Total knee arthroplasty (TKA) and total hip arthroplasty (THA) are among the most successful orthopedic pro- cedures with a 15 year-survival rate of more than 90% in most studies.1,2 They have traditionally been considered as inpatient surgical procedures. Historically, the inpatient stay exceeded several weeks. With multiple improvements including surgical techniques, anesthesia and implementation of clinical pathways, the length of stay (LOS) in the hospital has substantially decreased to a few days.3,4 The reasons that keep patients in hospital care postoperatively include patient and physician concerns about uncontrolled pain, delayed mobilization and possibility of peri- operative complications.5,6 However, more recent studies7 indicate that there are no differences between longer hospital stays, short hospital stays and outpatient surgery. Berger et al have reported successful outpatient total knee arthroplasty without an increase in perioperative and early postoperative complications.8 The studies which reported the outpatient arthroplasty results defined an out- patient as a patient discharged within 23 hours.8,9
Historically, it was thought that an extended acute hospital stay for several weeks was the best way for patients to recover and achieve a good outcome after total joint arthroplasty. However, there are studies that show with early discharge protocols,10,11 patients can recover safely and faster than previously thought, and this decreases inpatient workload and subsequent cost. Moreover, patients discharged quickly have comparable outcomes to patients who remain admitted for the standard hospital stay of 5-10 days. Bertin12 has reported that outpatient THA costs average 4,000 USD less than inpatient surgery. Lovald et al.7 have compared the incre- mental payment for osteoarthritis and attributable costs at 2 years and reported that costs were approximately 8,527 USD lower for the outpatient group.
To initiate and accomplish outpatient arthroplasty surgery, the roadblocks need to be understood. Studies13-15 show that patient fear or anxiety about the unknown, not knowing what is going to happen, and fear of pain are major obstacles as well as patient co-morbidities. For the surgeon, the side effects of the treatment from narcotics or anesthesia, blood loss or surgical trauma are concern- ing and indications for keeping the patient in hospital care under observation.10,16 For all of these reasons, good clinical pathways and protocols are crucial.
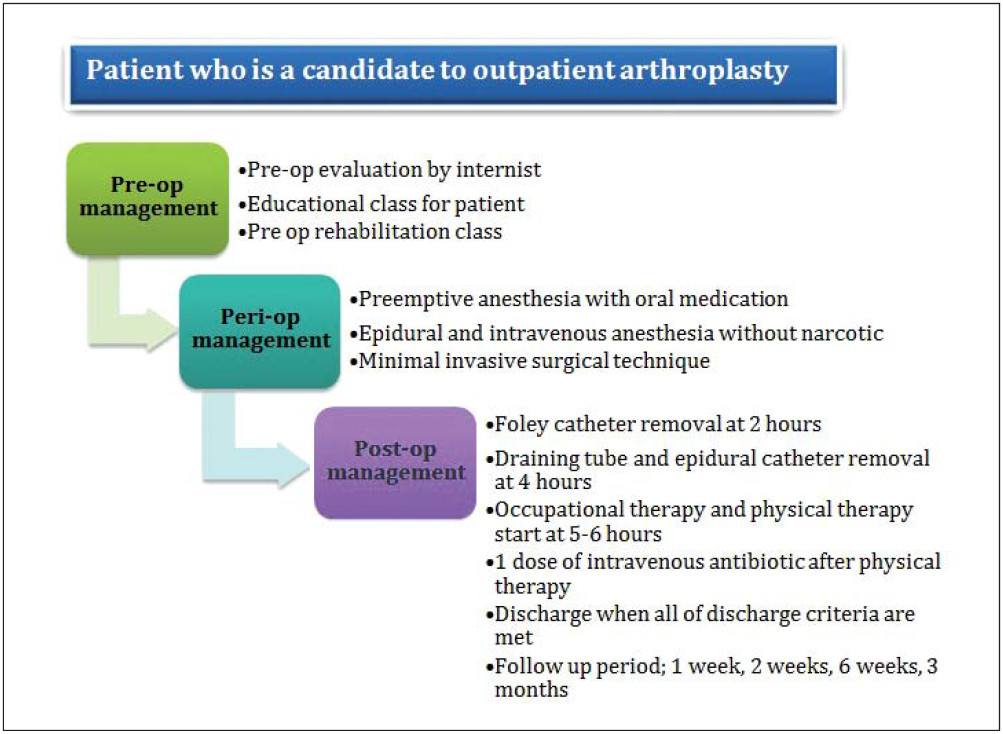
Patient selection is the first and most important step to success in outpatient arthroplasty. In addition to the history and physical examination by the surgeon, the patient’s home status should be also assessed to determine whether the patient has any support to help them move around the house safely after surgery.17 Patients with a history of diabetes, myocardial infarction, stroke, con- gestive heart failure, venous thromboembolism, cardiac arrhythmia, respiratory failure, chronic pain requiring regular opioid medications or patients who are on anti- coagulation therapy should not be considered candidates for outpatient total joint surgery as they were excluded from some of the studies.8,9 Lovald et al.18 has reported increased risk of revision, infection, accidental falls, wound complications, and death in patients with poorer health status (i.e. with a higher Charlson score). However, patients with ischemic heart disease or diabetes were not associated with increased risk for re-hospitalization, death, revision, infection, or DVT. Courtney et al.19 have reviewed 1,012 consecutive patients undergoing elective primary hip and knee arthroplasties and reported the independent multivariate risk factors for developing late (> 24 hours) complications included COPD (adjusted OR 4.16), CHF (adjusted OR 9.71), CAD (adjusted OR 2.80), and cirrhosis (adjusted OR 8.43).
Co-morbidities and any surgical risks of the patient should be evaluated carefully and cleared by a team of internal medicine specialists who are familiar with out-patient procedures and aware of factors that would make an outpatient procedure undesirable.5,20
There are studies21-25 that confirm that a significant aspect to consider is patient education which involves giving the patient appropriate goals and expectations, education about the surgical procedure and potential complications, the entire expected hospital course and postoperative care especially for pain control and am- bulation. Reviewing the patient’s questions and particu- larly addressing the patient’s needs are necessary steps to improve postoperative patient satisfaction and outcome.
Pre-arthroplasty rehabilitation further educates patients about what is expected from them after the operation, such as how patients are going to move the operated extremity, how to use a cane or crutches, and what to expect in the perioperative phase. Patients who receive pre-arthroplasty rehabilitation education have been shown to have significantly better post-operative outcomes regarding strength, recovery and function26 and also tend to save on hospital-related expenditure and have a shorter length of stay in the hospital.22,27,28
The main perioperative goals are prevention and prompt treatment of pain, nausea, and hypovolemia. It is better to manage these issues before symptoms arise. Premedication and perioperative protocols are varied in details between published studies,but all try to avoid using narcotics and aim to keep the patient well hydrated.8,9,29-31
The choice of anesthesia for outpatient arthroplasty varies according to surgeon, anesthesiologist, and insti- tution.Multimodal pain management including spinal anesthesia,local nerve block, intravenous narcotics and anti-inflammatory drugs have been shown to have significantly better post-operative pain management results.32-37
Tranexamic acid administration has also been dem- onstrated to safely reduce perioperative blood loss in hip and knee arthroplasty38-41 and to reduce blood transfusion requirements which are one of the main problems that keep patients in the hospital.
The operative intervention itself should be smooth and efficient, but not hurried. Less invasive approaches and techniques have been reported to have significantly decreased pain and improve outcomes especially in the short term.42-44
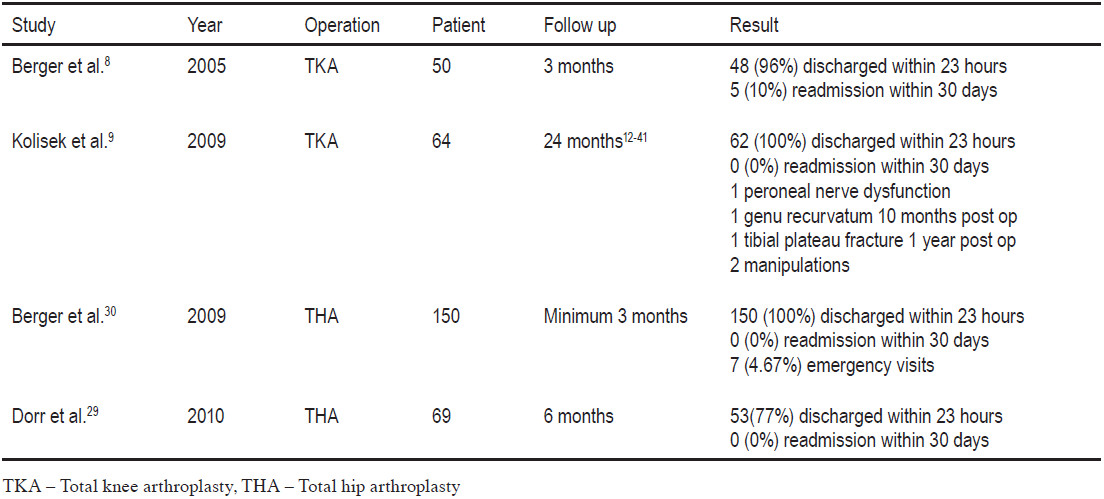
Most of the out-patient total joint arthroplasty studies have reported more than 90% success in discharging patients home within 23 hours without postoperative short term complications and less than 1% readmission due to pain, nausea or hypotension (Table 1).8,9,29,30 Lovald et al.7 have reported significantly less pain (31.7% vs 43.5%) in the outpatient group compared to the standard stay (3-4 days) group, but had higher 90 days infection (2% vs 1.9%), dislocation (0.4% vs 0.3%) and readmission rates (0.9% vs 0.5%). However, none of these differences are considered significant.
Table 1: Results of outpatient arthroplasty
A trend of outpatient arthroplasty is emerging. It has already been established for orthopedic procedures which were formerly done as inpatient procedures such as upper extremity surgery, arthroscopy and anterior cruciate ligament reconstruction. The potential benefit is that patients can recover in their own home with reduced inpatient services. Outpatient arthroplasty involves multiple and specialized protocols for preoperative, peri- operative and postoperative care. The surgeon’s role will change from the physician in the hospital to coordinator of the entire care experience.
Those interested in performing outpatient arthroplasty should initially aim to reduce the length of stay to 2 days. After a successful protocol and clinical pathway imple- mentation, once a 1 day discharge can be achieved safely, then a same day discharge may be considered.
With careful patient selection and good clinical path- ways, outpatient total joint arthroplasty can be done safely. However, current clinical studies have demonstrated only short term follow-up outcomes. Further studies with longer term follow-up and larger patient number are needed.