The diagnosis of hemobilia by non invasive magnetic resonance cholangiopancreatography (MRCP) can be difficult to interpret due to the technical procedures involved, surrounding tissue, respiratory artifacts and other factors. On many occasions, endoscopic retrograde cholangiopancreatography (ERCP) is attempted before MRCP. We presented a case of hemobilia identified using two dimension (2D) and three dimension (3D) MRCP findings to inform the physician in cases when ERCP alone cannot predict this condition.
A 45-year-old man developed chest pain for one day with no discernable underlying cause. ECG showed transient ischemia.The coronary angiogram showed severe arteriosclerosis with a narrowing of the left anterior descending (LAD) and circumflex arteries. Coronary arterial stents were performed successfully. He was administered thrombolytic drugs post-stenting. The blood examination including coagulation was within normal limits. After stenting for 48 hours, he developed fever, jaundice and colicky pain, and acute cholecystitis with ascending cholangitis. A stone in the common bile duct (CBD) was diagnosed clinically. A Computed Tomography (CT) without contrast study showed a suspected stone in the CBD. The patient underwent ERCP, but no stone could be seen in the CBD with turbid bile. A sphincterotomy was performed. Twenty four hours later he developed severe colicky abdominal pain which required morphine medication. MRCP was performed using two techniques namely:
The patient then underwent an explorative cholecystectomy and ERCP was performed intraoperatively. ERCP showed a bloody bile stain with a blood clot from the opening of the common bile duct. He had an uneventful post operative course.
The non invasive method to view the pancreatobiliary tract by MRCP is difficult because of the structures located in multiple planes and varying size. The content in the biliary tract is variable with viscosity, sludge, stones and/or blood clots. In addition, surrounding tissue contains: fluids such as stomach juice, duodenal loop, the right pelvocalyceal system,nferior vena cava,aorta,superior mesenteric vessels,respiratory movement and occasionally metallic clips from previous surgery. These produce artifacts for MRCP study. Morrin MM et al.1, however, have applied two techniques of MRCP to overcome these factors as follows:
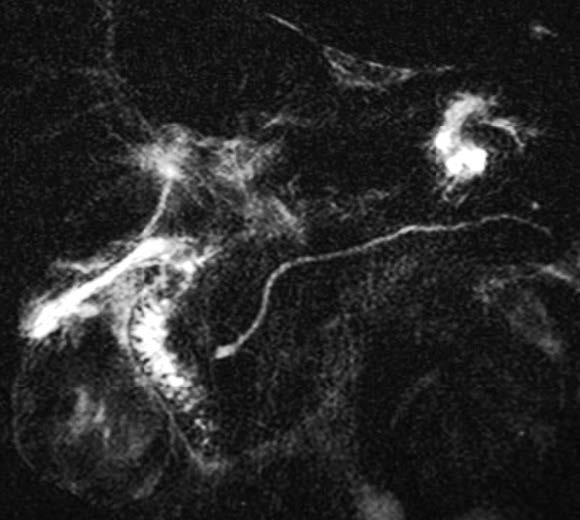
Figure 1: RARE technique shows non conspicuity of gall bladder, intrahepatic ducts and common bile duct (CBD). It depicts the pancreatic duct.
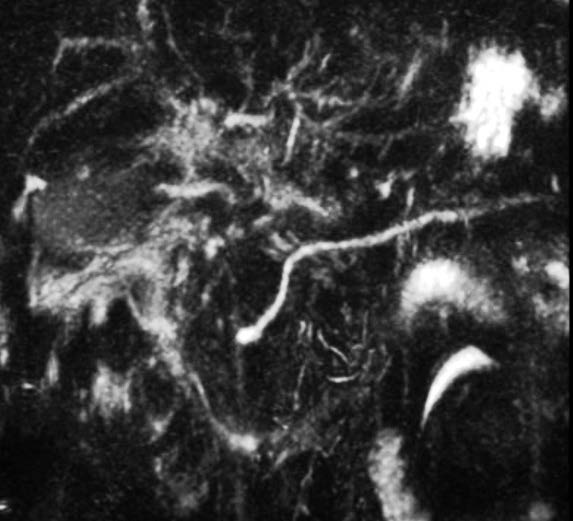
Figure 2: HASTE technique shows the same result as the RARE technique.

Figure 3: Normal MRCP using RARE technique. It shows a good image of pancreatic biliary ducts conspicuity (arrows).A few artifacts in the surrounding tissue are observed.
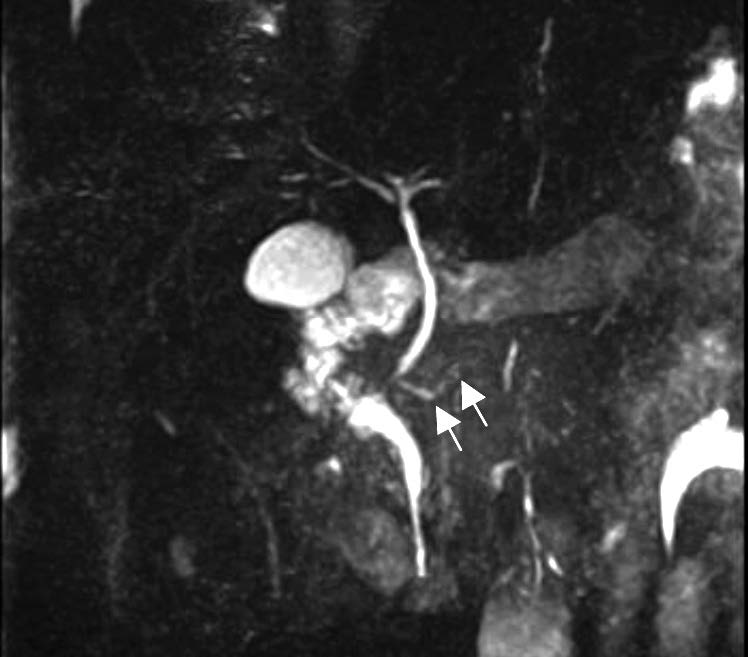
Figure 4: Normal MRCP using HASTE technique. There is less conspicuity of the pancreatic duct. More artifacts are seen in surrounding tissue (arrows).
1.Single-Short Rapid Acquisition with Relaxation Enhancement (RARE)
This technique is applicable for the duration of a single breath hold, a very long echo time (> 500 ms.) and multi-slices are performed at various angles (360°). This provides better pancreatic and intrahepatic ducts conspicuity (Figure 3).
2.Multiple-slice Half-Fourier Acquisition Single-short Turbo-spin Echo (HASTE)
This technique is a 3D reconstruction, with normal breathing. Irie H et al.2 claimed that it was better to detect a small choledocholithiasis. In our personal opinion, there are some cases when the visualization of the pancreatic duct is not sufficient (Figure 4).
For our case the clinical diagnosis of cholecystitis with ascending cholangitis and probably a stone in the common bile duct was suspected. Hence, a CT of the upper abdomen was performed. It showed a distended gallbladder containing small stones and a suspected small stone probably dislodged from the gallbladder into the common bile duct. We then decided to perform MRCP using the two techniques of RARE and HASTE studies. The findings showed non conspicuity of the gallbladder, intrahepatic duct and common bile duct but the pancreatic duct was depicted more clearly with the RARE technique. This effect can explain the basis of blood in the biliary tract which contains a hemoglobin-caused paramagnetic effect, amount of bile excretion, viscosity and components of bile fluid. MRCP will show hypointensity in gallbladder and CBD. In contrast, the pancreatic duct will show high intensity because of no bloody fluid. MRCP is a static study. The image may be inferior to ERCP which is a dynamic study. But MRCP is still required in cases requiring an examination by ERCP for many clinical indications. That said, MRCP is a non-invasive method and it is superior to ERCP in the case of hemobilia as shown in this case. The radiologist and radiographer should understand all potential pitfalls of MRCP and the use of various study techniques. This may help avoid an ERCP which may often be unnecessary.3
The diagnosis of hemobilia by MRCP using either RARE or HASTE techniques is very helpful. The paramagnetic property of hemoglobin, content and viscosity bile could explain the non depiction of the biliary tract. In some cases, however, HASTE may lead to a false negative result.
We recommend applying both techniques of MRCP in the case of a suspected hemobilia instead of ERCP as this cannot diagnose this entity.