Back pain is second only to the common cold as the most frequent reason for seeing a physician. Low back pain is experienced by most individuals, with 70 to 80% of the world’s population experiencing low back pain sometime during their lives.1
An international comparative study by Cherklin DC, et al showed the rate of back surgery in the United States was at least 40% higher than in any other country and was more than five times that of England and Scotland. Back surgery rates increased almost linearly with the per capita supply of orthopedic and neurosurgeons in the country. These findings illustrate the potentially large impact of health system differences on rates of back surgery.2
Surgical goals are improvements in pain, functional status and quality of life. It is well known that some patients operated on for spinal disorders will have a poor result, regardless of the apparent technical success of the operative procedure itself.3 This has prompted the search for risk factors and the development of pre-screening tools to assist with both the patient selection procedure and the promotion of realistic expectations on behalf of the patient.4-6 In order to make the correct diagnosis, Bangkok Spine Academy (BSA) always focuses on the history of medical illness and a thorough physical examination of all patients. We follow the Joint Clinical Practice Guidelines from the American College of Physicians and the American Pain Society for diagnosing and treating Low Back Pain.7
The BSA had 2,994 low back pain patients in 2010 and 223 (7.44%) underwent surgery. BSA has begun to develop a spine registration for patients who underwent lumbar spine surgery in order to study patient’s history, population, epidemic, quality of life and ability to perform daily activities. The analysis of this information will help us to improve our care and treatment of our patients.
Currently, there are several assessment tools used to measure the treatment results of patients who undergo lumbar spine surgery. Oswestry Disability Index (ODI) is an internationally accepted measure for spine disability and is used in most if not all spinal treatment result assessments. Additional measures are also used to supplement the ODI in order to fully define the patient’s spine condition; commonly used questionnaires include the SF-36, SF-12 and the Euro Quality of Life (EuroQol). Therefore we decided to utilize the ODI and EuroQol8 with our prospective surgery candidates as a pre-screening procedure and so we could also have effective tracking of the patient’s improvement on follow up. The following data then shows the pre-operative state of our patients, using the abovementioned measures.
Sample Size
The focus of this study is the 223 (out of 311 lumbar spine) patients treated with surgery at BSA between August 2010 and June 2011.
EuroQol
Pre-operative measurements of mobility, self-care, activities of daily life, pain, and anxiety and/or depression were determined by EuroQol using visual analogue scale (VAS) and 5 Dimensions (5D).9
The EuroQol Visual Analogue Scale (EQ-VAS)
The EQ-VAS is a part of the EuroQol Questionnaire. The patients rate their current health state on the line, which ranges from 0 - 100 (The worst to the best imaginable health).10
Oswestry Disability Index (ODI)
ODI versions with a scale ranging from 0-5 were used. Questionnaires addressing 10 common activities were administered, using both English and validated translations into other languages. Points were added up each section and plugged in to the following formula in order to calculate the patient’s level of disability:
Point total / 50 x 100 = % disability (aka: ‘point total’ divided by ‘50’ multiply by ‘ 100 = percent disability).11,12
In Thai patients the authenticated Thai ODI was used; in non-Thai speaking patients, the English ODI (version 0.1) was used.13
Thai score
In a study of the quality of life of Thai people across the country, using the EuroQol questionnaire, the formula to calculate the quality of life of Thai people was called Thai score.
Thai score = 1-0.202-(0.121*mo)-(0.121*sc)-(0.059- ua)-(0.072*pd)-(0.032*ad)-(0.190*m2)-(0.065*p2)- (0.046*a)-(0.139*N3).14
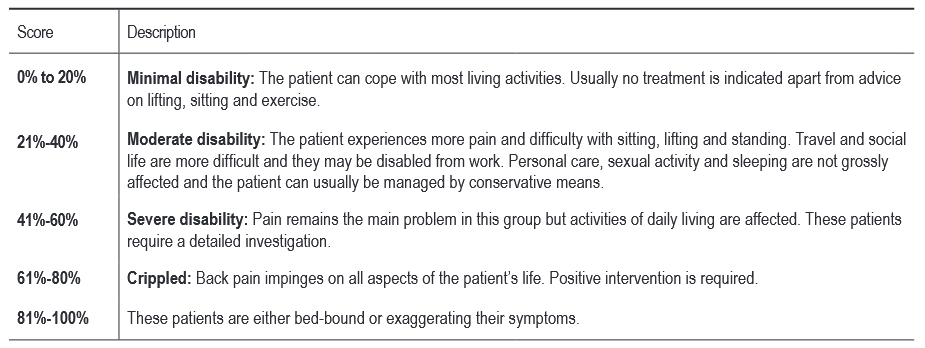
Table1: Interpretation of scores
SPSS Data Analysis
This descriptive statistic is used to analyze demographic data. EuroQol-5D is composed of five dimensions (mobility, self-care, usual activities, pain/discomfort and anxiety/depression). Each dimension has 3 levels: no problem, some problem, extreme problems.15 The ratings in the different possible health states will be transformed into an index value. We decided to adapt this and say that each dimension has two levels of severity: No problem and problem. No problem states were those rated the health as full health (all dimensions rated as 1). The problems which were proportionally ranked from 1-3 were analyzed.
Patients who filled out a questionnaire asking them to respond to questions in their native language before undergoing a surgical procedure at BSA between August 2010 and June 2011.
Patient population
Baseline parameters and patient data are presented in Table 2. The majority of patients, 169, or 75.78% were Thai. The proportion of males to female was male 129 (57.8%) female 94 (42.2%). Fifty-seven patients (25.6%) were in the age range of 51-60. Mean ± SD age of patients was 53.69 ± 15.62, minimum 20, and maximum 88. Eighty six patients (38.6%) had a body mass index range 25.1-30; Mean ± SD Body mass index was 26.28 ± 6.11, minimum 18.03, maximum 45.70. Two hundred and one (201) patients (94.6%) were non-smokers. Duration of pain for acute pain 127 (56.95%) Mean ± SD 44.60 ± 29.66, minimum 5 days, maximum 90 days and for chronic pain 96 (43.05%) Mean ± SD 733.70 ± 841.46 minimum 120 days, maximum 3,650 days. Fifteen (6.72%) of patients had previously undergone back surgery in the past. 96 patients (38.56%) had underlying diseases. Surgical procedures were categorized into five groups: Lumbar decompression with Fusion 64 (28.7%), Lumbar decompression without Fusion 76 (34.1%), Lumbar Microdiscectomy 68 (30.5%), Total Disc Replacement 1 (0.4%) and Mixed procedures 14 (6.3%) of the cases.
Mobility: Pre-operative 157 (92.9%) had problems, 12 (7.1%) had no problems. Self-care: Pre-operative 97 (57.4%) had problems, 72 (42.6%) had no problems. Usual activities: Pre-operative 157 (92.9%) had problems, 12 (7.1%) had no problems. Pain/discomfort:BPre-operative 167 (98.8%) had problems, 2 (1.12%) had no problems. Anxiety/depression: Pre-operative 137 (81.1%) had problems, 32 (18.9%) had no problems. (See Table 3 for more details)
The EQ Visual analog scale is presented in Table 4. Total patients pre-operative 223 cases, report EQ Visual analog scale Mean ± SD 50.25 ± 16.65, Median 50, 25th percentile 40, 75th percentile 60.
EQ-5D dimensions (Thai score). Thai patients preoperative 169 cases, report EQ-5D dimensions Mean ± SD 0.488 ± 0.151, Median 0.452, 25th percentile 0.45, 75th percentile 0.57. Lumbar decompression without Fusion 0.468, Lumbar Microdiscectomy 0.483, Lumbar decompression with Fusion 0.503 and Mixed procedures 0.536 respectively presented in Figure 1.
EQ-VAS (Thai score index). Thai patients pre-operative 169 cases, report EQ-VAS Mean ± SD 50.592 ± 16.501, Median 50, 25th percentile 40, 75th percentile 60. Lumbar Microdiscectomy 46.9, Lumbar decompression without Fusion 50.741, Lumbar decompression with Fusion 50.304 and Mixed procedures 50.333 respectively presented in Figure 2.
Oswestry Disability Index Score Of the 223 preoperative patients. Reported scores were: Mean ± SD 32.58 ± 21.60, Median 32, 25th percentile 12, 75th percentile 48. Mixed procedures 46.51, Total disc replacement 34, Lumbar Microdiscectomy 34.37, Lumbar decompression with Fusion 33.82 and Lumbar decompression without Fusion 27.34 respectively presented in Figure 3.
Our patients’ages ranged from 20-88. Seventy-five percent (75%) were Thai and 25% were non-Thai. Both groups received pre-operation ODI and EuroQol assessment and were reevaluated at 6 months after surgery. At entry surgical patients showed a wide range of ODI values but most were in the moderately disabled range of 40-60 indicating to us a justification to consider surgical treatment.
Additional data from the EuroQol confirmed the surgical patients’ disability and gave expanded detail about which aspects of the patients lives were most affected. The majority of patients experienced significant pain, with chronic pain (pain ≥ 3 months) being felt more severely than acute pain (pain ≤ 3 months). Pain/discomfort was also reported very frequently, by 98.21% of patients. Difficulty with Usual activities 92.83%, Mobility 91.93%, Anxiety/Depression 80. Seventy-two percent (72%), and Self-care 57.85% were reported respectively: see Table 3. We found the sexual dysfunction assessment not to be well defined in our patient population, which is very likely due to unspoken cultural restriction amongst Thais to fully discuss this aspect of their clinical symptoms.
Table2: Patient characterritics.
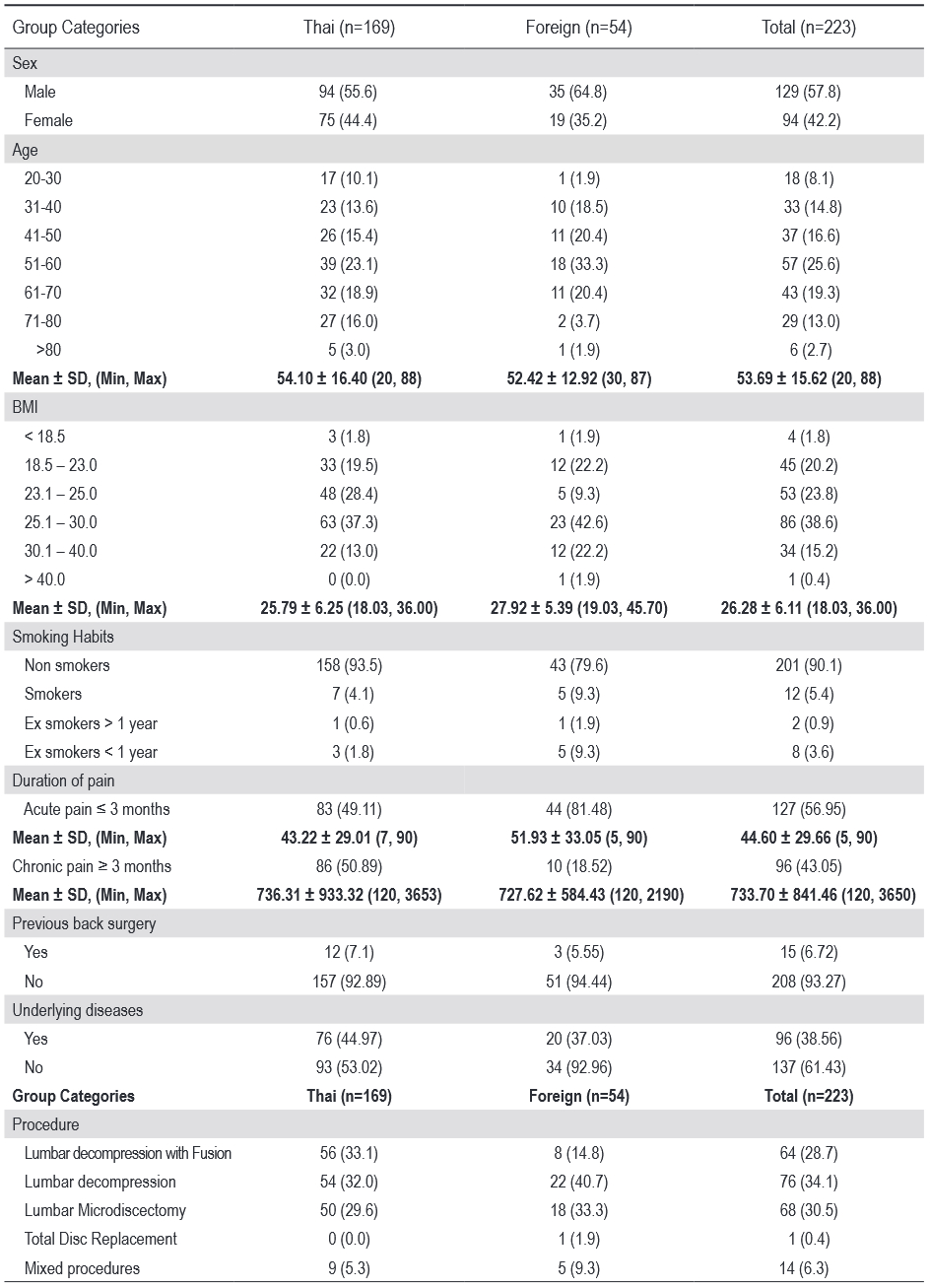
Table 3: EuroQol-5 Dimensions (EQ-5D)
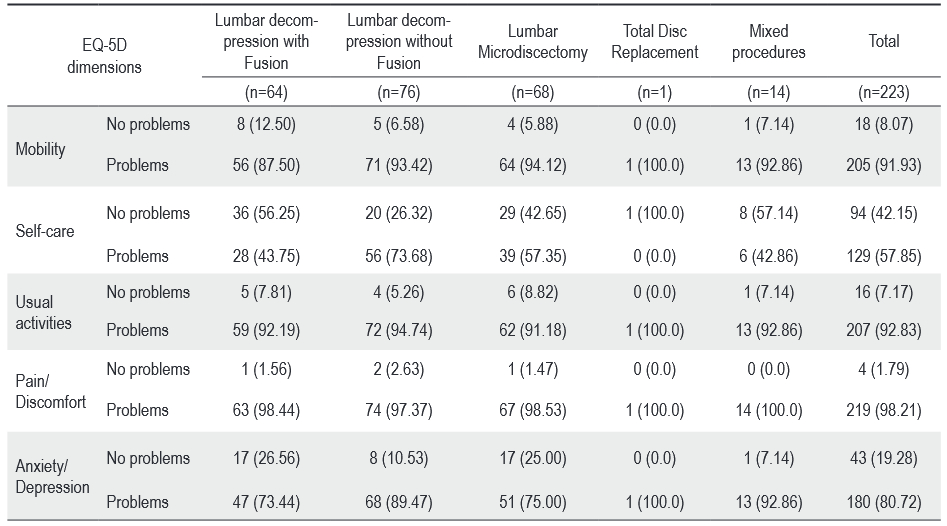
Table 4: EuroQol Visual analog scale (EQ-VAS)
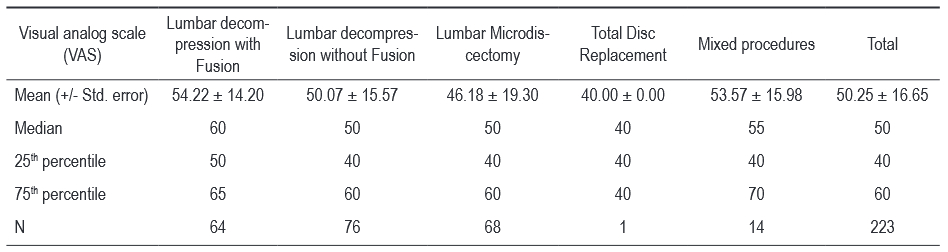
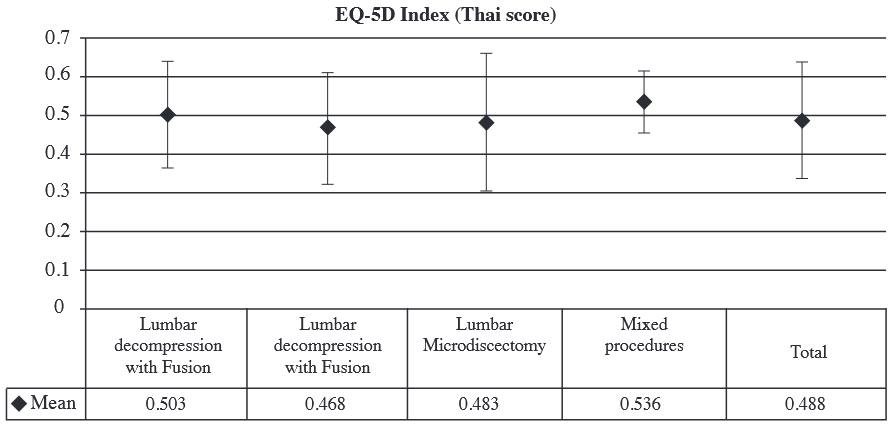
Figure 1: Average mean EQ-5D index (Thai Score) Pre-operation in each procedure
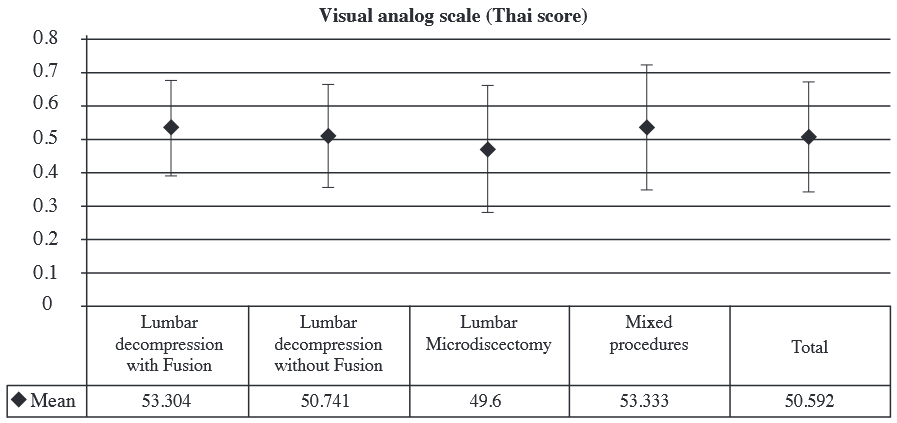
Figure 2: Average EuroQol Visual analog scale (EQ-VAS) 0-100 Pre-operation in each procedure
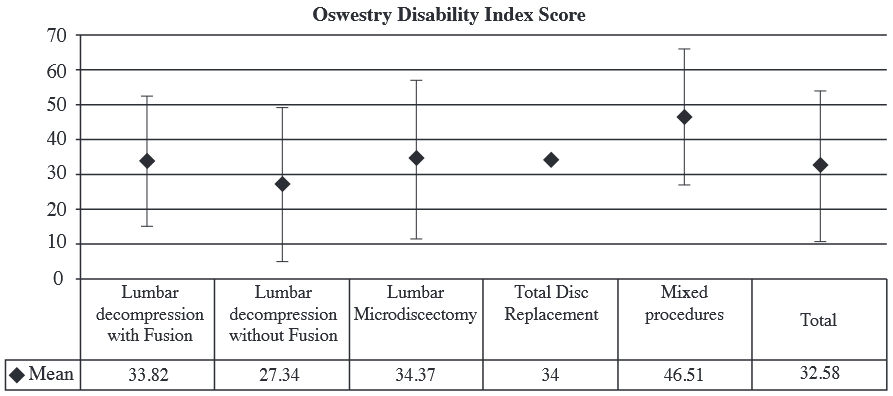
Figure 3: Average mean Oswestry Disability Index score Pre-operation in each procedure
All patients who underwent surgery for the treatment of low back pain were found to be having significant disability and restrictions in their lives; using the pre-operative ODI and EuroQol measurements, they could be categorized as having moderate to severe disability. The major problems reported were pain and mobility, there were also some problems with self-care and performance of usual activities.
Some differences were found between patients who underwent fusion and who only received laminectomies for decompression, or a herniated disc. Most patients who underwent fusion were elderly and had more comobility. Visual analog scale for patients with fusion was 60 and without fusion it was 50. We believe the preoperative ODI and EuroQol are both very useful in confirming the patients’ disability and impaired quality of life and these same indices will be useful in reliably documenting the improvement after surgical treatment.
Acknowledgement
Thanks to all Surgeons, Spine team, and the members of Low Back Pain group for their support and cooperation.