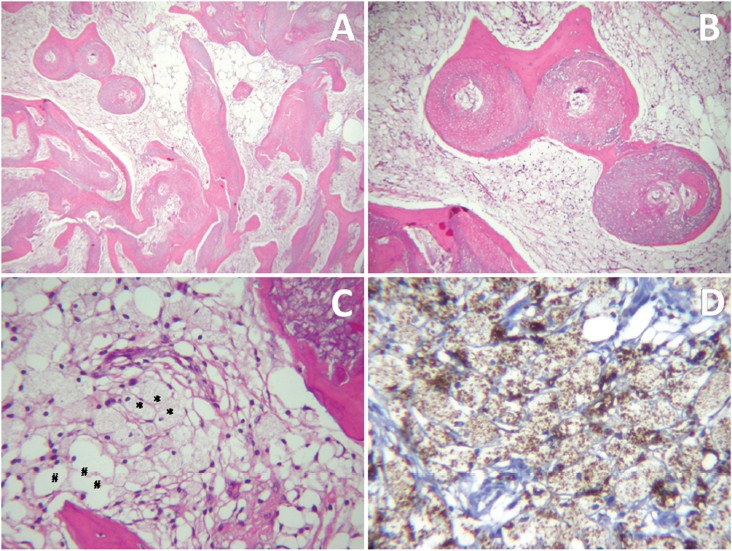
FIgure 1A-D: Histopathology
A: Low-power view of the specimen displaying irregular islands or nests of ghost cells with peripheral ossification within the loose fibrous stroma and adipose tissue.
B: Medium-power view of the lesion consisting of nests of eosinophilic shadow cells with lack of nuclei in the central portion, surrounded by ossification.
C: Photomicrograph of supporting tissue composed of abundant foamy cells (#) and adipocytes (*) (high power view).
D: Immunohistochemical staining for CD68 showing diffuse reactivity of moderate intensity in foamy cells confirming a histiocytic origin.
Pilomatricoma is an uncommon benign skin neoplasm, accounting for 0.12% of all cutaneous neoplasms.2,3 The head and neck region is the most frequent location for pilomatricoma (ranging from 40% to 77% of the reported cases), followed by the upper extremities, trunk and the lower extremities.3-7 Head and neck pilomatricomas involve frontal, temporal, cheek, periorbital, periauricular, and cervical regions.2,8 Some reports found the cheek is the most commonly involved location (ranging from 27% to 34%).5, 6 The majority of head and neck pilomatricomas are encountered in the first and second decades of life.3-9 Some authors have reported a bimodal peak with a second peak occurring during the sixth and seventh decades of life.9 Nevertheless, there is a steady decline in the frequency of pilomatricoma with advancing age.8 Gender and racial predilection for this lesion varies, depending on the geographic locations of the studies.3,5,8 The molecular pathogenesis involved in development of pilomatricoma has been reported to include overexpression of antiapoptotic protein BCL-2, mutations in gene CTNNB1 resulting in LEF-1 (the downstream transcription factor in WNT signaling) transactivation, and expression of hHB1 (human hair keratin basic1).10
Clinical presentation of this neoplasm is characterized by an asymptomatic slowly growing mass, hard in consistency, with intact overlying skin, occasionally displaying a bluish discoloration.3,8,9 The case presented here had a typical clinical presentation of pilomatricoma. However, due to the rarity of head and neck pilomatricomas cases reported in medical and dental journals, dental professionals may fail to include this entity in their clinical differential diagnoses. Generally, the clinical differential diagnosis of a bluish swelling in the head and neck region of a child should include vascular anomalies, developmental cysts, parotid neoplasms, and inflammatory lesions.9 However, pilomatricoma should also be considered in the list of clinical impression possibilities.
Diagnostic tools including radiographs and fine needle aspiration have been implemented to provide a provisional diagnosis in several cases. However, they fail to reveal the pathognomonic features of pilomatricomas. Submission of surgical specimens for histologic examination is required to disclose a definitive diagnosis.
Pilomatricoma evolves histopathologically through four stages including early, fully developed, early regressive and late regressive stages. These stages reflect the development of this tumor from an infundibular matrix cyst to a calcified and ossified nodule with complete absence of epithelial component.1 Pilomatricoma has a typical histopathologic presentation, characterized by an encapsulated mass consisting of two cell types; basophilic cells and ghost cells arranged in irregular anastomosing sheets or islands within a background of fibrous stroma. The basophilic cells are seen to have scant cytoplasm, indistinct cell margins, and round or intensely elongated basophilic staining nuclei. The ghost cells have sharp cell margins, faint eosinophilic cytoplasm, and a central unstained area representing the lost nucleus. Mixed cell population of basophilic cells and ghost cells were evident in most cases in one report.8 However, some cases have been reported with a histological appearance of ghost cells alone.8 Variable degrees of stromal foreign body giant cell reaction, keratin deposition, calcification, melanin deposition, or ossification may be seen in this tumor.8 The case here displayed characteristic histological features resembling reported cases. An absence of basophilic cells was noted in our case and it is possible they had undergone ossification, presumably evolving into a late regressive stage tumor. Interestingly, the presence of a tremendous amount of CD68 positive cells, foamy histiocytes, was observed in our case. Evidence of a histiocytic reaction has not been reported previously in benign pilomatricoma.
The histologic differential diagnosis of pilomatricoma should include other neoplasms demonstrating shadow cells or ghost cell formation, including basal cell carcinoma, neuroendocrine carcinoma, and calcifying odontogenic cyst. Its malignant counterpart, pilomatrical carcinoma, also should be considered.
Basal cell carcinoma is a common malignant skin tumor, with diverse histological variation. The shadow cells, which are characteristic of pilomaticoma, can be seen in the type of metrical differentiation. However, evidence of minimal anaplastic basaloid cells arranged in palisades at the periphery, artificial retraction spaces between tumor cells, and connective tissue stroma are present in basal cell carcinoma.11
Neuroendocrine tumors also contain ghost cells in some cases. The typical presentation of a neuroendocrine tumor shows an organoid arrangement of relatively uniform tumor cells, with nesting, trabecular, or lobular growth patterns. Tumor cells demonstrate finely granular chromatin, inconspicuous nucleoli, and abundant neurosecretory granules in the cytoplasm. While atypical variants, or cases of neuroendocrine carcinoma, may show tumor necrosis with ghost cells, areas of neuroectodermal differentiation with immunoexpression of neuroendocrine markers must be identified.12
Gorlin and his colleagues described the calcifying odontogenic cyst as having a distinct microscopic resemblance to, and that it may be an oral analog of, pilomatricoma. Calcifying cystic odontogenic tumor, previously named calcifying odontogenic cyst, is a benign cystic neoplasm of odontogenic origin occurring in the oral region, characterized by solid masses or cystic lesions lined by proliferative epithelium resembling ameloblastoma, with the formation of ghost cells in the suprabasal epithelium. Focal calcification in these lesions is frequently observed.13
The malignant counterpart of pilomatricoma, pilomatrical carcinoma, is characterized by an abundant proliferation of basaloid cells with cell masses scattered throughout the tumor. The tumor cells have an infiltrative growth pattern and penetrate into the deeper portion of the tumor. Varying degrees of cytologic atypia, frequent mitoses, and areas of necrosis differentiate this tumor from pilomatricoma.10 Surgical excision is the treatment of choice for pilomatricoma. The prognosis for this lesion is considered to be quite good with a relative low recurrent rate ranging from 1.12% to 3%.3,5 Malignant transformation in a previously diagnosed pilomatricoma has been reported in a few cases.3,8
We have presented a rare report of the presentation, surgical treatment, and histological diagnosis of a pilomatricoma observed in the cheek of a 14-year-old Asian female, in the hope that this report will aid other clinicians in their future diagnosis of such lesions.
The author thanks Dr. Kevin Tompkins for the assistance in manuscript preparation.