Charles T.Dotter was the first to describe balloon angioplasty and Melvin P. Judkins published the angioplasty technique using a Teflon dilating catheter in the magazine Circulation in 1964.1 This technique was developed by Andreas Gruentzig to use in the clinic, especially in the coronary artery, and was published in South Germany in 1974. This marked an important change in the use of balloons in angioplasty and in organs which is still practiced today.
The innermost layer of the artery is called the Intima. It contains endothelial cells which have only one layer on the basement mem- brane and are inserted by a connective tissue around the subendo- thelial area that connects to the media layer. This seam is called the internal elastic lamina, or IEL. The media layer mostly contains smooth muscle cells along with some collagen fibers and elastic fibers. The adjoining media layer, before the outermost layer is called Adventitia, and is the joint called the external elastic lamina, or EEL. In the adventitia layer some connective tissues, especially elastic fibers, distribute loosely. In this layer, there are both vasa vasorum, nerve plexus and lymphatic vessels. Vasa vasorum provide nourishment to the media layer.
There are three types of arteries; arteriole, muscular arteries and elastic arteries. The aorta and the iliac are the largest elastic arteries in the body. These contain the most elastic fibers while muscular arteries such as the coronary artery, the arms, legs and abdominal arteries contain more smooth muscles than elastic fibers so they control the circulation and blood pressure. Arterioles, which are the smallest arteries, act as a controller of physiology and secrete substances to regulate the operation of coronary endothelial cells like endothelin-derived relaxing factor, prostacyclin, tissue plas- minogen activator, heparin sulphate, and prostanoids.
General lesions in arteries presenting with artheroscle- rotic symptoms will have fibro-fatty plaques in the intima layer. The media layer will also be thinner and will enter a decline leading to fibrosis.
There are 2 types of plaques; fibrous plaques and artheromatous plaques. Fibrous plaques are found in abundance in the intima layer. They are later replaced by smooth muscle cells and connective muscle cells. The bold area that extends into the blood vessels is called the fibrous cap of artheromatous plaques and mostly contain cholesterol. Both types of plaques can cause stenosis or obstruction in the blood vessels. If there is a lot of fat and high cholesterol, and plaques in the fibrous cap, it can split, break and become ulcerated which can then cause thrombus. When this occurs in small blood vessels, it causes an obstruction. If this happens to the larger blood vessels, the lesions might have fibrosis or might be calcified and that can lead to chronic artery stenosis(See Figure 1).
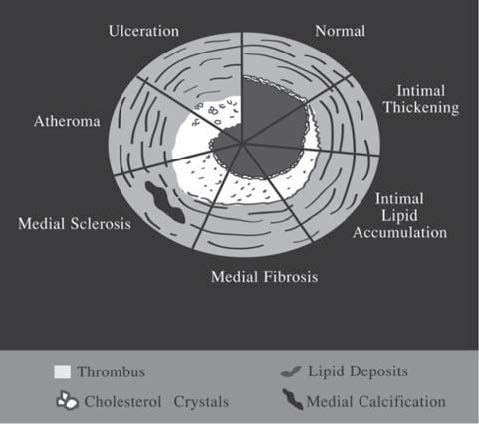
Figure 1: Diagram shows pathophysiology of artery plaques.
Many theories try to explain the mechanism and pathology of balloon angioplasty by studying laboratory animals, and cadaveric and intravascular ultrasound (IVUS) studies.
In the early days, there was a belief that plaques com- pression or plaques displacement caused the remodeling of the endothelial. This theory was refuted when the path- ological examination found that there was no change in the interior features of plaques.However,the result of the study using IVUS in measuring the size and the volume of plaques after balloon angioplasty found that plaques were squeezed out of the lesions to the top and the bottom of the lesions.This proved the existence of plaques compres- sion and displacement but this is nonetheless not the main mechanism.
The most widely accepted theories nowadays are that plaques fracture and there is localized wall dissection. After balloon angioplasty, the plaques will split and break especially the thinnest area (in the case of eccentric plaques). Moreover, the tearing of the artery is also found in the intima layer and in some parts of the media layer around the IEL line, both circumferential and longitudinal. The tearing of the artery especially in the media layer causes a dissection flap which can be seen sometimes from the vascular imaging after balloon angioplasty. These are shown by the thin stripes in the longitudinal vessels or the stain of contrast media around the area that has the intimal flap (Figure 2,3,4).
Another mechanism that explains the result of balloon angioplasty is the arterial wall stretching of the media and adventitia layers. From observation, it is found that there is a stretching of the smooth muscle cells and a necrosis of some smooth muscle cells. Studying the IVUS, it can be seen that arterial stretching happens to 25% of patients after having balloon angioplasty.3
Balloon
Rule of Laplace T = P × R
T= Tension or pressure to the artery wall
P= Pressure inside the balloon
R= Radius of the balloon used
An increase in tension or pressure to the artery can be achieved by adding inflation pressure into the balloon or by increasing the diameter of the balloon.
The types of balloon are non-complaint, compliant and special.
A non-compliant type of balloon is used in balloon angioplasty. It means that, when the balloon is enlarged to its limit, it cannot be expanded no matter how much more pressure is added inside. Therefore, it is more suitable to be used in angioplasty than a compliant balloon. The size of a compliant balloon changes according to the pressure applied inside it. The pressure is higher in the area that has no obstruction while the stenosis area has lower pressure. This kind of balloon is mostly used with a balloon expandable stent or the balloon that is used in endovascu- lar aortic repair (EVAR).
New types of balloon are made from different kinds of materials, such as polyvinyl chloride (PVC), polyethylene (PE), polyethylene terephthalate (PET), polylephin copolymers (POC), nylon derivatives (N), nylon-rein- forced polyurethane (PU) (which is the most popular material used), and co-extruded copolymers (CP).
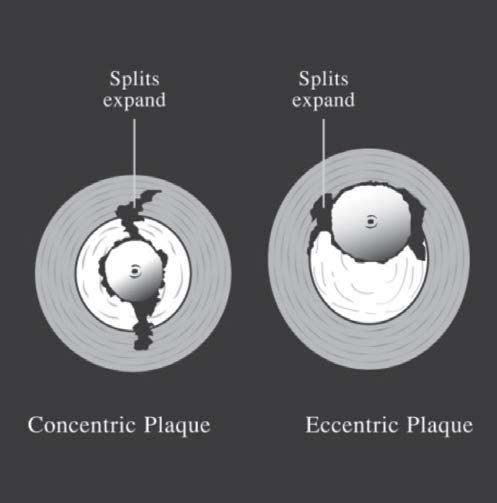
Figure 2: The demonstrated mechanism of balloon angioplasty on plaque.
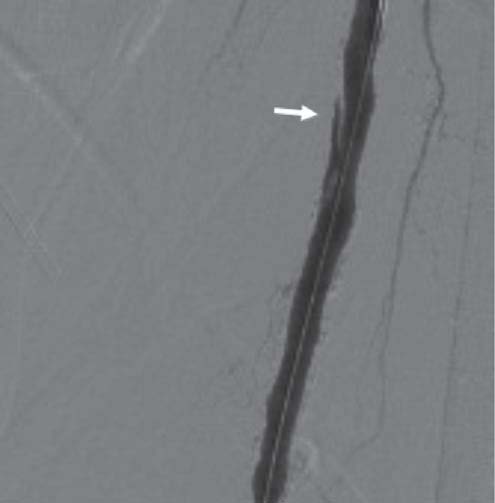
Figure 3: The right femoral artery shows an intimal fl ap after balloon angioplasty.
Non-compliant balloons are PET, PU and CP while PVC and POC are found in highly compliant balloons. The balloons that withstand High Burst Pressure (HBP) are PET, N, PU and CP. PU, CP and N can resist a puncture from sharp calcium or from the wire of a stent. Hydro- philic polymers or silicone are popularly used because of their coating effect, as this makes the balloon slippery and easier to put through the stenosis area.
The design of the balloon used nowadays is mostly true multiple-lumen (see Figure 5) which is the type of balloon that is used with guide wires sized 0.035 inch, 0.018 inch, and 0.014 inch. The same hole is used to inflate or deflate the balloon. Another type of balloon that is popularly used in expanding coronary arteries and small blood vessels is called the monorail balloon (see Figure 6). This type of balloon is special as its hole is located in the catheter that allows the guide wire to emerge from the side. With this balloon, a normal size guide wire can be used, and there is no need to change to the longer sized guide wire (such as in the case of the co-axial balloon). The disadvantage of using this kind of balloon is that it is impossible to in- ject the contrast media through the tip of the catheter and it might be more difficult to put the balloon through the stenosis areas.
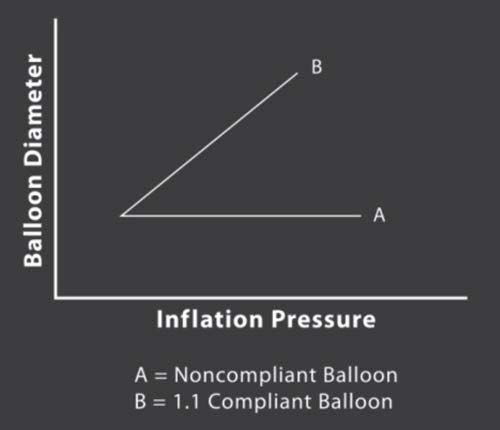
Figure 4: Diagram shows the rule the rule of Laplace.
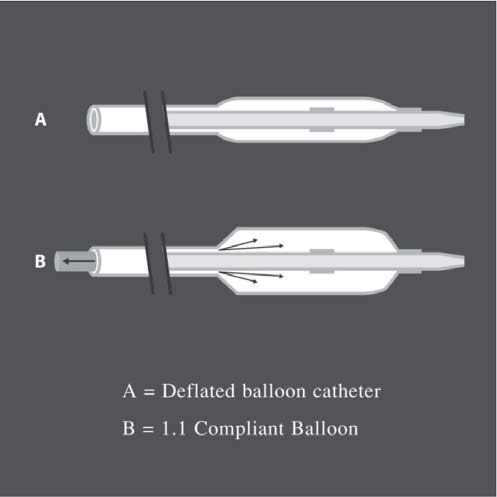
Figure 5: Diagram of true multiple-lumen balloons.
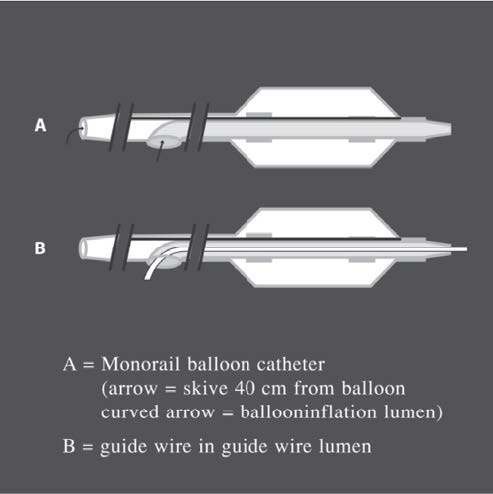
Figure 6: Diagram of monorail balloons.
To select the appropriate balloon, the following factors need to be considered: