Gianotti-Crosti syndrome (GCS) or papular acrodermatitis of childhood (PAC) is a childhood skin condition characterized by lymphadenopathy, anicteric hepatitis and an erythematous papular eruption symmetrically distributed on the face, buttocks and extremities. The cause of acrodermatitis usually occurs in association with a viral illness. Hepatitis B Virus (HBV) and Epstein-Barr Virus (EBV) are the most common causes.
A one year and three months old French boy, who had previously been healthy, travelled six days prior to admission to Samui Island with his family for a vacation, where he played in the sunlight a lot. After the third day he developed a fever with a rash. He was sent to Koh Phangan hospital and was given paracetamol and cetirizin. On day 4, he developed a high grade fever and could not eat well and did not play, and was consequently transferred to Bangkok Hospital Samui. Vitals sign were: BP 123/72 mmHg, pulse 140/min, respiratory rate 24/min, temperature 37.8-38.7 oC. He presented a mild injected pharynx, with no oral mucosa changes or cervical lymphadenopathy detected. The skin lesion was an erythematous maculopapular rash on the buttock, upper and lower extremities. He was admitted to Bangkok Hospital Samui for two days for investigation and symptomatic treatment. Steroids were given as follows: dexamethasone, chlorpheniramine, hydroxyzine, 0.02% triamcinolone acetonide milk lotion. No response to the medica- tions prescribed was seen and the rash worsened. The patient was then transferred to the pediatric team at Bangkok Hospital for further investigation and treatment.
Since admission, the patient remains afebrile and diarrhea started. He did not experience vomiting but has poor intake and mild cough was noticed. He developed a papulovesicular rash on his face, with more extensive rash on the upper and lower extremities. (see Figures 1A-C).
Past history: 3 weeks ago he had chicken pox, symptomatic treatment in France. No history of drug allergy. Vaccination schedule complete.
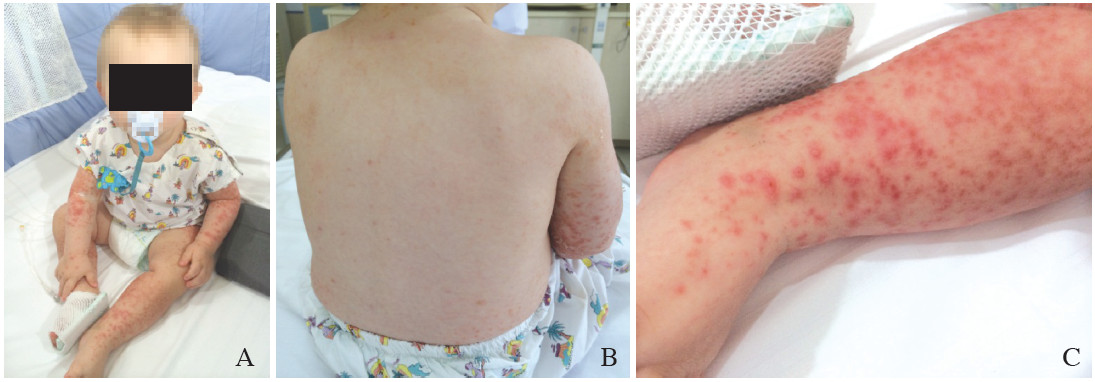
Figures 1A-C: Patient presents with papulovesicular rash on face, with more extensive rash on upper and lower extremities.
Physical examination: Vital signs showed BP 94/51 mmHg, pulse 120/min, respiratory rate 26/min, temperature 36.1 oC. Patient looked weak but body weight was 12.3 kilograms. There were positive findings for mild injected pharynx, monomorphous, nonpuritus erythematous papulovesicular rash on his face, ear, buttock, both upper and lower extremities. Otherwise unremarkable. Rash was pruritic. Some excoriation was noted on his buttock and lower extremities. Individual lesions measured 2-4 mm in diameter. There were no lesions on palms and soles. No hepatosplenomegaly or lymphadenopathy was detected.
Investigations: Complete blood count (CBC) revealed anemia and neutropenia. Hb 10.6 g/dL Hct 31.7% WBC 8,960 cell/mm3 with 25% of neutrophil, 61.5% of lymphocyte, 9.5% of monocyte and 3.8% of eosinophil, no band form, platelet 286,000 cell/mm3. Elevation of inflammatory marker CRP 7.43 mg/L. Liver function test was normal: albumin of 4.54 g/dL, SGOT 32 U/L, SGPT 13 U/L. Urinalysis exam and stool exam were normal. Patient was vomiting and had poor intake, so electro- lytes were administered: sodium 138 mmol/L, potassium 4.48 mmol/L, chloride 102 mmol/L, TCO2 20.5 mmol/L and high anion gap mmol/L. Tests were conducted for mycoplasma, measles virus, herpes simplex virus and EBV (both IgG and IgM) were negative. Anti-streptolysin O less than IU/m. Stool cultures were negative.
Hospital course: Diagnosis of Gianotti-Crosti syndrome was given to the patient after reviewing all clinical findings and investigations. Differential diagnosis included: erythema multiforme, measles, and drug allergy. He was on IV fluids and symptomatic treatment was given: medicine for cough, diarrhea (infloran berna), azithromycin syrup for bronchitis. For the rash, patient was administered hydroxyzine, cleanser, with desquamation seen at upper and lower extremities so moisturizing lotion was given.
On Day 2 of admission to Bangkok Hospital, there was no fever and diarrhea noted. His appetite and activity increased, so IV fluid was discontinued. Discussions with the pediatric doctor and pediatric dermatologist regarding discharge and air travel were under taken at Day 3.
Gianotti-Crosti Syndrome (GCS) was first described in 1955 by Gianotti in a case of HBV infection.1 GCS is mainly a clinical diagnosis. There are no laboratory characteristics for GCS. Dermatologic findings usually include: erythematous vesiculopapular eruption symmetri- cally distributed on the face, buttocks and extensive surface of the extremities with or without pruritic infection.2-4It is associated with hepatomegaly, splenomegaly and lymphadenopathy. GCS usually occurs in children younger than five years of age, and affects both boys and girls equally.5,6 However, in adulthood, females may be more prone than males to develop GCS.7
GCS usually occurs in association with a bacterial and viral infection. HBV and EBV are the most common causes. The incidence of EBV infection has been estimated to be 0.37-26.5 percent.8 A review of 308 cases indicated that 22 percent of cases were caused by HBV and 78 percent by other viruses. GCS is less commonly reported in association with other pathogens, includingviruses,9,10 cytomegalovirus,11,13 parvovirus,14,15 parainfluenzavirus,16,17 hepatitis A virus,18,19rotavirus,20,21 molluscum contagiosum,14,22 respiratory syncytial virus,10 human immunodeficiency virus,23human herpesvirus6,24,25 Mycoplasma pneumo- niae,26,27 beta-hemolytic streptococci,10 bartonella henselae28 and borrelia burgdorferi.29 Occasional cases have been noted following immunization with Bacillus Calmette- Guerin (BCG), poliovirus34, diphtheria, tetanus, pertussis, and influenza.30-33 Reported patients with GCS were often seen 7 to 14 days after acute infection.30,32,33
GCS is usually associated with HBV infection. Most of the cases present symptoms after immunization. Skin manifestations occur during 7 to 14 days after immunization or infection. The link with varicella infection onset on the second day after the appearance of skin lesions.34,37,38 Spear and Winkelmann reported a case of GCS with the occurrence of varicella three weeks before the onset of rash.39 But in a report from Emel Erkek, the patient received an oral polio vaccine two days before, so it cannot be proved that GCS is caused due to being associated with the polio vaccine or varicella infection. The lesions of GCS may be a consequence of viral antigenemia or circulating immune complexes.40 In this case, the patient developed GCS three weeks following a varicella infection, it may originate from a process of the formation of the immune complex. It has been suggested that the development of GCS may require a primary previous immune stimulation and a secondary viral infection.41,42
There are two reported cases of GCS associated with viral diarrhea. In 1988, Patrizi et al43 reported the first two cases of GCS associated with rotavirus infection. In another report in 1998, Di Lernia et al20,21 reported a third case possibly associated with rotavirus. Our case presented with monomorphus erythematous papule before clinical diarrhea. So it is unlikely that our case is associated with viral diarrhea. The treatment of GCS is supportive. Antihistamine may help decrease the itchiness but will not shorten the course of the rash.
This is a case report of GCS with clinical features on the skin, with rash occurring at cheeks, extremities, buttocks and symmetrical characteristics of monomor- phous, flat, pink-brown papules or papoluvesicles. The symptoms occurred after a varicella infection 3 weeks prior to admission. The investigation for viral infections except HBV proved negative. Hence we presume this case maybe attributed to an initial varicella infection as previously reported by Spear and Winkelmann.