Urothelial carcinoma is the most common malignant neoplasm in the urinary tract.1-2 This malignancy affects approximately 33,000 people each year and increases in morbidity and mortality.1,2 The standard diagnosis is commonly made by cystoscopy with tissue biopsy; however, such diagnostic method is rather invasive and inconvenient in routine clinical practice. Therefore, the urine cytology becomes increasingly useful for urothelial cancer screening in a high-risk patient.2-5 Proposed by Papanicolaou and Marshall, urine cytology was initially classified into five classes, which loosely related to histological classification.6-8 The Papanicolaou Society of Cytology later revised the urine cytological classification in concordance with World Health Organization (WHO) classification of tumors of urinary system and male genital tract.9
However, detection of urothelial carcinoma has low sensitivity when the sample is prepared conventionally. More recently, liquid-based c ytology (LBC) plays an important role in cytological diagnosis, particularly in a group of high volume but low cellularity specimens such as urine and cerebrospinal fluid. Exclusively urine cytology, liquidbased cytology has been proved to get the better yield to diagnose urothelial carcinoma when compared to conventional methods.10 This invention renders urine cytology more sensitive and nowadays are used as screening and diagnostic tools for detection of urothelial carcinoma particularly a group of high-grade urothelial carcinoma (HGUC) in combination with cystoscopy and tissue biopsy diagnosis in several medical centers.2,11
In the Thai population, urothelial carcinoma is the eighth most common cancer but urine cytology is not widely used and there are only a few studies on this tool.11 Our institute has been applying liquid-based cytology to evaluate urine specimens for several years. This retrospective study aimed to validate the accuracy of urine cytology and histopathology in our center.
This study is a retrospective cross-sectional study, approved by the Committee on Human Rights Related to Research Involving Human Subjects of our faculty. Subjects included all urine cytological specimens examined from 2013 to 2016, which had accompanying histological tissue samples collected concurrently or within one year after cytological diagnosis. All cytological specimens were prepared using liquid-based cytology technique. Samples of which either glass slides or paraffin blocks could not be retrieved for secondary reviews and unsatisfactory cytological or histological materials were excluded from this study. Data collected from each subject was categorized as follows: age, gender, types of cytological specimen collection (voided urine or instrumented material) and types of histological specimen (biopsy, transurethral resection of bladder tumor (TUR-BT), or organ resection). The urine cytological diagnoses were categorized into 3 groups: 1) negative, 2) atypia or low-grade urothelial neoplasm, and 3) suspicious for malignancy or malignancy. Histological diagnoses were classified into 1) negative or unremarkable, 2) benign neoplasm, atypia, low-grade papillary urothelial carcinoma, and 3) high-grade papillary urothelial carcinoma, carcinoma in situ or infiltrating urothelial carcinoma; of any site within the urinary tract. All discordant cases between cytology and histopathology were reviewed separately by cytopathologists and an uropathologist. The statistical analysis was performed by Statistical Package for the Social Sciences (SPSS) for Windows, Version 16.0. Chicago, SPSS Inc; 2007.
A total of 211 cases from 2013 – 2016 were included. Mean age was 66.3 years (23-92 years). Peak of age groups was 60-79 years (59%). The sample group is composed of almost equally male (54%) and female (46 %). Characteristics of specimens were summarized in Table 1. Types of specimen were more instrumented material (77.3%) than voided urine (20.4%). The correlation between cytological and histological diagnoses was demonstrated in Table 2.
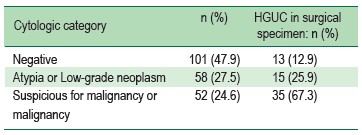
Rate of high-grade urothelial carcinoma for each urine cytological category was 12.9%, 25.9% and 67.3% in negative category, atypia or low-grade urothelial neoplasm category and suspicious for malignancy or malignancy category, respectively. The sensitivity and specificity of high-grade urothelial carcinoma screening in suspicious of malignancy cases or malignancy of urine cytology category were 55.6% and 88.5%. Positive predictive value and negative predictive value were 67.3% and 82.4%.
Twenty-eight out of 211 samples (13.3%) with histologically confirmed high-grade urothelial carcinoma were reported negative (13 cases) and atypia or low-grade urothelial neoplasm (15 cases) in urine cytology. Urine cytological slides and corresponding histological materials of these cases were reviewed and most of these cases demonstrated either low cellularity or prominent inflammatory cells without recognizable neoplastic cells in urine cytology. Four of these cases had a tumor located at the upper urinary tract (renal pelvis and ureter).
Seventeen cases (8.1%) presented with suspicious cells or malignant-liked cells in urine cytology, but without evidence of high-grade urothelial carcinoma in histology were reviewed. Most of them demonstrated suboptimal tissue samples; including too small pieces (only stromal tissue fragments), superficial fragments, distorted tissue, severe inflammation causing obscuring artifact and reactive atypia of urothelial cells in inflammatory process; e.g. polypoid cystitis and granulation tissue. However, two of these cases demonstrated malignant histological diagnosis on subsequent tissue samples. One was carcinoma in situ of the urinary bladder and another was high-grade urothelial carcinoma of the prostatic urethra.
Table 1: Characteristics (n = 211)
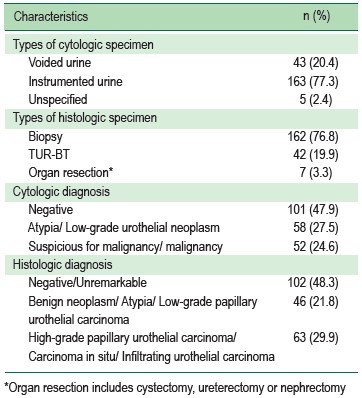
Table 2: Rate of high-grade urothelial carcinoma (HGUC) in each urine cytologic category
Urine cytology is simple and non-harmful investigation for screening and detection of high-grade urothelial carcinoma. It provides essential information for physicians to plan for further management and investigation to get definitive diagnosis. Before an era of liquid-based cytology, the cytological detection of malignant cells in urine was low sensitivity due to high volume but low cellularity. Nowadays, liquid-based cytology plays an important role and greatly improved the quality of urine cytological diagnosis; especially for high grade urothelial carcinoma.2,10,11
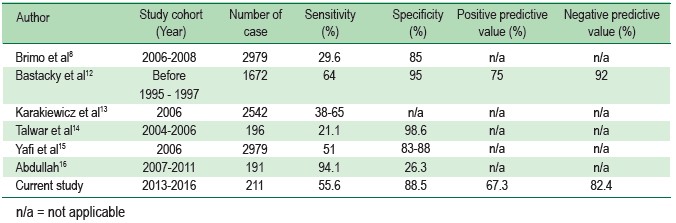
In this study, the sensitivity and specificity for detection of high-grade urothelial carcinoma in urine cytology are 55.6% and 88.5%, respectively. In comparison with previous studies concluded in Table 3, the sensitivity and specificity are similar to those of other studies (sensitivity 21.1 to 85% and specificity 26.3 to 98%).8,12-16
From those preceding studies, causes of false negative cases in urine cytology were no detectable tumor cells, rarely Conclusion Urine cytology is a valuable and practical tool for urothelial carcinoma screening; especially high-grade urothelial carcinoma and early invasive lesions. Although urine cytology has rather less sensitivity, its specificity is high. This helps the physician to screen high-risk individuals who need further investigations such as subsequent cystoscopy or surgery with confidence. However, a negative or false-negative result may not be entirely excluded of carcinoma. In these patients, close follow-up or investigations with other diagnostic tools are needed for inclusion/exclusion of urothelial carcinoma. Thus, a combination of clinical information, urine cytological diagnosis and histopathological diagnosis is the best practice for making a definitive diagnosis, leading to appropriate management and follow-up of patients. found suspicious or malignant cells with human errors, suboptimal material and degenerative changes of atypical or malignant cells; especially in voided urine specimen.8,12,16 The false positive cases are frequently related to atypical reactive changes in instrumented materials or previous therapeutic process.12,16 When compared to this study, the false negative urine cytology is related to no detectable malignant cell in samples and the tumor of upper urinary tract origin. Cases with false positive cytology are related to suboptimal tissue biopsy; including small biopsy, tissue artifact and reactive atypia from severe inflammation. In addition, few false positive cases are carcinoma in situ of urinary bladder and invasive carcinoma of prostatic urethra; which were undetectable during the concurrent cystoscopy.
As a result, the most important factors to get high diagnostic accuracy on urine cytology depends on experience of cytopathologists and adequacy of specimens. Therefore, integration of information including cytology, histopathology and clinical findings would be required to make the exact diagnosis for proper management.
Table 3: Comparison of sensitivity, specificity, positive predictive value and negative predictive value of the current research with other previous studies
Urine cytology is a valuable and practical tool for urothelial carcinoma screening; especially high-grade urothelial carcinoma and early invasive lesions. Although urine cytology has rather less sensitivity, its specificity is high. This helps the physician to screen high-risk individuals who need further investigations such as subsequent cystoscopy or surgery with confidence. However, a negative or false-negative result may not be entirely excluded of carcinoma. In these patients, close follow-up or investigations with other diagnostic tools are needed for inclusion/exclusion of urothelial carcinoma. Thus, a combination of clinical information, urine cytological diagnosis and histopathological diagnosis is the best practice for making a definitive diagnosis, leading to appropriate management and follow-up of patients.