Dementia is a group of abnormal symptoms due to brain celldamage, which can result in impaired cognition, memory,behavior, and performance of activities of daily living.1 It hasseveral causes, including diseases that directly target the brain, such asAlzheimer’s disease, and vascular dementia caused by chronic diseases.2The World Health Organization (WHO)1 has found the number of adultswith dementia worldwide to be rapidly escalating. At present,approximately 50 million adults have dementia and nearly 10 millionnew cases of dementia are reported every year. According to the FifthThai National Health Examination Survey, the prevalence of dementiain older adults was 8.1%, and this rate increases with age.3
However, older adults with dementia, their relatives, and caregiversare unaware of dementia and its abnormalities occurring and progressinggradually until the patients are unable to perform activities of daily life,such as their jobs or social events.4 Consequently, impacts were foundin several areas. Dementia can cause individuals to become uncooperativewith caregivers. Furthermore, families and caregivers require assistanceand knowledge to care for older adults with dementia.5 Low-andmoderate-income countries, in particular, have budgetary and personnellimitations in arranging efficiently adequate health care and socialservices.6 In Thailand, the cost of care for individuals with dementia isapproximately 600,000-800,000 baht per year for high-pricedmedications.7
WHO developed the 2017-2025 Global Action Plan on thePublic Health Response to Dementia, which includes guidelinesfor the care and treatment of adults with dementia. Preventionis prioritized by minimizing dementia risk factors, earlydiagnosis, care and treatment, and assistance and support forfamily caregivers. Moreover, information systems for dementiawere proposed in the document as a method for communicatingresearch projects and innovations.8 In addition, the WHO9expects a campaign in each country for reducing dementia riskfactors, providing support and training caregivers in communitybasedcare. In Thailand, the 2nd National Plan on the Elderly(2002-2021) has set up policy for the care of older adults.Regardless, there are limited health care services for olderadults in communities and proactive work in protecting thehealth of older adults. Thus, the Ministry of Public Health hascreated community networks for continuing care of olderadults.10
Literature review of competency development in VHVsshows that the efficacy of VHVs has improved in variousareas such as home visits, home-based palliative care forpatients, and providing care for stroke patients.11-13 A studyin Japan found that health volunteers provide care to reducedepression in older adults,14 and palliative care forterminally ill patients.15 In Thailand, VHVs are key leadersin the performance of public health work in communities,but VHVs have been found to perform well in short-termproject work such as data surveys, campaigns on variousissues, disseminating news and information. Regardless, thereare various limitations to long-term work such as providingcare for chronic disease patients.16
In Sakon Nakhon province, community nurse practitionersplay an important role in contributing to knowledge onchronic care for VHVs once a month as a routine program atSakon Nakhon Municipality Public Health Service Centers.However, improving health knowledge alone does not ensureVHVs will have confidence in practice. Therefore, it is necessaryto build perceived self-efficacy as a key factor to bridgeknowledge and performance.17 Thus, a self-efficacy promotingprogram, based on Self-Efficacy Theory developed by AlbertBandura,18 has been introduced to VHVs to enhanceknowledge and perceived self-efficacy for dementia screeningin older adults. Four resources are used including masteryexperiences, vicarious experiences, verbal persuasion, andphysiological and affective states. The program includesdementia knowledge and screening performance in older adultsand group discussion for sharing experiences and problemsolving. As a community nurse practitioner, the researcher isinterested in examining the effects of self-efficacy promotingprogram on VHVs’ knowledge and development of VHVsefficacy for dementia screening. This program will help VHVsin dementia screening for early detection in order to refer tonurses and health care team for diagnosis and propermanagement.
Population and Sample
This quasi-experimental research designed with a twogroup pre-test-posttest design was conducted to answerresearch objectives after approval by the Institutional ReviewBoard, Faculty of Medicine, Ramathibodi Hospital, MahidolUniversity (ID 04-59-38). Willing participants were villagehealth volunteers (VHVs) in the Sakon Nakhon MunicipalityPublic Health Service Centers, Thadcherngchum Sub-district,Muang District in Sakon Nakhon Province, Thailand. Thestudy ran from July-August 2016, and all participants met theinclusion criteria including:
The exclusion criteria was having attended the programless than 4 times.
The sample size was calculated using the G* Powerprogram.20 The effect size was set at 0.80 in line with a previousstudy21 with statistical power at 0.80, p value at 0.05. Thesample size equaled 21 participants with an additional 40%for a final sample size of 30 participants in each group for atotal sample size of 60 participants. Two health centers ofSakon Nakhon Municipality Public Health Service Centerswere randomly divided into the experimental and controlgroups. The potential participants in each group wererecruited into this study based on inclusion criteria.
Instruments
Instruments are divided into the following two parts:
Part 1: Instrument for intervention
1. The intervention program: The self-efficacy promotingprogram for dementia screening in older adults was appliedto the community activities of the Alzheimer’s Disease andRelated Disorders Association (ARDA) for caregivers ofolder adults with dementia and activities were developedbased on the conceptual framework of Bandura’s Self-EfficacyTheory.18 This program consisted of instruction,video presentations, four learning activities of brainassessment and stimulation at the 1st week, practicedementia screening in older adults in the community at the2nd week, group processes at the 3rd week and post- test atthe 4th week. This program was examined for contentvalidity by three experts, including a physician, a care ofcommunity-based older adults, and an advanced practicenurse in older adult. The content validity index (CVI) ofthis program is equal to 1.
2. The routine program: Information about dementiaconsisted of teaching dementia screening, caring once amonth and giving out a dementia handbook.
Part 2: Instruments for data collection:
1. Demographic questionnaire, a fill-in-the-blank andmultiple-choice questionnaire containing 13 items createdby the researcher.
2. Dementia knowledge questionnaire developed byresearcher based on the literature review having 20 itemswith 15 positive items. Each item had two answers valuedat zero point and 1 point. Total scores ranged between 0-20points in which a high total score meant the VHVs had ahigh level of dementia knowledge. This questionnaire hadCVI = 1 and KR-20 (Kuder-Richardson Reliability) = 0.80.
3. The perceived self-efficacy for dementia screening inolder adult’s questionnaire developed by researcher basedon the literature review with 20 items. The responses wererated on 5-level Likert scales with total possible scoresranging between 20 and 100 points in which a high scoremeant the VHV had a high level of perceived self-efficacyfor dementia screening. This questionnaire had a CVI of0.95 and the Cronbach’s Alpha Coefficient was 0.88.
Data collection
After participants signed the informed consent form, theresearch assistants collected data using the demographicquestionnaire, the knowledge of dementia, and the perceivedself-efficacy for dementia screening in older adult’s questionnairein both groups. The experimental group participated in selfefficacypromoting program over 4 weeks including knowledgedementia, dementia screening and video presentations for 2hours using vicarious experiences. Demonstration of four learningactivities included assessment of brain capacity, numericalcalculations/drawings, folding pandan leaves with the hand, andshaping a ball with the feet by using verbal persuasion withphysiological and effective state and vicarious experience. Theseactivities stimulate brain functions by head, hand, and feetexercises. Assignment to practice dementia screening in olderadults in the community was conducted to promote masteryexperience. The group process was integrated to motivateexpression of opinions about the screening experiences withverbal persuasion and additional physiological and affectivestates in problem-solving and overcoming barriers. On theother hand, the control group received routine program oneducation once a month and were given a dementia handbook.After both groups completed the program, the participants weremeasured for the knowledge of dementia and the perceivedself-efficacy for dementia screening in older adult (Figure 1).
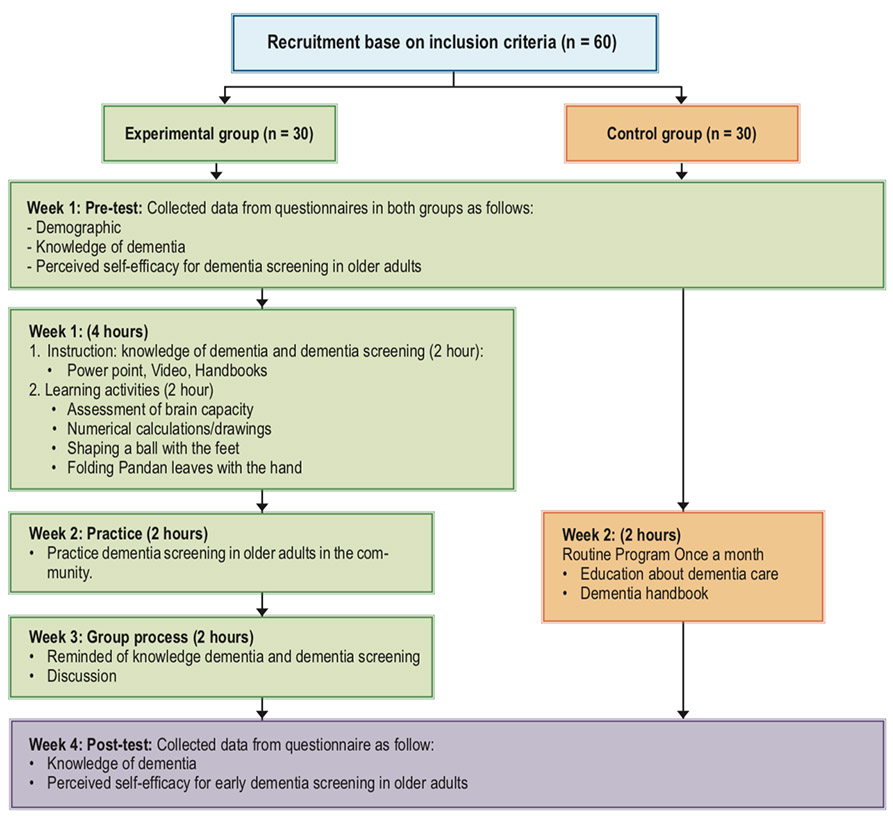
Figure 1: Process of VHVs programs
Data Analysis
The data obtained was analyzed with a computer program.The demographic data of participants and dependent variableswere analyzed by using descriptive statistic of percentages,mean, and standard deviations. Chi-square test, independentt-test, and Mann-Whitney were conducted to examine thedifference in the demographic data, and dependent variablesbetween the experimental and control groups. Comparison ofmean score on dementia knowledge and perceived self-efficacyin dementia screening in older adults within the groups byusing Wilcoxon signed rank test and paired t-test.
From a total of 60 VHVs, most of the experimental andcontrol groups were female, with a mean age of 54.97 years(standard deviation: SD = 7.91) and 54.53 years (SD = 9.11)respectively. Approximately half of each group was married(56.70% and 53.30%, respectively). In terms of educationlevels, both groups were similar, at elementary level or lower(43.30% and 56.70%, respectively). Both groups had an equalnumber of Buddhists. Two in three of the experimental groupwere employed and in service as VHVs, while only half of thecontrol group was employed (76.70% and 56.70%, respectively).In both groups, none of the participants had experiences inproviding care for dementia patients, and had no older adultswith senility in their families. However, one in three of theVHVs in each group had received instruction about dementiafrom various sources, namely, brochures and online media.The mean monthly incomes in each group was similar at 4,640Baht (SD = 3,432.76) and 5,400 Baht (SD = 2,676.20); thelength of time the participants had resided in the area weresimilar at 35.40 years (SD = 16.77) and 32.30 years (SD =13.33). The period of time for the VHVs in each group wasalso similar at 10.03 years (SD = 5.75) and 11.70 years (SD =5.72). The number of households under the VHV’s responsibilitywere similar at 22.17 households (SD = 8.98) 23.07 households(SD = 8.14). The participants’ demographic had no significantdifference between the experimental and control groups usingChi-square test, and independent t- test (p > 0.05).
Before analysis of data, mean scores of dementia knowledgeof both groups and perceived self-efficacy in dementia screeningin older adults of the control group did not have normaldistribution. Before the program, mean scores of dementiaknowledge and perceived self-efficacy in dementia screeningin older adults were not different when compared with thecontrol group using Mann-Whitney U test (z = -0.50, p > 0.05,z = -1.70, p > 0.05, respectively) as shown in Table 1.
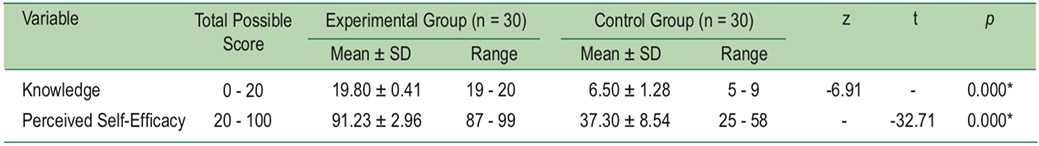
After participating in the program, the experimental grouphad significantly higher mean for knowledge dementia andperceived self-efficacy in dementia screening in older adultsthan before the program (z = -4.81, p < 0.001; t = -35.32,p < 0.001, respectively) and the control group (z = -6.91,p < 0.001; t = -32.71, p < 0.001, t = -32.71, p < 0.001) as shownin Table 2&3.
Table 1: Comparison between mean scores of dementia knowledge and perceived self-efficacy for dementia screeningin older adults between experimental group and control group before the program by using Mann-Whitney U test (n = 60).
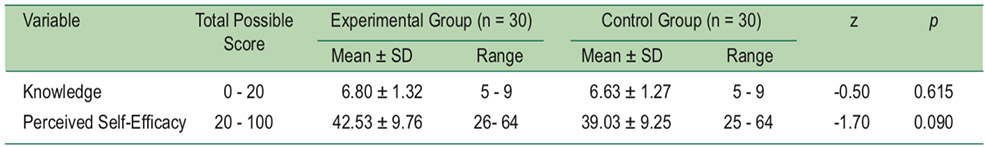
Table 2: Comparison of mean scores of dementia knowledge and perceived self-efficacy for dementia screening in olderadults Pre-test and Post-test the program by using Wilcoxon signed rank test and paired t-test (n = 30).
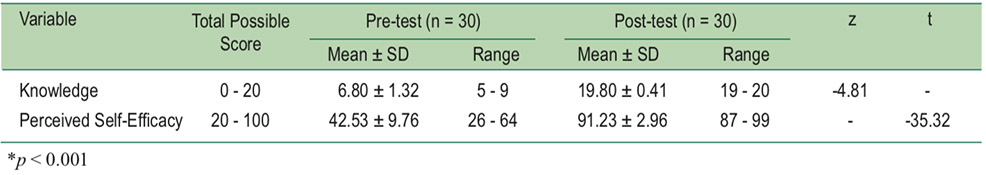
Table 3: Comparison of mean scores on dementia knowledge and perceived self-efficacy for dementia screening in older adultsafter the program between experimental group and control group by using Mann-Whitney U test and independent t-test (n = 60).
After taking part in the self-efficacy promoting programfor dementia screening in older adults, the experimental grouphad a mean score on knowledge of dementia and a perceivedself-efficacy for dementia screening in older adults higherthan before the intervention and the control group (p < 0.001).VHVs in the experimental group received the self-efficacypromoting program integrated by Bandura’ self-efficacytheory through experiences, building their confidence andenhancing their knowledge of dementia knowledge. Theygained experience in dementia screening using the fourresources: vicarious experience through the cognitive processby health education, including etiology, symptoms, screening,treatment and prevention using brain fitness, for people withdementia, via PowerPoint, video presentation and handbooksof dementia; enactive mastery experience, verbal persuasionand physiological and affective states through the motivationalprocess by demonstration and return demonstration using manystrategies for brain exercise, such as numerical calculations,shaping ball with the feet and so on. In addition, the groupprocess provided for solving problems of dementia screeningin older adults in the community by delivering verbal persuasionwith physiological and effective state. Hence, this result iscongruent with previous studies that self-efficacy promotingprogram could increase knowledge and self-efficacy of VHVsfor dementia screening in older adults leading to increasedhigher scores on perceived self-efficacy than before theexperiment17,23 and the control group.24
The self-efficacy promoting program should be applied toVHVs in order to enhance dementia disease knowledge andself-efficacy for dementia screening in older adults in thecommunity. Therefore, the self-efficacy promoting programshould be useful for other similar VHVs characteristics orcaregivers of people with dementia to prevent onset or reportearly detection in older adults in the community. Furtherresearch should be conducted to follow up after a period ofone year on the self-efficacy of VHVs in knowledge andscreening for dementia in older adults.
This study was supported in part by the Theses Grant,Graduate Faculty, Mahidol University, Thailand. We wouldlike to thank all staff from Municipality Public Health ServiceCenter I and Center II for their help and contributions that ledto the success of this study.