Acute Coronary Syndrome (ACS) is the consequence of atherosclerotic plaque disruption with thrombus formation and significantly increasing different degrees of coronary artery occlusion. Using clinical features, electrocar-diogram and cardiac biomarker (troponin), ACS can be divided into
Figure 1 summarizes ACS pathophysiology, and clinical features. Note that STEMI is the only condition that the infarcted artery is usually completely occluded (acutely)
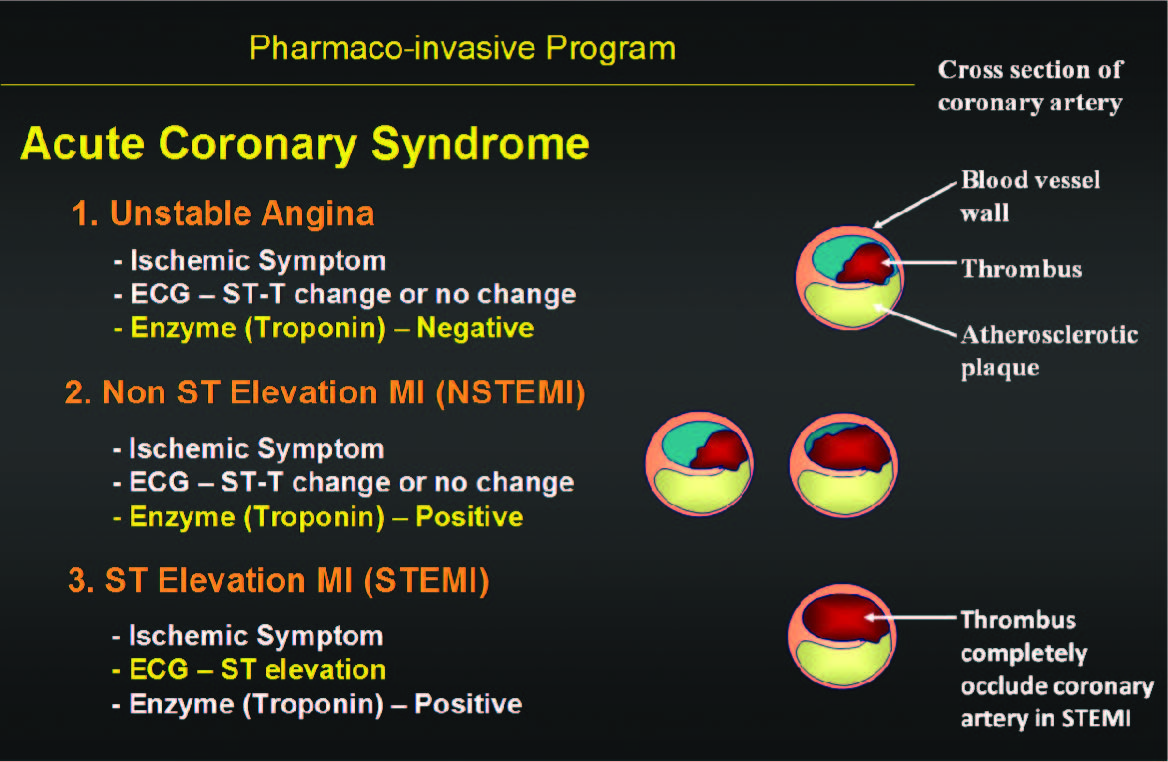
Figure 1: ACS, Pathophysiology, Clinical Features
The management goal of STEMI is to reperfuse the infarct occluded coronary artery as soon as possible, to reduce myocardial cell death as much as possible.
1. Thrombolysis with thrombolytic agents.
The advantage of thrombolysis is its ready availability in most hospitals that have full emergency services and that it can be admin- istered in a short period of time. The disadvantages of thrombolysis are lower initial successful rate and higher re-occlusion rate, when compared with PCI.
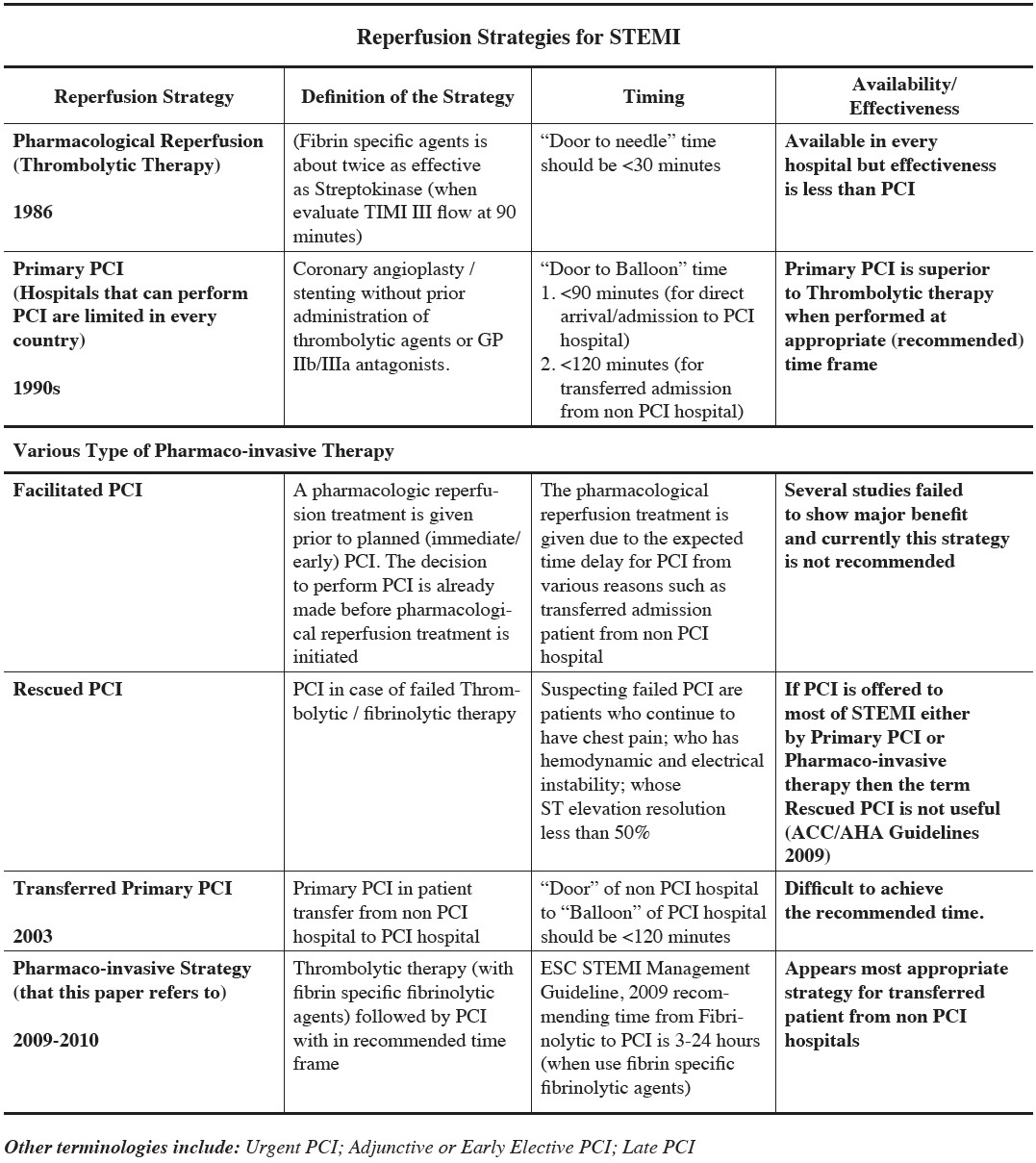
Table 1: Lists the various PCI terminologies and their definition, timing and effectiveness.
2. Percutaneous Coronary Intervention (PCI).
PCI is only available in a small number of all hospitals in any country (about 25% in US). It has high successful reperfusion rate but this technique requires a longer period of time to deliver, particularly if the patient has to be transferred from non PCI capable hospital.
Early on, thrombolysis and primary PCI strategies were considered separately and appeared to compete with each other. They both have advantages and disad-vantages points as aforementioned. In the past 25 years, there has been extensive research to find out which single or combination of strategies works the best and for what situation.
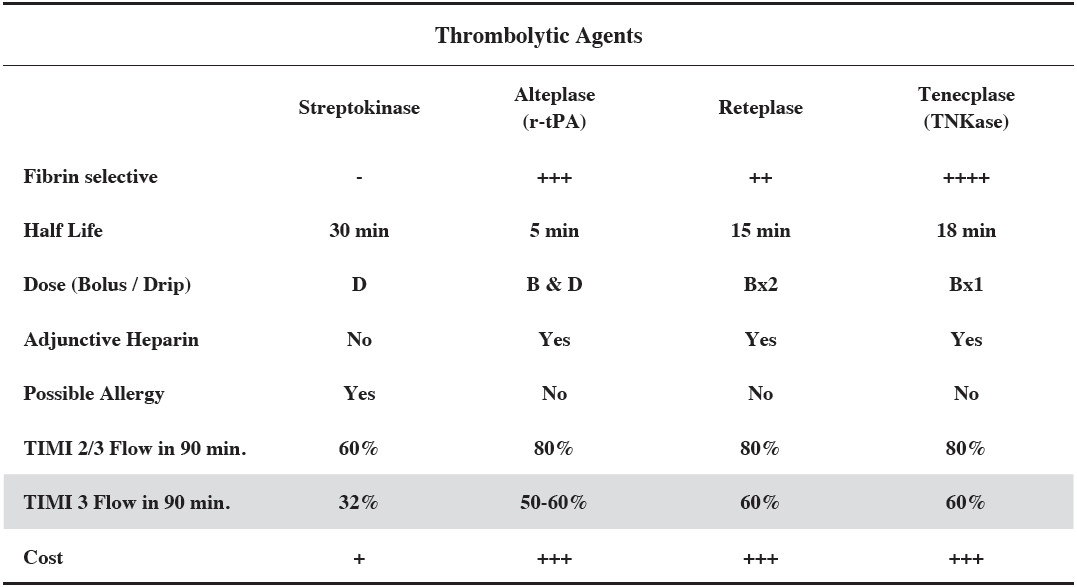
Table 2. Thrombolytic Agents.Note that streptokinase is only half as effective as those fibrin specific products when look at TIMI 3 flow (normal coronary artery blood flow) by coronary angiogram at 90 minutes following thrombolytic administration.
Evolution of reperfusion therapy for STEMI can be summarized into 4 periods. Any one of these strategies are still being utilized depending on the situations. It is expected that the practice guidelines will change further for this dynamic condition. Pre hospital thrombolysis is not included in this article.
1. Thrombolytic therapy (1986).
Streptokinase was the thrombolytic agent most used in reperfusion therapy for STEMI early on. It has since been replaced by fibrin specific products which are more effective (Table 2). The current popular agent is Tenecta- plase (TNK), a fibrin specific thrombolytic agent which is easy to administer. Because of its lower cost, despite lower efficacy, streptokinase is still being used in coun- tries with less financial resources, including Thailand.
Thrombotytic therapy is more effective if it can be given within 3 hours after the onset of symptoms such as chest pain. We have not yet been able to shorten up the time from chest pain onset to the time of first medical contact (FMC). We should be able to control the time from FMC to the time of delivering the thrombolytic agent which was recommended to be “Door to Needle” time is
2. Primary PCI (1990s).
Primary Percutaneous Coronary Intervention therapy has been performed since early-mid 1990s. Primary PCI is the therapy to open the infarct occluded coronary ar- tery with angioplasty and stent placement without pre- ceding thrombolytic therapy (See Table 1. for various PCI terminologies and their definition, timing and effec- tiveness)
Recommended median time for Primary PCI is < 90 minutes from FMC to infarct coronary artery open. The so-called “Door to Balloon” time is < 90 minutes. Primary PCI has better results than thrombolysis when both approaches are performed with in the recommended time frame. Early data has been collected exclusively from direct arrival/admission patients.
3. Transferred Primary PCI (2003)
Refers to Primary PCI therapy in which the patient transfers from first hospital to PCI capable hospital. Rec- ommended median time for transferred primary PCI is < 120 minutes from FMC (of the first hospital) to in- farct coronary artery open (of the PCI hospital). This recommended time is hard to achieve even in developed countries (Figure 2 for US) with better transport systems available. However there were more than 30 % of the patients that could achieve this timeline (NCDR 2005- 2006) suggesting that not only is the shorter distance between the two hospitals important but also the devel- opment and execution of the proper protocol is necessary to help the achievement of this goal.
Transferred Primary PCI is not suitable (or not pos- sible) in the locations or countries with slow transporta- tion time (for whatever any reason).
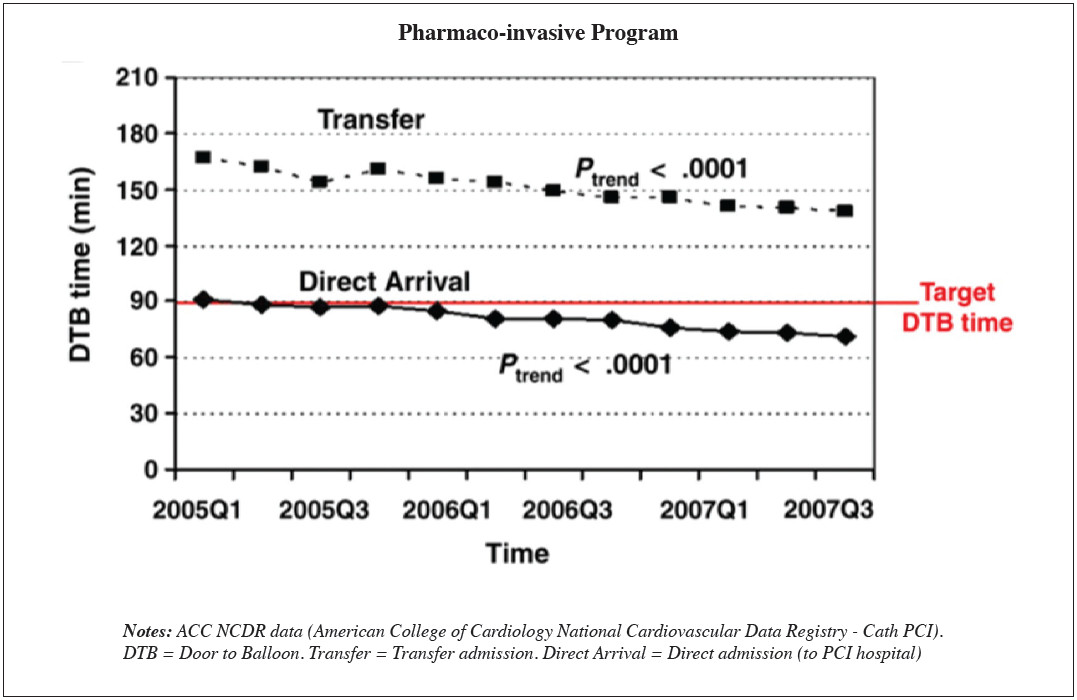
Figure 2: Graph shows US median Door to Balloon time is now about 70-80 minutes for “Direct arrival/admission patients”.However median time for Door (First medical contact of the first hospital) to Balloon ( CI hospital) for transferred patients is still over 140 minutes.
4. Pharmaco-invasive approach (2009-2010).
To off-set the time delays in transferred patients the researcher has combined the quickness and ready avail- ability of thrombolytic (pharmaco) therapy and the delayed but complete reperfusion of PCI (invasive). There have been few approaches with different terminol- ogies, timing between the two strategies, and different clinical set up (Table 1).
Facilitated PCI failed the test likely due to a too short period from thrombolysis to PCI. Immediate PCI afte fibrinolytic therapy causes significant increase in mor- tality, nonfatal reinfarction, urgent target lesion revascu- larization and stroke and a trend toward a higher rate of major bleeding.
The pharmaco-invasive therapy in this paper in particular, refers to the technique whereby there is a time elapse of 3-24 hours between thrombolysis (pharmaco) and PCI (invasive) when using fibrin specific thrombo- lytic agents. This approach has been endorsed by the most recent guidelines of both ESC and ACC/AHA. Whether or not there should be a greater time delay (>3 hours) when using streptokinase is not yet known.
The pharmaco-invasive strategy appears most suitable for Thailand or similar countrie or similar situations. There should be sufficient time for trans- ferring the patient (does not have to be within 3 hours or more) and sufficient time to perform PCI with in 24 hours. Door to needle of the first hospital (PCI non capable) should remain the same ()
Recommendations for Pharmaco-invasive therapy as follows:
Brief