The World Health Organization (WHO) aims to eliminate global tuberculosis (TB) by 2035.1 Thailand is one of the TB burden countries. WHO estimated the incidence of 172 cases per 100,000 population, 2,700 cases of drug-resistant TB and a case fatality ratio of 0.11 in 2016.2 Songklanagarind hospital provides care for nearly 1,000 pulmonary TB patients per year including those with multi-drug resistance or total drug resistance. TB transmits through inhalation of Mycobacterium tuberculosis- contaminated droplets. Infection may slowly progress from an asymptomatic latent tuberculous infection (LTBI) to symptomatic TB over a period of years.3 Moreover, healthcare workers (HCW) can be at risk of TB infection due to contact with such patients.4 However, the early management of LTBI in HCW can prevent symptomatic TB and the transmission of TB in hospitals. Systemic testing and treatment for LTBI should be considered in health care workers at risk.5 Medical students are also at risk for TB infection during their clinical years.6-10 TB control in healthcare settings plays an important role in limiting transmission from patient-to-patient, patient-to-healthcare worker and healthcare worker–to-patient.1,11 Tuberculin skin test (TST) is a classic, widely-used and affordable screening tool for LTBI.12,13 Casas et al found that annual TST conversion in HCW has declined during the 20-year period of their study. This may directly reveal the effectiveness of TB control measures in healthcare settings.14 Albuquerque da Costa et al showed that TST conversion probability in the Kaplan-Meier curve had significantly reduced after TB administrative measures were introduced in 1998.15 Many TB control measures have been continuously implemented in Songklanagarind hospital since 2005 (e.g., mechanical ventilation, the TB screening system, the one-stop TB service and the Airborne Infection Isolation Unit) TB control assessment is a decisive tool for TB administrative control. The tool should include local epidemiological, climatic and socioeconomic status alongside TB and HIV burden.1 Songkla- nagarind hospital has provided an annual voluntary TST for medical students before and during their clinical year. Epidemiological study of LTBI through TST records in medical students may indirectly evaluate nosocomial TB control and TB training in medical students. This study aimed to evaluate trends in serial TST survival from 2001-2016 with TB control implementation.
Records of TST results from the infection control unit were used. The following details show how the TSTs were done and interpreted.
TST for medical students in Songklanagarind hospital
Infection control unit provided voluntary TST with 0.1 ml of PPD-TRC (Thai Red Cross tuberculin protein, equivalent to 5 TU of PPD-S) on the volar surface of the forearm using the international standard Mantoux intradermal injection method.
Two-step TST
Two-step TST was provided to third (pre-clinical) year medical students. Initial TST with ≥ 10 mm induration was positive for the test. To examine the boosted reaction, a second TST was administered to students with < 10 mm induration at 1–3 weeks later. Booster effect was considered when the second induration was ≥ 10 mm with > 6 mm increase in size.
Serial TST
Medical students with negative two-step TST were eligible for serial TST during the clinical (4th-6th) year training. Conversion was counted when induration was ≥ 10 mm with > 6 mm increase in size from the initial TST.
Records of tuberculin test in medical students performed by the infection control unit from 2001- 2016 were included in the study.
Records without data from the serial tuberculin skin test were not included in the calculation of TST conversion rate.
Electronic records of TSTs provided by the Infection Control Unit of Songklanagarind Hospital were obtained and organized. Figure 1 shows sequences of data in the records. Data from two-step TSTs were summarized and then data from serial TSTs. Finally, conversion rates from serial TSTs were graphically demonstrated in the Joinpoint model.
Analysis
Descriptive analysis
Records on two-step TST from each year were classified into positive, booster and negative results and the percentage of each group was calculated (number of cases in that year divided by number of two-step TST performed in that year). Summarized records on serial TST included the conversion cases. Conversion rate of each test year was calculated as a percentage using number of conversion cases in that year divided by number of follow-up students in that year. Conversion cases were also categorized by generation and year of conversion.
Predictive analysis
Joinpoint model was used to identify change in linear trends of the TST conversion rate. Joinpoint regression program version 4.5.0.1 2017 was the tool.
Ethics
Human Research Ethics Committee, Faculty of Medicine, Prince of Songkla University granted permission for this research (reference number 60-189-09-4). Authors conducted no disclosure of identifiable data.
Two-step TST
There were 2,271 records from two-step TSTs performed in the pre-clinical students (third year medical students) from 2001-2016. Shortage of TST reagents was experienced a few times. Figure 2 shows a summary of the two-step TST results in each test year.
Serial TST
Six hundred and sixty-five medical students underwent a serial TST from 2002-2016. The conversion cases were categorized in Table 1.
Predictive analysis
One Joinpoint model was the best fit for the conversion rates (Figure 3). The annual percent change (APC) in the years 2006-2016 significantly differed from zero (p = 0.013).
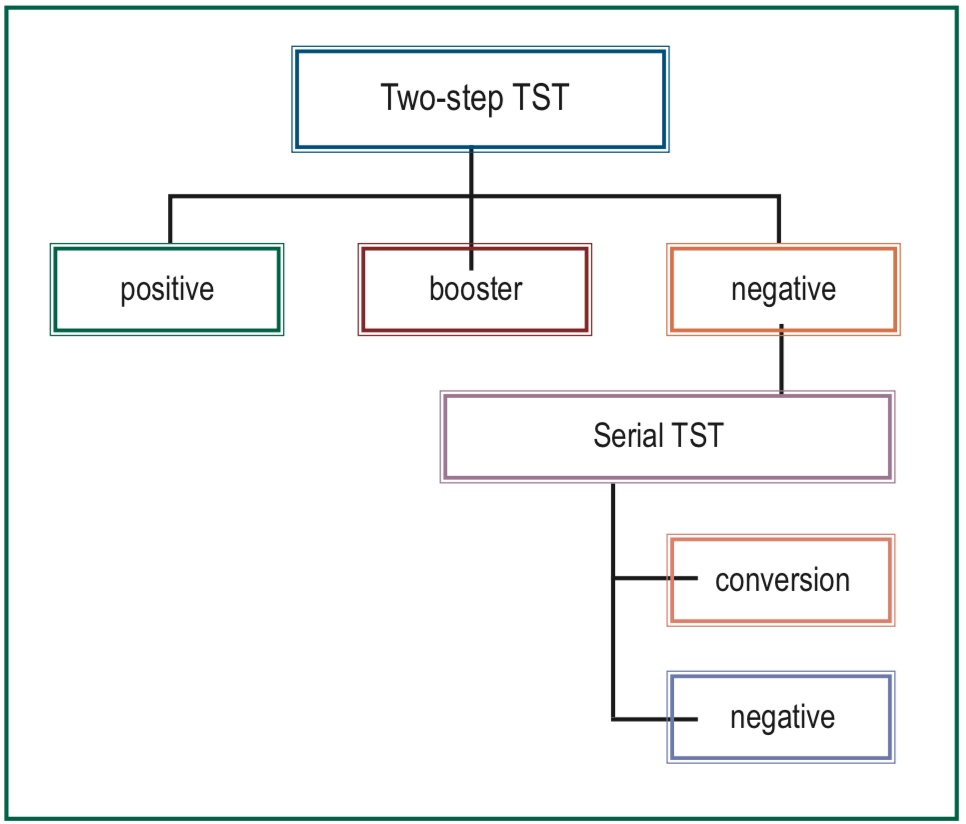
Figure 1: Sequences of data records.

Figure 2: Two-step TST results.
Table 1: TST conversion cases grouped by year of two-step TST performance and time of conversion 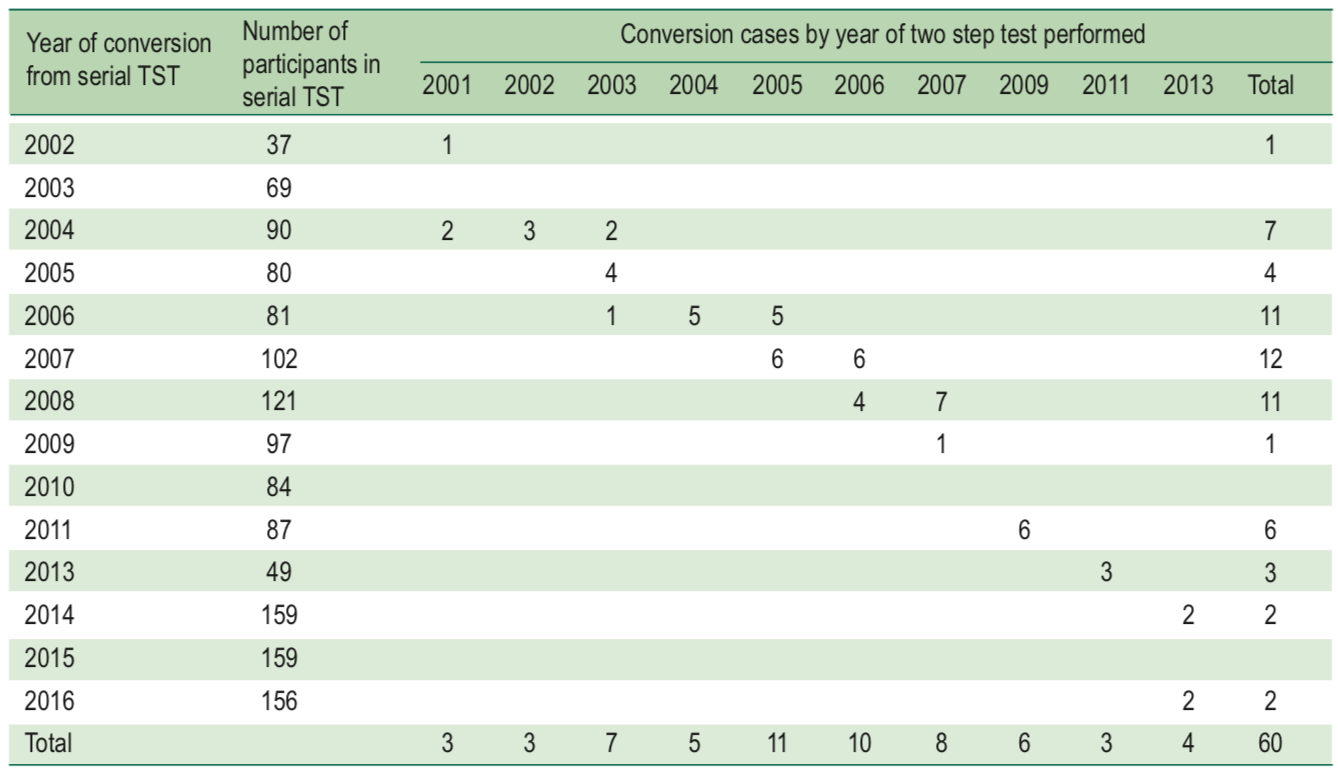
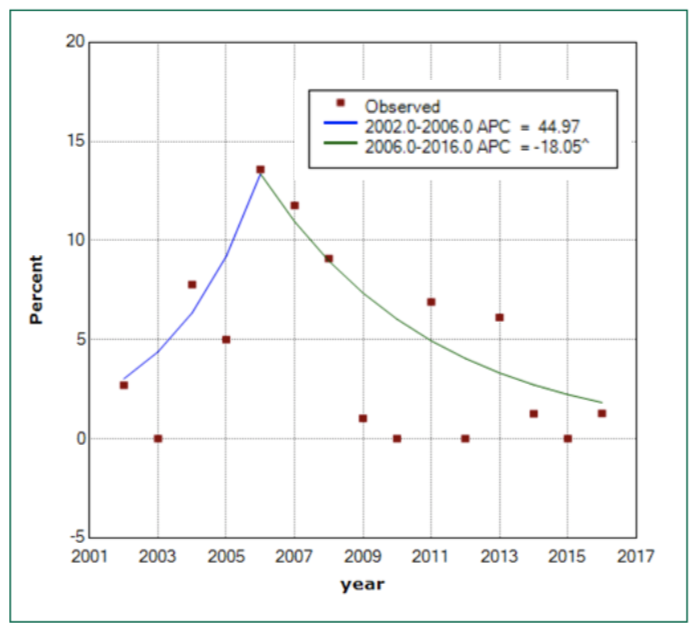
Figure 3: Trend of TST conversion rates in Joinpoint model.
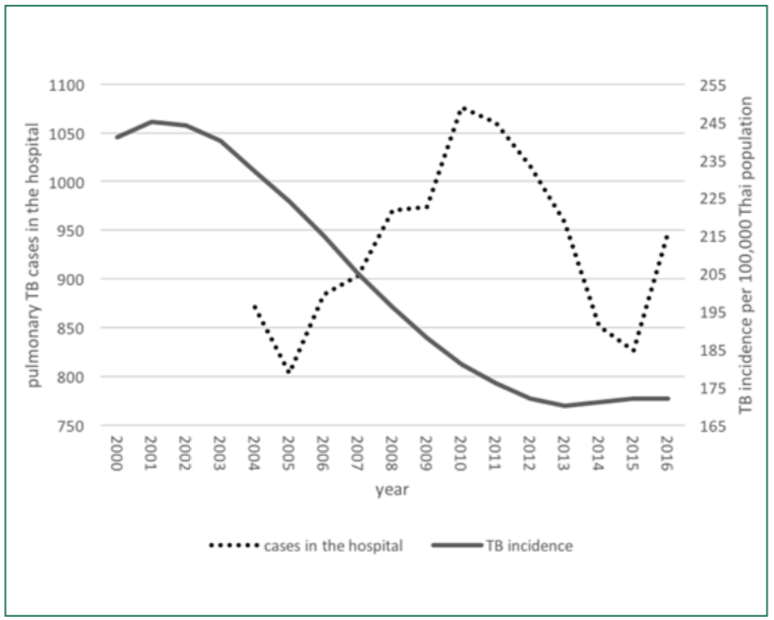
Figure 4: Burden of TB in Thailand and Songklanagarind hospital.
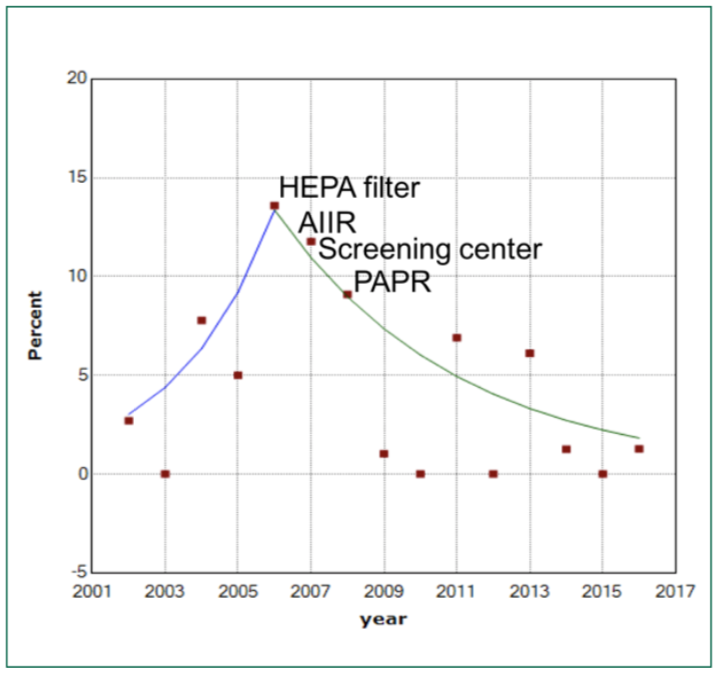
Figure 5: Timeline of major TB control measures introduced at Songklanagarind Hospital.
Among medical students training at Songklanagarind Hospital during the years 2001 – 2016, the incidence of negative two-step TST results was between 40% and 100%.
Only identities, test dates and results were available in the secondary data. No other factors could be obtained for the risk factors. Shortage of reagent supply occurred so no TST was done in 2012 and a small number of two-step TST was done in 2014-2015. For conversion cases in 2013, we have tested an assumption that the conversion happened in 2012 and the peak of Joinpoint trend is also at the year 2006 similar to the Joinpoint model.
To the best of our knowledge, no other study in Thailand has used TST data in medical students longer than 5 years. Albuquerque da Costa, et al.15 showed that TB control implementation in a medical school from 1999 to 2001 had statistically reduced the TST conversion rate with the confirmation of K-M curve analysis. Casas, et al.14 found that TST conversion of health care workers in a Spanish tertiary hospital over 20 years (1988-2007) dropped over time and this reduction may be from TB control measures in the hospital.
While TB incidence in Thailand has been decreasing,16 the number of pulmonary TB patients in Songklanagarind hospital seems to be rising (Figure 5). TB control measures has been implemented by the hospital over time, with administrative and environmental controls, as well as personal protection, in place. Some of those might be relevant over a time line of study as shown in Figure 6. We believe that the hospital investment in modified air ventilation such as open spaces and industrial fans is also outstanding. It can be said that TB con- trol measures play an important role in TST conversion among medical students in Songklanagarind hospital.
We have notice that the percentage of positive two-step TST results has been declining lately. The improvement of the overall TB incidence in Thailand as mentioned above may be one of the contributing factors. Moreover, TST reagent is now regularly ordered and stored by the Pharmacy Department of the hospital. The suppliers of the reagent are the Thai Red Cross and the Tuberculosis Bureau of the Thai Ministry of Health. The Mantoux technique for the administration of TST is employed by our infection control nurses. However, we cannot trace the storage documentation and lot number used for each student after opening the packaging. Therefore, question on the best method for TB infection screening still remain.
Conversion rates of TST among medical students have declined since the year 2006. This corresponds to airborne infection control measures of the hospital at the time.
None declared.
The authors would like to thank the infection control unit, department of family medicine and preventive medicine department of pathology and department of epidemiology for their kind support.