Non-Communicable Diseases (NCDs) are a significant health problem worldwide.1 NCDs are defined as chronic conditions caused by multiple risk factors, resulting in prolonging the course of illness and functional disability.2 Of the 56 million global deaths in 2008, over 60% (36 million) died from NCDs, and the death rate increased to 68% (38 million) in 2012 and 71% (40.5 million) in 2016.
Furthermore, NCDs have an impact on physical and socioeconomic status. NCDs are the most significant cause of mortality and disability, as indicated by disability-adjusted life years (DALYs), which is the sum of the years of life lost (YLLs) due to premature mortality and the years of productive life lost due to disability (YLDs).3 With regards to the economic consequences, the cost of NCDs is significant and is increasing. For the period between 2008-2030, it is expected that NCDs will cost 21 trillion USD due to illness and lost productivity.4 In Thailand, the healthcare cost of NCDs accounts for 2.2% of government expenditure (2 hundred thousand million baht per year).5 In response to the increasing burden from NCDs, prevention and management of NCDs are important health care services especially in primary care settings, impacting all stakeholders.
Given these problems, the government and stakeholders have launched policies and projects to deal with NCDs, particularly in primary care settings including district health system (DHS), primary care cluster (PCC), and Thai Health Promoting Hospital (THPH). In addition, HA institutions have started to accredit the primary care system in order to enhance the quality of care. HPs play an essential role in mobilizing processes in the primary care system and in responding to patients’ needs. HP’s roles prioritise health promotion and disease prevention including: monitoring, diagnosis, and investigating health hazards in communities, health education and health counselling, diseases surveillance, establishing and contributing to strategic planning, empowerment for community participation, development of database in primary care, research, innovation, and supporting health care services. In addition, HPs, especially nurses, have duties including: history taking, physical examination, laboratory interpretation, differential diagnosis and medication prescription following the protocol, prevention and management of acute illnesses and stable chronic illnesses, emergency care, and referral systems.6,7 Unfortunately, studies on the needs of nursing as described by patients with NCDs, HP, and HA are limited. Thus, this study aims to explore the nursing needs of NCDs in order to respond to patient’s needs and to increase the quality of care in primary care settings.
This study used a descriptive quantitative design, approved by the Institution Review Board for the Protection of Human Subjects from the Faculty of Medicine Ramathibodi Hospital, Mahidol University, No. MURA2018/973, dated December 11, 2018. Participants included 385 patients with NCDs, 21 HP, and 10 HA surveyors. The sample size of patients was determined based on the Kelsey formula.8 Through purposive sampling, patients with NCDs met the following criteria:
Inclusion criteria for HP were:
1. Working in HA for more than one year.
2. Having experience as a hospital accreditation surveyor.
Instruments
The instruments were divided into three parts, including instruments for patients with NCDs, health care providers, and HA surveyors.
1. Instruments used to collect data from patients with NCDs included:
1.1 The demographic survey questionnaire consisting of gender, age, education, occupation, income, family history, and comorbidity.
1.2 The secondary data from the medical records included patient health status consisting of blood pressure (BP), fasting blood glucose (FBG), body mass index (BMI), and waist circumference (WC). 1.3 The Needs of Nursing Questionnaire as perceived by patients with NCDs was modified from the Nurses’ Role in Primary Care Questionnaire developed by Thailand Nursing and Midwifery Council. The questionnaire consisted of 6 subscales (31 items) including NCD care (8 items), PMC (6 items), community activity (5 items), emergency care (4 items), home visit (4 items), and communication (4 items). The response was a 5-point Likert scale, ranging from less required (1) to strongly required (5). The interpretation was based on the sum score divided by numbers of items. The higher score indicated a higher need. The content validity index (CVI) was 0.97 and Cronbach’s alpha coefficient (α) was 0.77.
2. Instruments used to collect data from all HP included:
2.1 The demographic survey questionnaire consisting of gender, age, educational level, work position, and years of work experience.
2.2 The Needs of nursing Questionnaire, as perceived by HP, was modified from the Nurses’ Role in Primary Care Questionnaire, developed by Thailand Nursing and Midwifery Council. The questionnaire consisted of 7 subscales (33 items) including NCD care (9 items), PMC (5 items), community activity (4 items), emergency care (3 items), home visit (5 items), communication (4 items), and data management (3 items). The response was a 5-point Likert scale, ranging from less required (1) to strongly required (5). The interpretation was based on the sum score divided by a number of items. A higher score indicated a higher need. The CVI was 0.95, α = 0.97.
3. Instruments used to collect data from the HA surveyors included:
3.1 The demographic survey questionnaire consisting of gender, age, work position, and years of work experience.
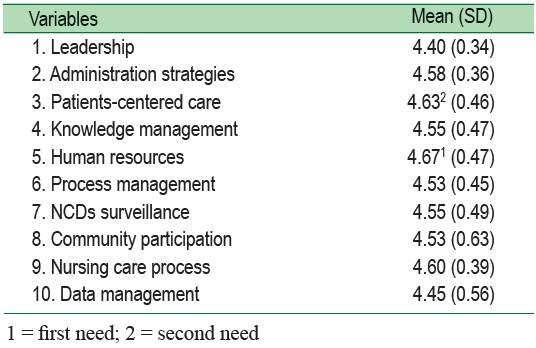
3.2 The Needs of nursing Questionnaire, as perceived by HA was developed and based on the guidelines set by DHS standard. The questionnaire consisted of 10 subscales (37 items) including leadership (3 items), administration of strategic plan (6 items), patient- centered care (3 items), community participation (3 items), knowledge management (4 items), human resources (3 items), process management (4 items), NCDs surveillance (2 items), nursing care process (5 items), and data management (4 items). The response was a 5-point Likert scale, ranging from less required (1), to strongly required (5). The interpretation was based on the sum score divided by a number of items. A higher score indicated a higher need. The CVI was 0.97, α =0.93.
Data collection
The researchers made an appointment with patients with NCDs for collecting data on demographic information, and needs of nursing for NCDs, lasting approximately 10-20 minutes/person using a structured interview. Then, the researchers obtained the patient’s health status from secondary data, whereas the HP completed the self-report questionnaires. The questionnaire was mailed to 26 hospital surveyors along with an envelope and stamp to return mail to the researcher.
Statistical Analysis
Descriptive statistics, including frequency, percentage, range, median, mean and standard deviation, were used.
A total of 385 patients with NCDs from five primary care settings participated in this study. Eight patients with NCDs were excluded due to a short portable mental status score of less than 7. Most of the patients were female (72.2%) with a mean age of 63.9 ± 10.7 years, ranging from 21 to 88 years old, had elementary education (77.7%), and used universal health coverage insurance scheme (91.2%). More than 70% of patients with NCDs had at least two diseases including HT, DM, cardiovascular disease (CVD), and stroke. 2 The mean BMI in patients was 25.74 ± 4.67 kg/m . More than 70% were overweight or obese. The mean waist circumference in males was 93.56 ± 11.93 cm. The mean waist circumference in females was 89.54 ± 11.26 cm. The mean systolic blood pressure was 131.37 ± 14.16 mmHg. The mean diastolic blood pressure was 74.30 ± 10.83 mmHg. The mean fasting blood glucose was 114.73 ± 34.28 mg/dl (Table 1).
The majority of all HP were female (81%) with a mean age of 39.3 ± 12.5 years. Most of them obtained a bachelor’s degree (76.2%). The highest proportion of all HP was public health technical officers (33.3%), following by registered nurses (28.6%), public health officers (14.3%), dental therapists (14.3%), and Thai traditional medicine practitioners (9.5%). The median year of work experience was 21 years, ranging from 1-39 years.
Half of HA surveyors were male (50%), similarly to female. Their mean age was 49.9 ± 12.2 years. Most of them obtained a master’s degree (70%). The median year of work experience as an HA surveyor was 2.5 years, ranging from 1-17 years.
The highest need of nursing as described by patients with NCDs was in emergency care (ER care) (4.27 ± 0.67), including contact with healthcare providers (4.42 ± 0.74), knowledge on emergency complications (4.29 ± 0.85), and basic emergency response skill (4.19 ± 0.88), followed by primary medical care (PMC) (4.12 ± 0.66) including diagnosis (4.25 ± 0.86), receiving medication (4.21 ± 0.82), and physical examination (4.15 ± 0.86), community activity (4.01 ± 0.78) including knowledge and skill for complication prevention (4.11 ± 0.90),quit smoking campaign (4.05 ± 1.08), quit alcohol consumption campaign (3.99 ± 1.14), and promoting a healthy diet (3.99 ± 0.99), communication (3.88 ± 0.72) including using simple language (4.30 ± 0.76), communication through public broadcasting (4.25 ± 0.82), and health education through appropriate media (3.92 ± 1.00), home visit (3.74 ± 0.90) including community and healthcare providers support (3.91 ± 0.99), environmental modification (3.72 ± 1.08), and environmental assessment (3.68 ±1.11), and NCD care (3.65 ± 0.64) including medication refill (4.14 ± 0.92), follow up (4.12±0.88), and referral system (4.07 ± 0.97). The highest score in each subscale is presented in Table 2.
The highest need of nursing as described by all healthcare providers was in ER care (4.24 ± 0.83) including referral system in emergency care (4.20 ± 0.94), basic emergency response skill (4.13 ± 0.83), and knowledge and skill of emergency management (3.80 ± 1.08), followed by PMC (4.19±0.76) including advice on self-management (4.13 ±0.83), differential diagnosis, history taking, physical examination and laboratory interpretation (4.00 ± 1.13), advice on diseases and medication (4.00±1.00), and follow up (4.00±0.75), home visit (4.15±0.85) including health assessment and demonstration of health management (4.13 ± 0.83), empowering the patient’s family (4.00 ± 1.06), and procedures at home (4.00 ± 1.00), data management (4.07 ± 0.98) including managing data including HT, DM, IHD, and stroke (4.07 ± 1.03), managing data on health status (3.93 ± 1.22), managing data on health behaviors (3.73 ± 1.10), communication (4.07 ± 0.89) including selection of exciting media for health education (4.00 ±1.06), using simple language (3.93 ±1.16), and communication through social media (3.93 ± 1.16), community activity (4.05 ± 0.79) including health promotion in the community (4.00 ± 0.84), environmental modification (4.00±1.00), and activity for management of NCDs (3.87 ± 0.99), and NCD care (3.98±0.82) including medication refill (4.13 ± 0.91), counseling on quit smoking and alcohol consumption (4.07 ± 0.96), screening (4.00 ± 0.76), and promoting healthy diet and physical activity (4.00 ± 0.93). The highest score in each subscale is presented in Table 2.
The highest need of nursing as described by HA surveyors was in human resources (4.67 ± 0.47) including knowledge and skills for NCDs in primary care (4.90 ± 0.32), knowledge and skills for NCDs in community (4.70 ± 0.67), and assessment of medical equipment (4.40±0.69), followed by patients- centered care (4.63 ± 0.46) including perception of needs through appropriate methods (4.80 ± 0.42), responding to patients’ needs (4.60 ± 0.52), and survey needs and satisfaction in patients with NCDs (4.50±0.70), nursing care process (4.60 ± 0.39), administration strategies (4.58 ± 0.36), knowledge management (4.55 ± 0.47), NCDs surveillance (4.55 ± 0.49), community participation (4.53±0.63), process management (4.53 ± 0.45), data management (4.45 ± 0.56), and leadership (4.40 ± 0.34) (Table 3).
Table 1: Characteristics of the Patients (n = 385)
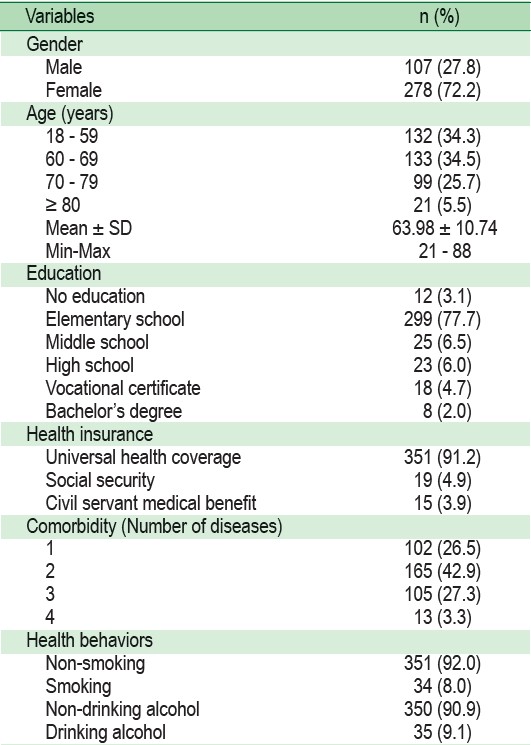
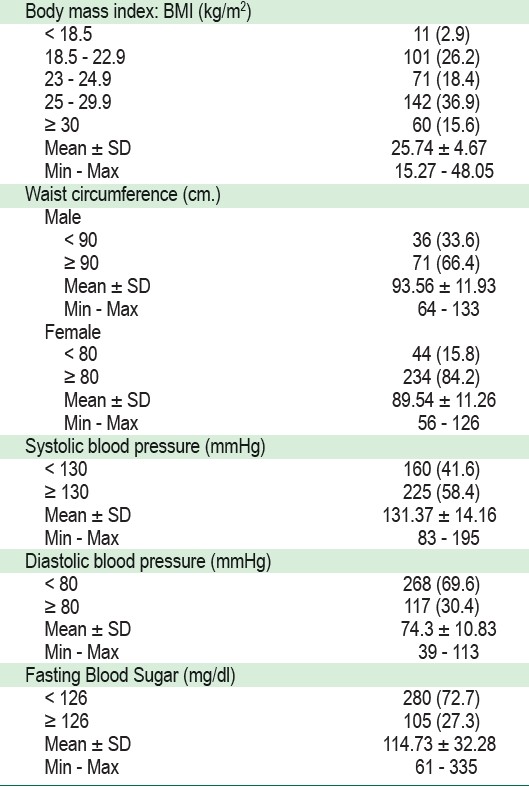
Table 2 : Needs of nursing as described by patients with NCDs and healthcare providers in each subscale
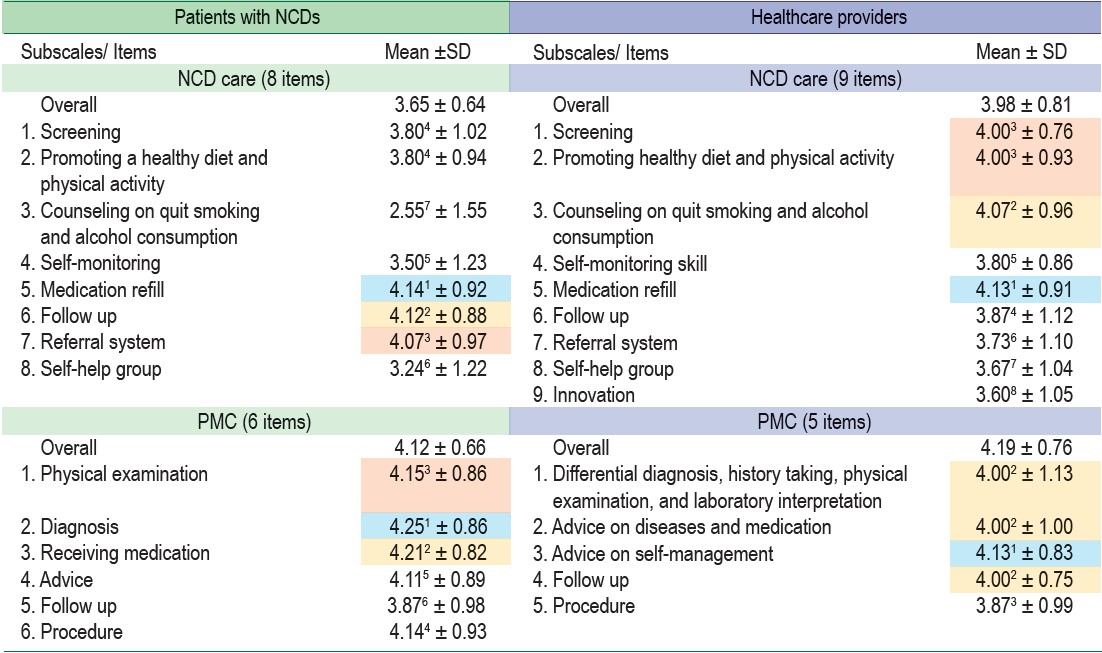
Table 3: Needs of nursing as described by hospital accreditation surveyors (n = 10)
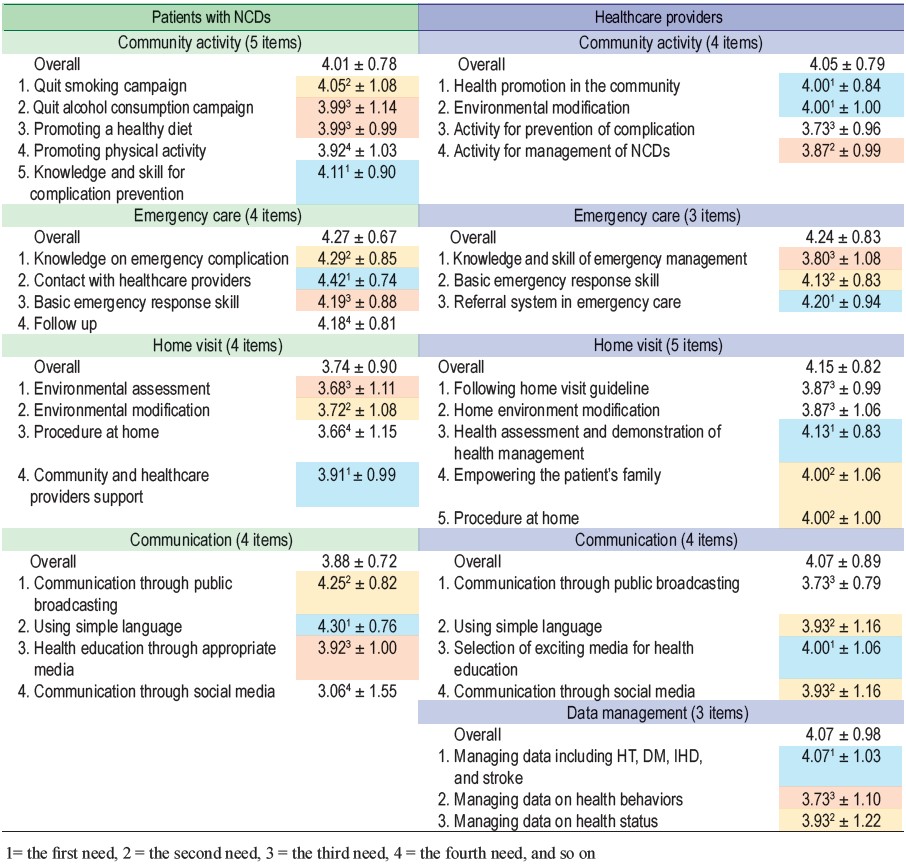
Table 3: Needs of nursing as described by hospital accreditation surveyors (n = 10)
Needs of nursing as described by patients with NCDs
Evidence to support the needs of nursing in ER care is very important because the majority of patients with NCDs in this study were older adults who tend to develop health problems from both the aging process and the consequences of having NCDs. Aging is a complex process leading to macromolecular damage and organ functional losses involving physiological changing in all body systems such as cardiovascular, nervous, respiratory, digestion, renal, endocrine, and musculoskeletal systems.8 For example, atherosclerosis leads to an increase in smooth muscle tone and the decline in a number of arterial pacemaker cells resulting in elevated blood pressure and abnormal cardiac rhythm. Moreover, renal function will decrease due to the loss of renal mass and lower glomerular filtration rate (GFR), resulting in renal disease.9 With increasing age, the function of the insulin-producing beta cells also decreased, increasing blood sugar and may result in hyperglycemia.9
Furthermore, older patients with NCDs tend to visit the emergency department more than those without NCDs.10 The pathophysiology of NCDs causes emergency conditions, particularly uncontrolled hypertension leading to increased organ damage including heart failure, kidney failure, or stroke.11 For example, the mechanism involving hypertension includes cardiac output, peripheral resistance, renin-angiotensin- aldosterone, and autonomic nervous system. Chronic organ systems dysfunctions lead to emergency conditions.12 Furthermore, the abnormal insulin-mediated glucose production and insulin-mediated glucose uptake leads to hyper-hypoglycemia in patients with type 2 diabetes.13 Thus, patients with NCDs need more emergency care than their counterparts. Patients with NCDs required knowledge to recognise warning signs of emergency conditions and the necessary skills to manage these conditions before referring to a hospital and contact with an HP team with basic emergency response skill.14,15,16
The needs of nursing for PMC were also very high, ranking second. In this study, patients expressed their need for diagnosis, receiving medication, physical examination, nursing procedure, advice for self-care and medication use, and follow up. Patients with NCDs are more likely to have common health problems that need primary medical care such as upper respiratory infections, diseases of the skin and subcutaneous tissue, and diseases of the digestive system particularly in older patients.10, 17 Moreover, the district health- promoting hospitals are located close to their home; therefore, it is convenient for them to visit there for health services using PMC.
For community activities and communication, patients needed activities that provided the most information on the complication of NCDs, followed by campaigns on quitting smoking and alcohol consumption, promotion of good nutrition and physical activity. The results indicated that patients need support for behavioral modification. This was consistent with their need for communication, particularly using simple language to provide medical and health information. On the other hand, communication with HP using a mobile phones, Line applications, and Facebook were at the lowest need. This context of rural communities showed that patients do not commonly use social media, especially among older adults, when compared with urban areas and younger adults.18 However, they needed communication through public broadcasting along with supports by HP, community members, and their families.
For the home visit, patients with NCDs who have a long- term chronic condition, uncontrolled hypertension or diabetes, and advanced age tend to experience complications from NCDs which need a home visit more than others.19,20 The evidence showed that the nurse-led home visit program has an impact on increasing self-management skills resulting in improving medication adherence and health behavioral modification.21
Unexpectedly, nursing procedures at home were at the lowest need because most of them had the ability to perform activities of daily living and live without medical equipment. This is relevant to adhere to home visit guidelines to provide home visits based on patients’ needs and health status.22
The NCD care was at the lowest need. Their need for self- monitoring skills was rather low. It could be due to vision impairment.7 Moreover, they had been living with NCDs for more than 5 years, so they had already developed self-moni- toring skills. Meanwhile, medication refill was at the highest need. It was consistent with a previous study revealing that time since diagnosis is the predictor of medication adherence, indicating a need for medication refill.23
More than half of patients with NCDs in this study were overweight or obese; they had excessive waist circumference and an average systolic blood pressure higher than the target blood pressure of 130/80 mmHg (Table 1) according to the American Heart Association.24 This is probably associated with less concern about NCDs as described by needing less self-help groups and self-monitoring skills in this study sample, consist- ing mainly of older adults. However, they had normal blood sugar on average, indicating that they regularly take medication lowering blood sugar and their need for medication refills, consistent with medication adherence.25
Needs of nursing as described by HP
HP needing to provide ER care scored at the highest rank. The primary care settings are located close to their patients’ homes. Thus, when the patients experience emergency health problems, they usually decide to go to primary care settings. The result was consistent with a previous study on the role of nurses in primary care settings revealing that the majority of health problems consist of ER care.26 Also, there are guidelines for ER service delivery involving all of HP. The guidelines aimed to provide ER care linked to the community, primary care, and definitive care in the hospital. These guidelines identified the activities and capacities of each level of health care settings. The essential care in primary care settings includes triage, basic resuscitation, fast track and special services especially geriatric emergency. The geriatric emergency includes geriatric triage, an initial screening toolto recognize and evaluate older people at risk, fall and delirium assessment, medication reconciliation, and procedures including wound care and urinary catheter insertion.27
The needs of nursing for PMC ranked second as PMC is an essential service. One-third of HP obtained nurse practitioner certification. Therefore, they needed to provide advice for medication use and self-management according to differential diagnosis through history taking and physical examination, while the needs of nursing in NCDs ranked lowest on innovation. The HP spent most of their time on routine jobs with no financial support for innovation.28 HP’needs of nursing were different in different primary settings depending on patients’ and HP’s characteristics and sociocultural and geographical contexts including urban and rural types of communities29 depending on where each primary care setting was located, which may need further detailed exploration.
Needs of nursing as described by HA surveyors
The needs of nursing as described by HA surveyors was in human resources including knowledge and skills in NCD care in primary care and community and assessment of medical equipment, ranked highest. This indicates a significant component of care quality particularly knowledge and skills in NCD care, a relevant indicator of care quality assessment. HA roles include assessing work systems, accrediting healthcare organization, supporting and developing quality of healthcare organizations. The process of accreditation includes self- assessment, data review, and external confirmation by experts.30 In addition, a perspective of HA surveyors revealed a need for patient-centered care particularly perceived patients’ needs and responses to patients’ needs, followed by administration of the strategic plan and knowledge management which was defined as a structure of care quality assessment. This may be explained as all these structures were principal inputs leading to a process, particularly patient care process, through care provision based on: professional standards, collaboration, system management to access to NCD care, and follow up with continuing care as well as outcomes including evaluation of health service delivery, data management of care for specific NCDs (stroke, ischemic heart disease, hypertension, diabetes) and health behaviors (food consumption behaviors, physical activity, smoking, alcohol consumption), and health outcomes (blood pressure, blood glucose, body mass index, and waist circumference).
The highest need of nursing for prevention and management of NCDs as described by patients with NCDs and HP was in emergency care whereas the highest need as described by HA surveyors was in human resources. Thus, HP especially nurses, should enhance their knowledge and skill in emergency care for patients with NCDs including signs and basic emergency care, emergency contact with nurse and referral systems in a primary care setting as well as PMC care including diagnosis, receiving medication, and physical examination. In addition, the HP should be concerned with the appropriated community activity, communication with patients, and home visit in each setting.
The Thai Nursing and Midwifery Council supported this study.