Diffuse idiopathicpulmonary neuroendocrine cell hyperplasia (DIPNECH) is a generalized proliferation of scattering single cells, small nodules (neuroendocrine bodies) or linear proliferations of neuroendocrine cells of lung. They may be confined to the bronchial and bronchiolar epithelium, include local extraluminal proliferation (tumorlets), or progress to the develop- ment of carcinoid tumor. Sometimes DIPNECH is accompanied by intra- and extraluminal fibrosis of the involved airways.1,2 It is rare and presents typically in the fifth or sixth decades and is more common in woman.
The great majority of pulmonary tumorlets are found incidentally and show no clinical consequence.Only rare occasions bronchopul- monary lymph node metastasis were reported.3,4,5 DIPNECH and tumorlets may associated with Cushing syndrome,6,7 elevated serum CEA.8
A 60-year-old asymptomatic Thai female with history of mild hyperglycemia, hyperlipidemia and hyperuricemia had high and rising serum CEA levels (Figure 1).The chest x-ray and tomosyn-thesis(Figure 2a-b) showed subsegmental atelectasis and reticular infiltration at the right middle lobe. CT Chest (Figure 3) showed small pulmonary atelectasis at right middle lobe.
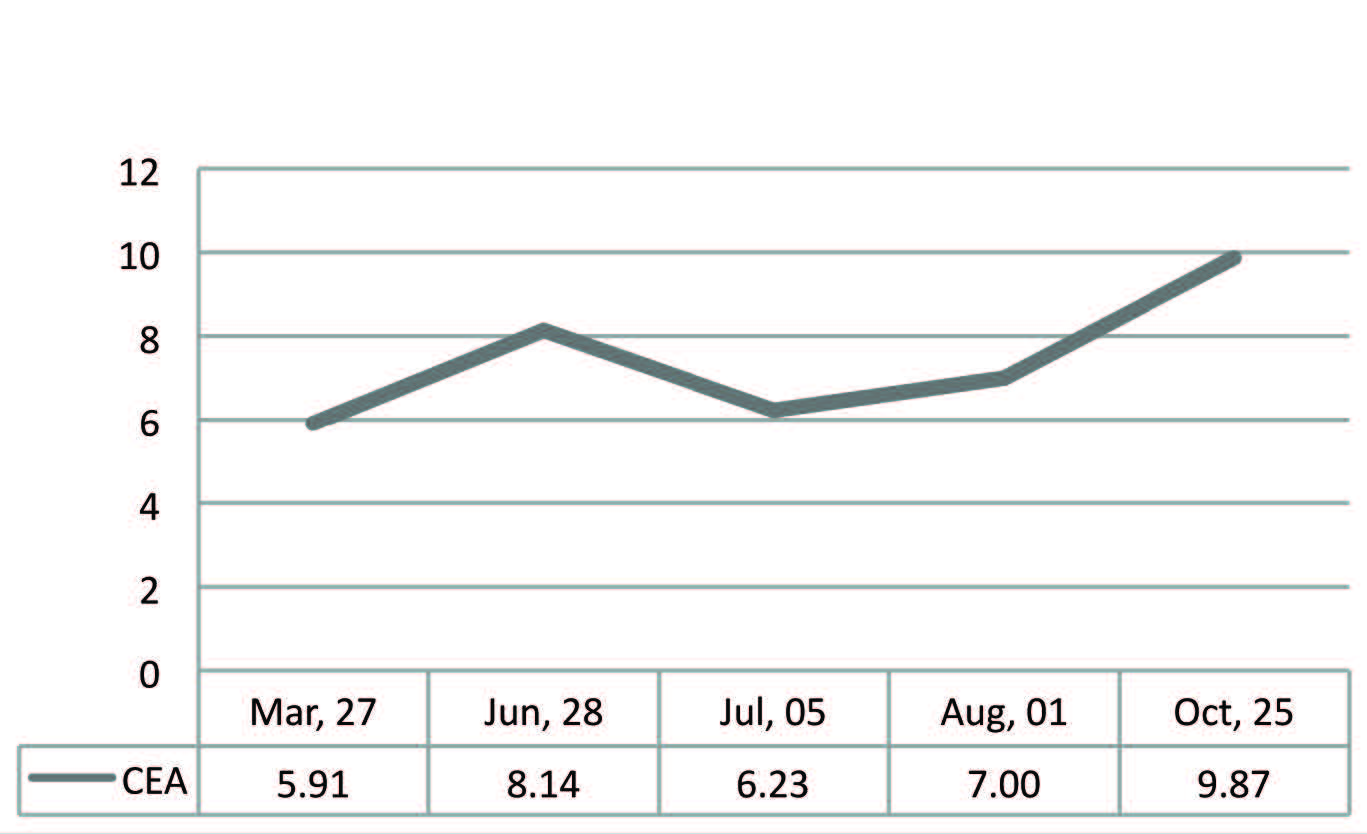
Figure 1: Graph shows rising serum CEA
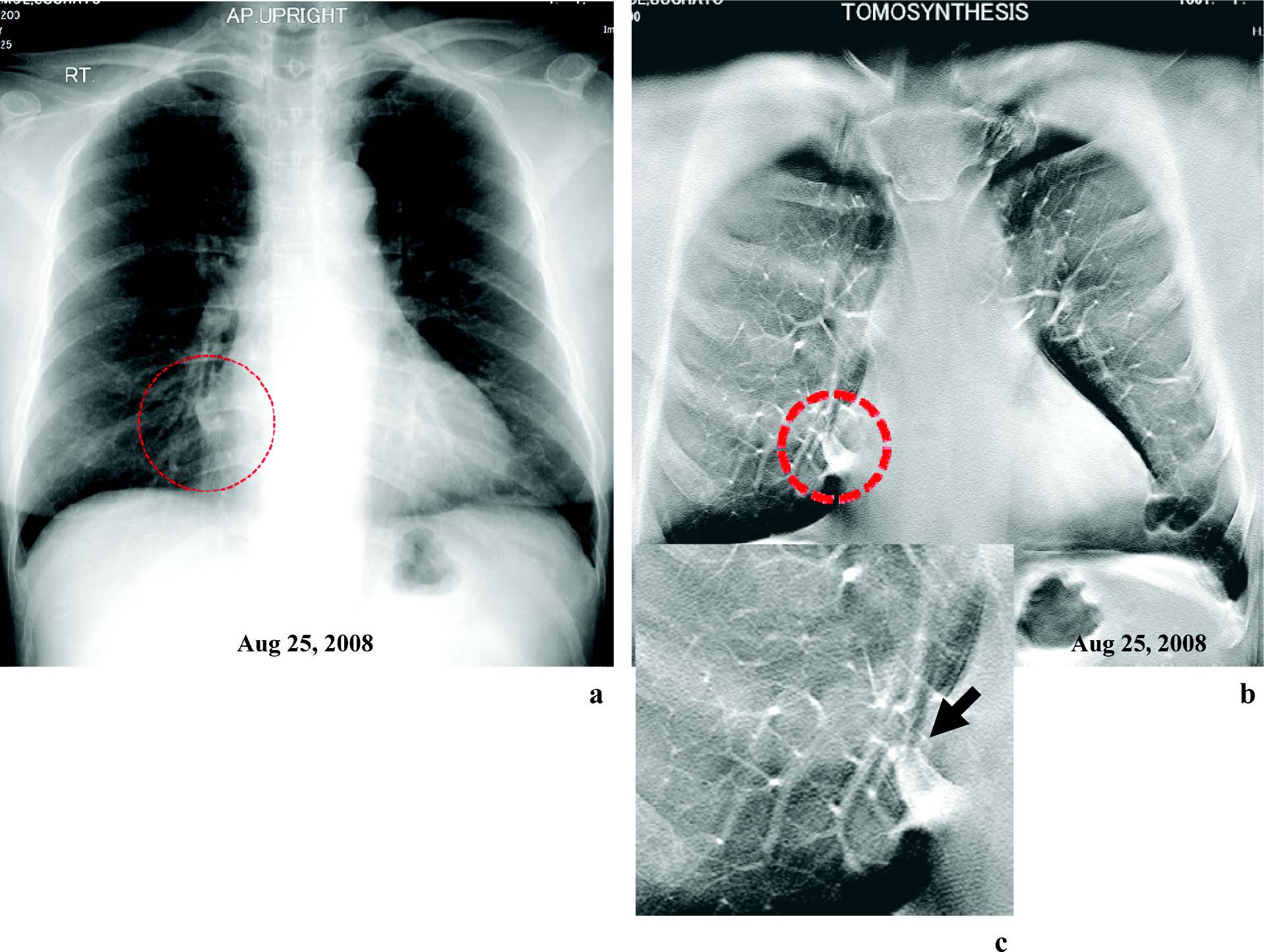
Figure 2: Chest x-ray (a) and Chest Tomosynthesis (b, c) show subsegmental atelectasis and reticular infiltration at right middle lobe.
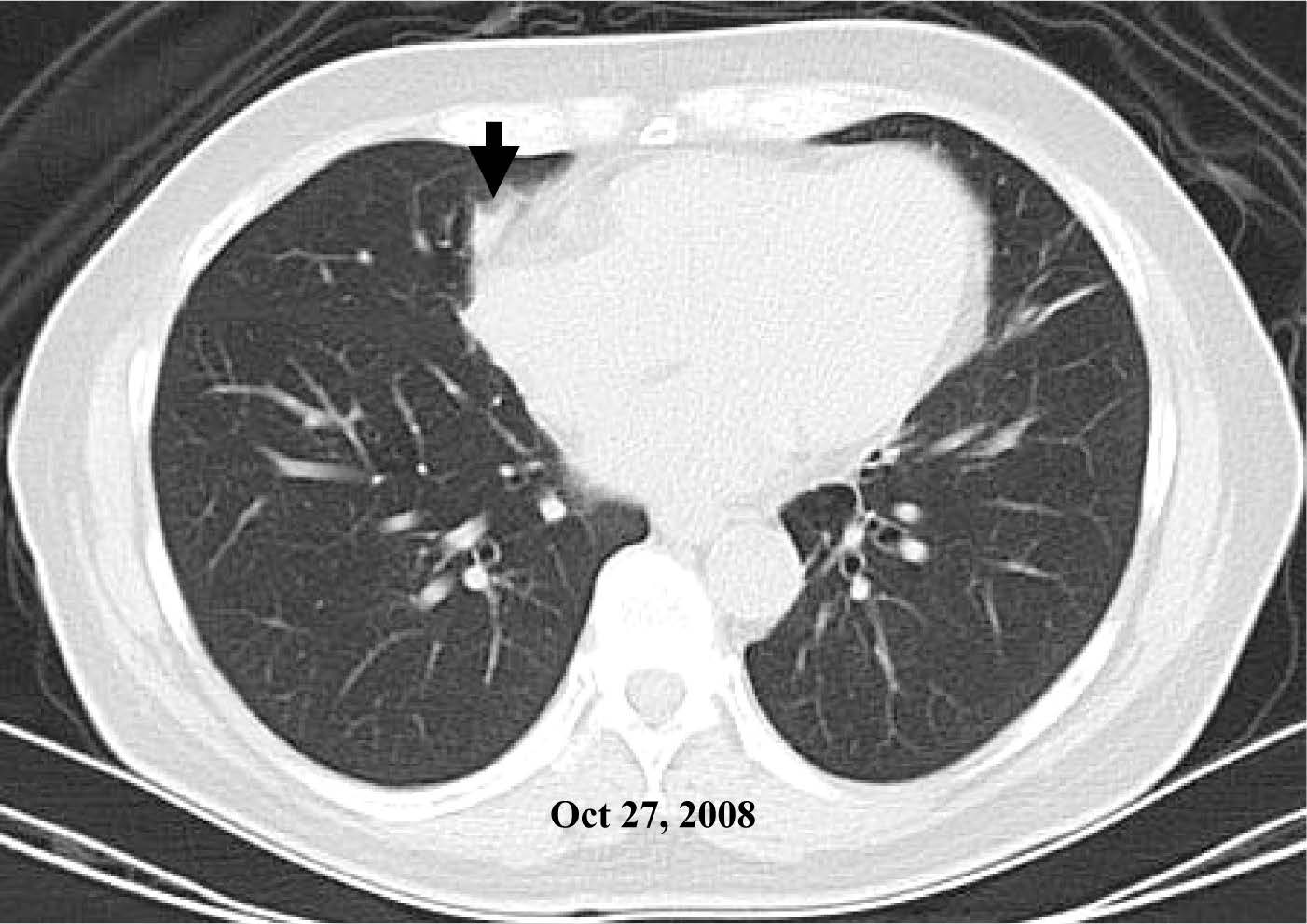
Figure 3: CT Chest shows small pulmonary atelectasis at right middle lobe.
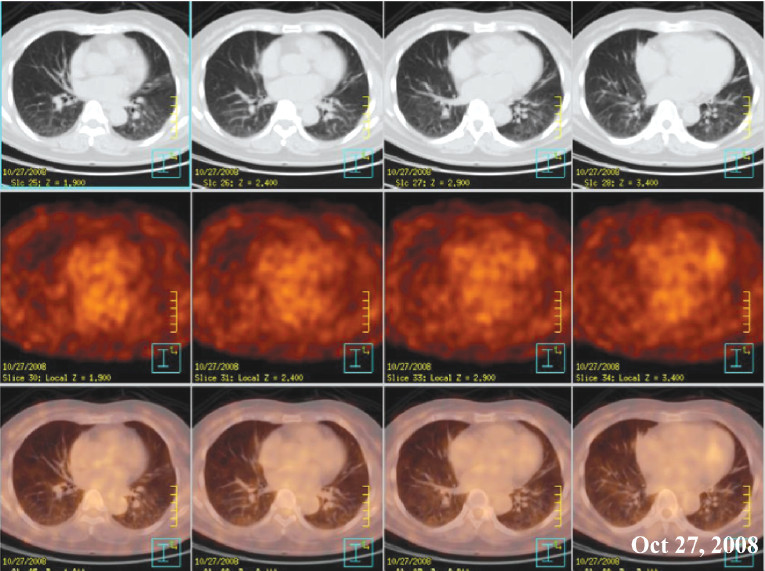
Figure 4: The F18-FDG-PET/CT show non-FDG avid lesion in right middle lobe, which could be a benign lesion. Pulmonary tumorlets and bronchioalveolar carcinoma may also be non-FDG avid lesion.
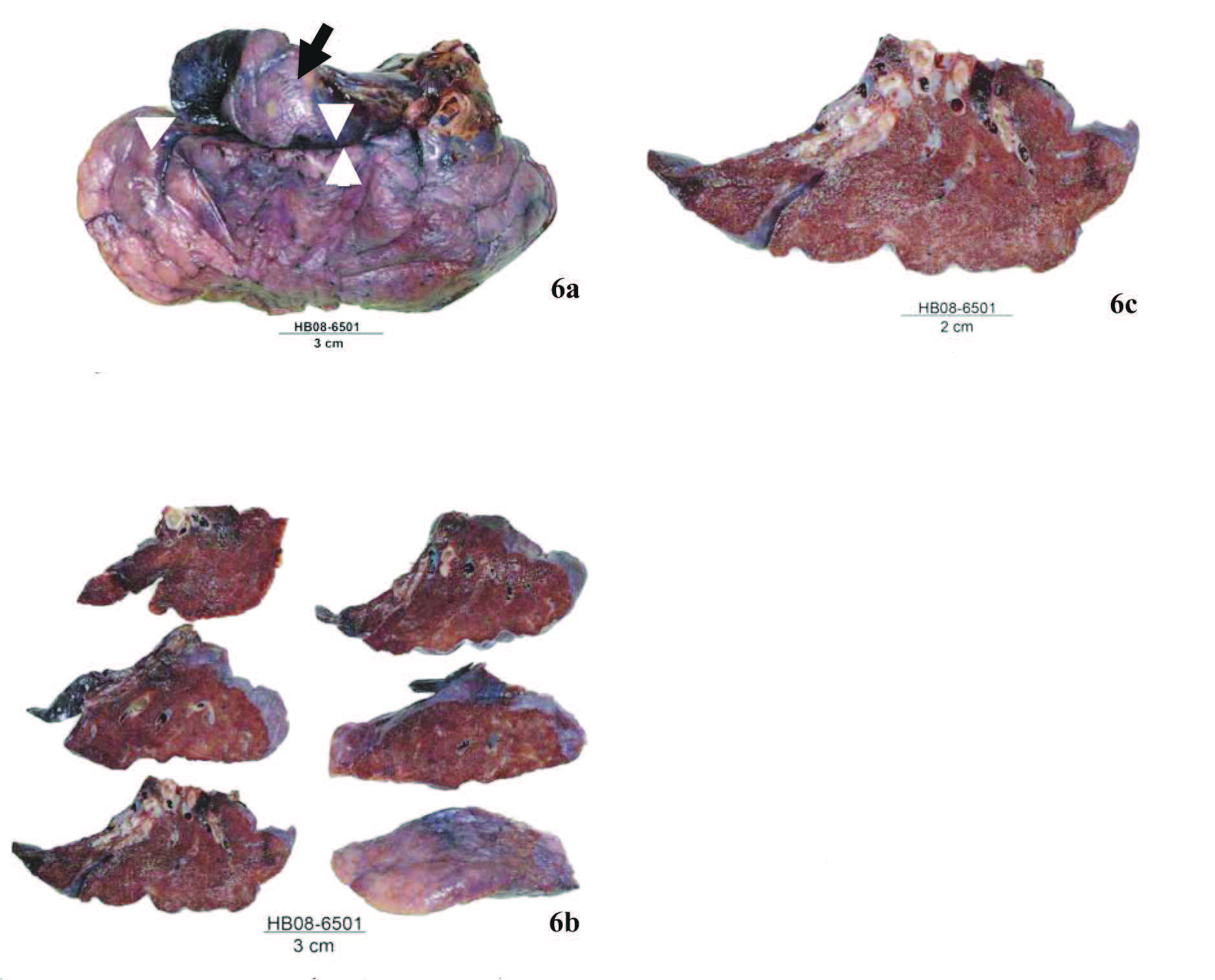
Figure 6a: The right middle lobe shows one accessory lobe (arrow ) superior to a minor fissue (arrow head)
Figure 6b: Serial near horizontal sections of the right middle lobe show no visible tumor nodule.
Figure 6c: The accessory lobe shows areas hemorrhage, atelectasis and clusters of dilated brochi.
The F18-FDG-PET/CT (Figure 4) showed non-FDG avid lesion in the right middle lobe, which could be a benign lesion. But pulmonary tumorlets and bronchio- loalveolar carcinoma may also be non-FDG avid lesion.
On gross examination, the right middle lobe of lung showed one minor fissure and one small accessory lobe at the superior part of the lateral segment (Figure 6a). There is no tumor nodule seen in the lung parenchyma. (Figure 6b). One pale tan brown rubbery firm atelectatic area, measuring 2x1x0.8 cm. with clusters of dilated bronchi is noted in the central part adjacent to the minor fissure, extending from the middle lobe bronchus to the peripheral part of lung. The remaining accessory lobe is grey brown and firm. The lung parenchyma is tan brown, focally black and soft. Some dilated blood vessels filled with blood and few brown black nodules of 3 to 4 mm. are noted. (Figure 6c).
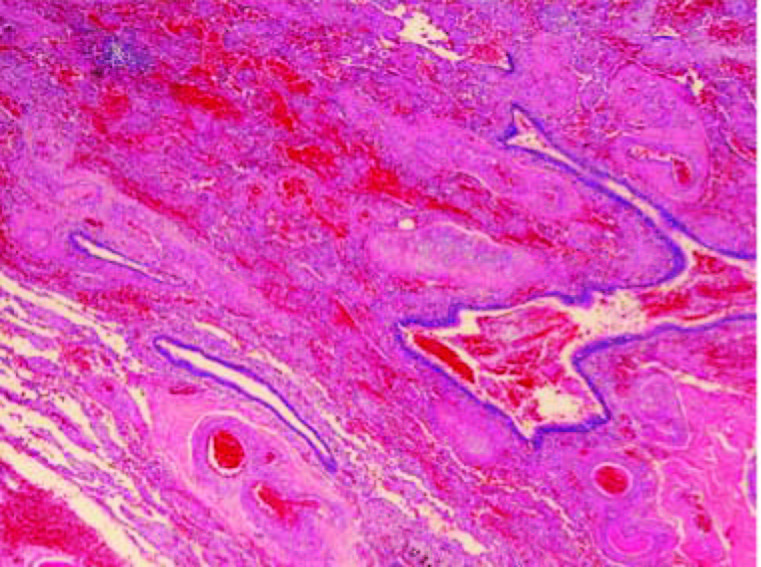
Figure 7: Lung shows areas of hemorrhage, several blood vessels, focal fibrosis and dilated bronchi (HE x20).
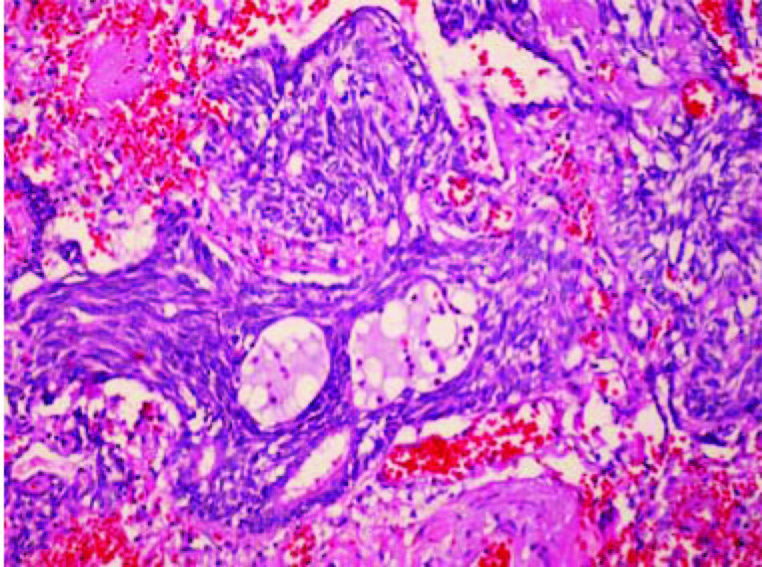
Figure 8a: Lung tissue shows three microscopic tumorlets with hemorrhage and mild focal fibrosis in the stroma.(HE x100).
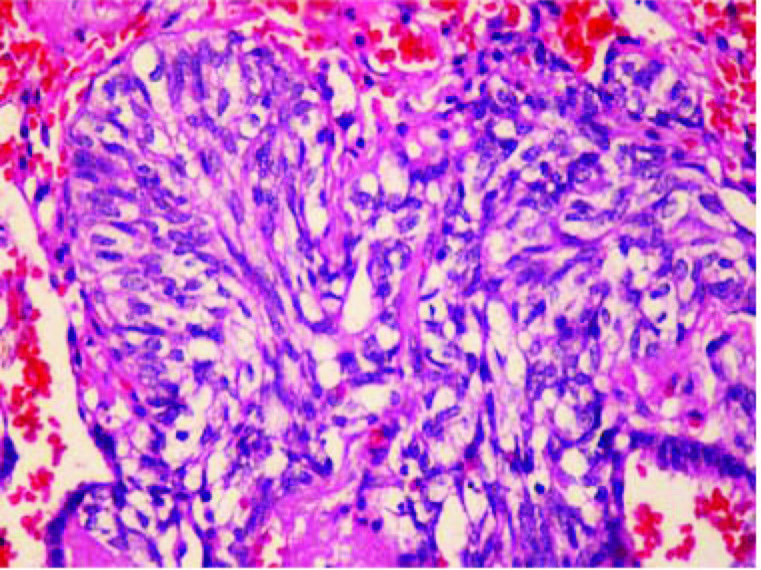
Figure 8b: One tumorlet composing of spindle, polyhedral to oval shape tumor cells with scanty to clear, vacuolated cytoplasm and elongated to oval nuclei with speckled chromatin (HE x200).
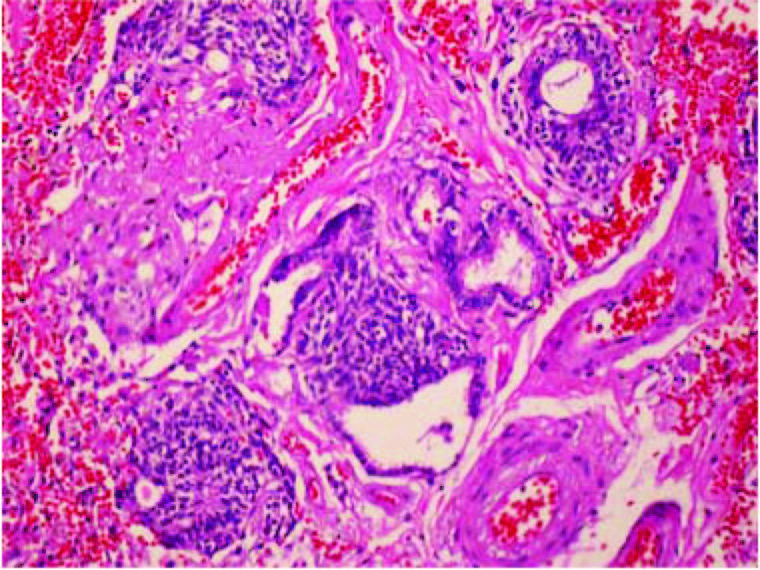
Figure 8c: In this fibrotic, hemorrhagic and vascularized area,there are four terminal bronchi showing neuroendocrine cell hyperplasia (HE x100).
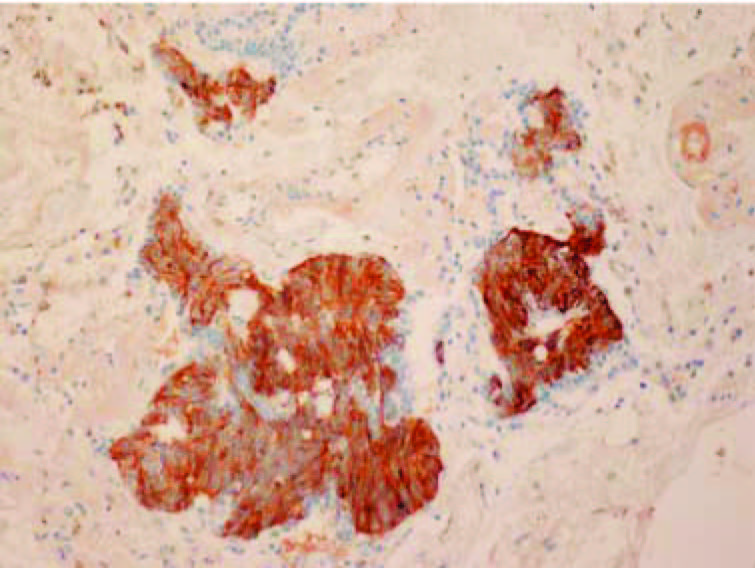
Figure 8d: One tumorlet and three terminal bronchi show neuroendocrine cell hyperplasia (chromogranin A x100).
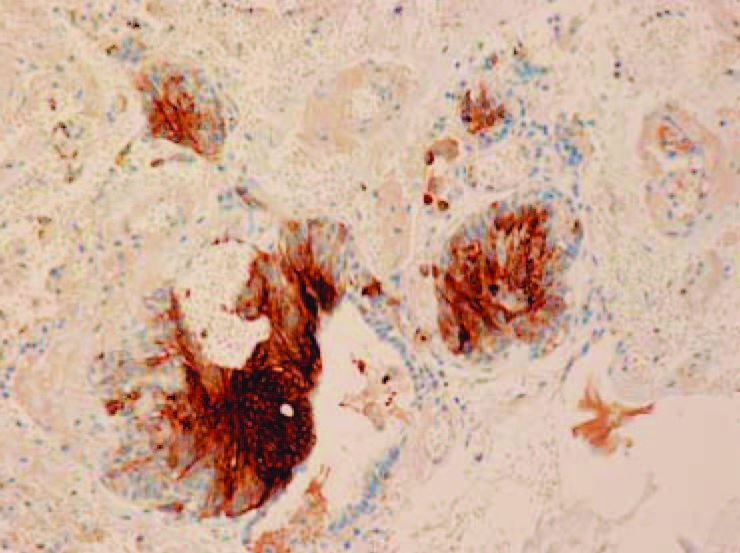
Figure 8e: The tumorlet and foci of neuroendocrine cell hyperplasia are also CEA positive (CEA x100).
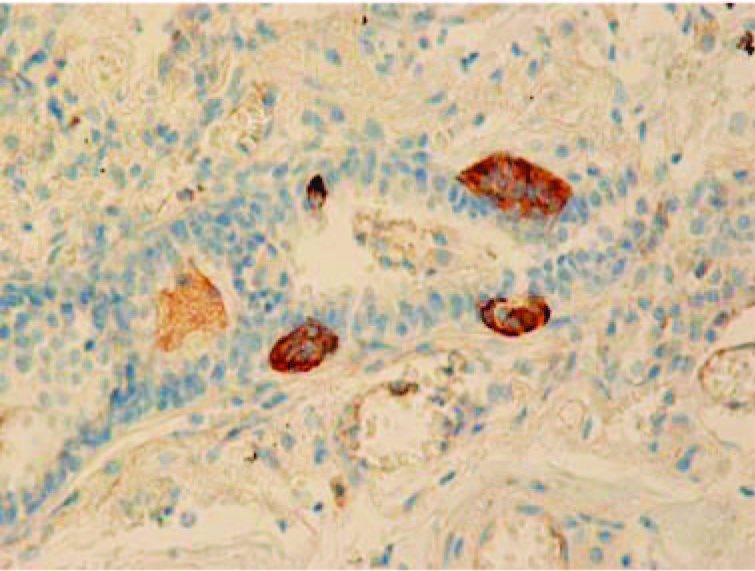
Figure 9: Single, small clusters and one small nodule of chromogranin A positive neuroendocrine cells in the mucosa of one small brochus (Chromogranin A x200).
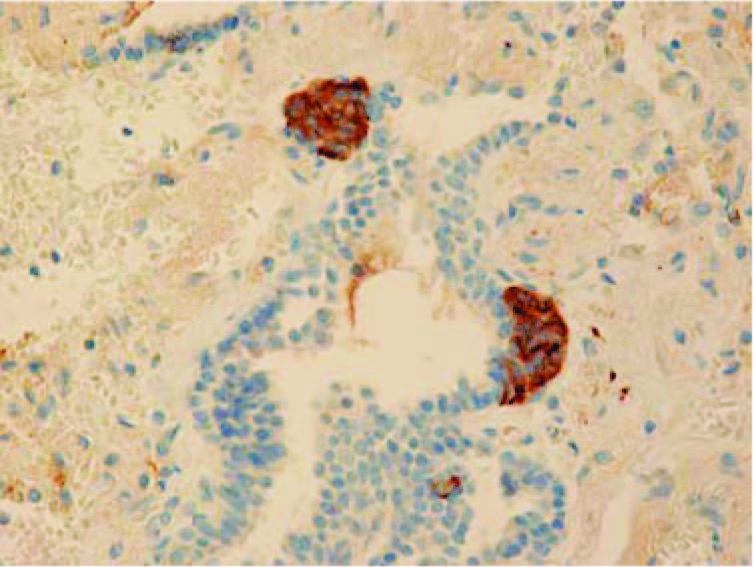
Figure 10: Two small nodules of neuroendocrine cells (neuroendocrine bodies) in the bronchiolar mucosa (chromogranin A x200).
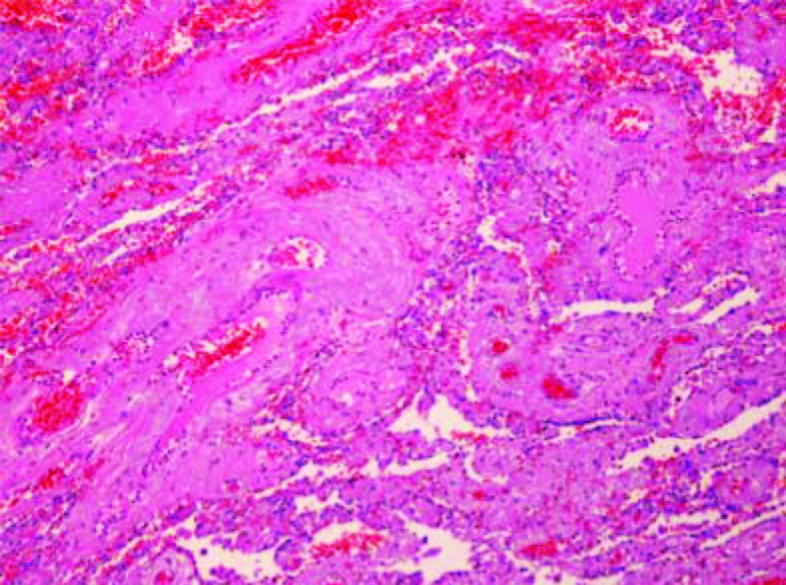
Figure 11: Lung tissue shows areas of vascular malformation and mild hemorrhage (HE x100).
The microscopic examination of the lung revealed areas of severe hemorrhage with several vaious sizes blood vessels, foci of fibrosis (Figure 7), dilated bronchi, multiple small foci of lymphoid cells infiltration and multiple clusters or nests of spindle, polyhedral, oval to round tumor cells with scanty cytoplasm and oval to elongated nuclei with speckle chromatin and few per- ceptable nucleoli (Figure 8a-e).These cells are TTF1 +ve; chromogranina A +ve; CEA +ve but CK 20 –ve. Few tumor cells are CK 7 +ve. There are few mitoses noted. They are tumorlets or carcinoid tumorlets of lung. Many dilated bronchi show mild chronic inflammation and focal fibrosis. Some dilated bronchi in the hemorrhagic areas show occasional thick wall blood vessels and some areas of dilated capillaries and small lymphatics in the lamina propria of the mucosa. Many small bronchi and bronchioles show scattering single, small clusters and nodules of chromogranina A and CEA positive cells in the mucosa (Figure 9-10). The finding are compatible with diffuse pulmonary neuroendocrine cell hyperplasia. Several small blood vessels in the hemorrhagic areas show hyalinization of the wall with occasional foci of increased elastic fibers. Some larger blood vessels show acidophilic areas and increased elastic fibers in the wall. Few blood vessels show mixed aterial and venous walls (Figure 11). The lung parenchyma inferior to the minor fissure shows congestion, occasional foci of hemorrhage, mild emphysematous changes and occasional small foci of mild anthracosis.
Diffuse Pulmonary neuroendocrine cell hyperplasis (DIPNECH) and pulmonary tumorlets can be found in lungs with little to no scarring or less common in lungs severely scarred by bronchiectasis or other inflammatory process.1-5 They may be associated with Cushing syn- drome6, 7 High CEA (33ng/ml) was found in one case of DIPNECH in associations with an adenocarcinoma of a mixed subtype with partial neuroendocrine differentiation of the right upper lobe. The tumor was strongly positive for CK7;CK18; TTF1 and SPA and focally positive for CEA, NSE and chromogranin A. The proliferation rate (Ki67) was 20-30%. The cells of multiple tumorlets and DIPNECH were strongle positive for CD56; synapto- physin, NSE and chromogranin A and focally positive for CK7,CK18, TTF1 with proliferation rate (Ki67) of 1-2%8 Tumorlets were found in one case of pulmonary sequestration with elevated serum progastrin-releasing peptide.9 Tumorlets and carcinoid secondary to congeni- tal broncho-esophageal fistula were also reported.10
The right middle lobe in our case showed one accessory lobe with vascular malformation, hemorrhage and bronchiectasis. These may be suggestive of a minor malformation (?sequestration) The DIPNECH and tumorlets found mainly in the accessory lobe showed positive chromogranin A, CEA and CK7. The serum CEA in her postoperative and follow up period are still elevated and rising. Bronchioloalveolar carcinoma (BAC) less than 5 mm. with rather low number of tumor cells is possible false negative by F18-FDGPET/CT. Slow growing pulmonary neuroendocrine neoplasms with low metabolic activity are often negative F18-FDG-PET/CT.11 These may explained the negative imaging results in our case. Pulmonary tumorlets should be included in the differential diagnosis of a subcentrimeter pulmonary nodule.12
Tumorlets developed from hyperplastic neuroendo- crine cells (Kulchitsky cells) in the bronchial and bron- chiolar mucosa.13 The natural history is unknown. The mechanism of progression may involve critical genetic alteration. There are some reports of Cushing syndrome associated with pulmonary tumorlets. The tumorlets are benign condition but rarely they show lymp node metas- tasis. Since the pulmonary neuroendocrine cells in this patient also secrete CEA (evidence by immunohisto- chenical study), postoperatively rising serum CEA may be suggestion of remaining neuroendocrine cells prolif- eration so recurrent DIPNECH and tumorlets should be aware. On routine CT scan shows small subsegmental atelectasis or small nodule. The other study F18-FDG- PET/CT show no increase uptake. All investigation could not rule out malignant process. Therefore the thoracotomy for lesion removal is recommended. This report is a good teaching case for the pulmonary innfiltration or small nodule which all imagings and laboratory findings do not show the definite diagnosis. The removal of the lesion is indicated.
This case illustrates the difficulty in the preoperative diagnosis of DIPNECH and tumorlets, the definite diag- nosis can be made by pathologic examination.