Therapeutic hypothermia is a standard recommended treatment for patients after out-of-hospital cardiac arrest. However, clinical benefits of therapeutic hypothermia for patients with in-hospital cardiac arrest have not yet been approved. The present report aims to demonstrate clinical benefit of therapeutic hypothermia in patients with in-hospital cardiac arrest at the Phyathai 2 Hospital.
We reported two cases of patients who were treated with therapeutic hypothermia after in-hospital cardiac arrest. Surface cooling method with Arctic Sun® system was applied in both cases. Core temperature curve and serial laboratory parameters are reported.
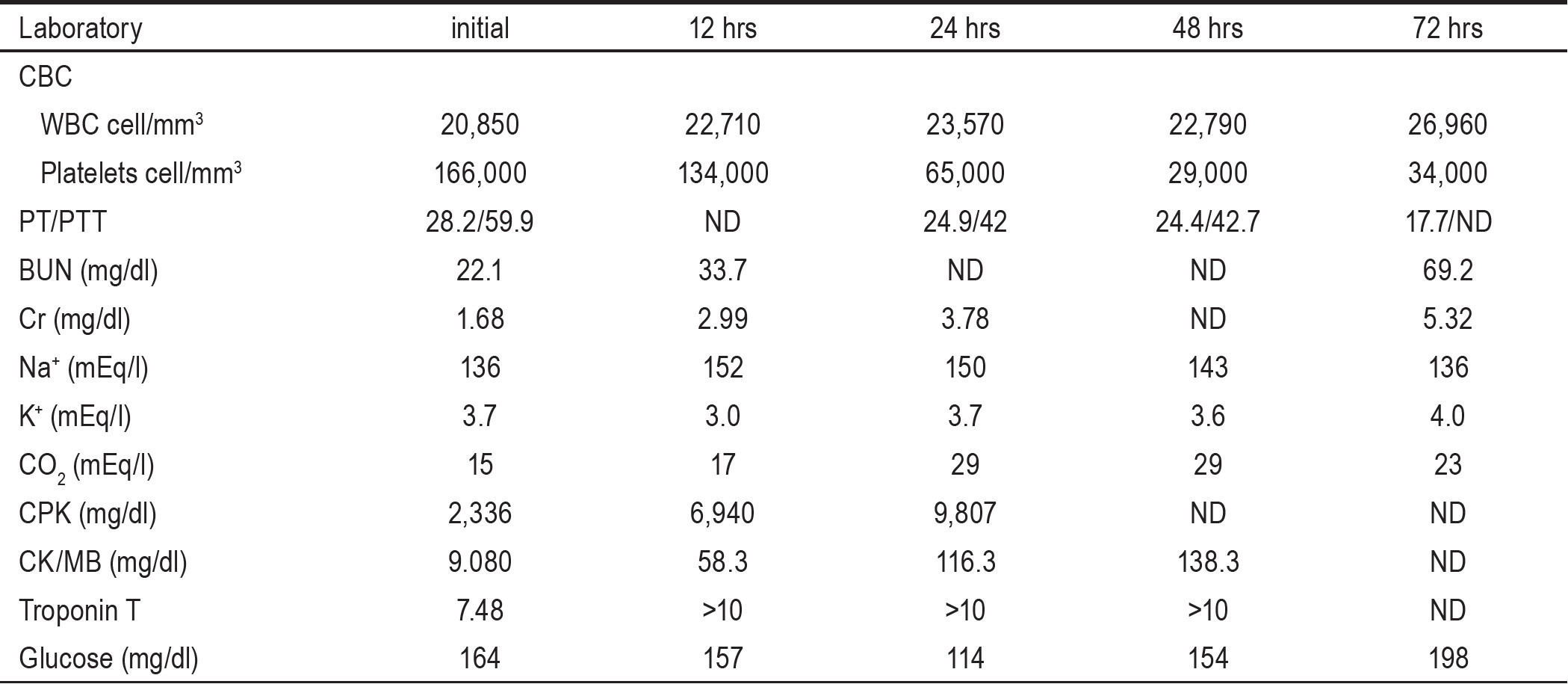
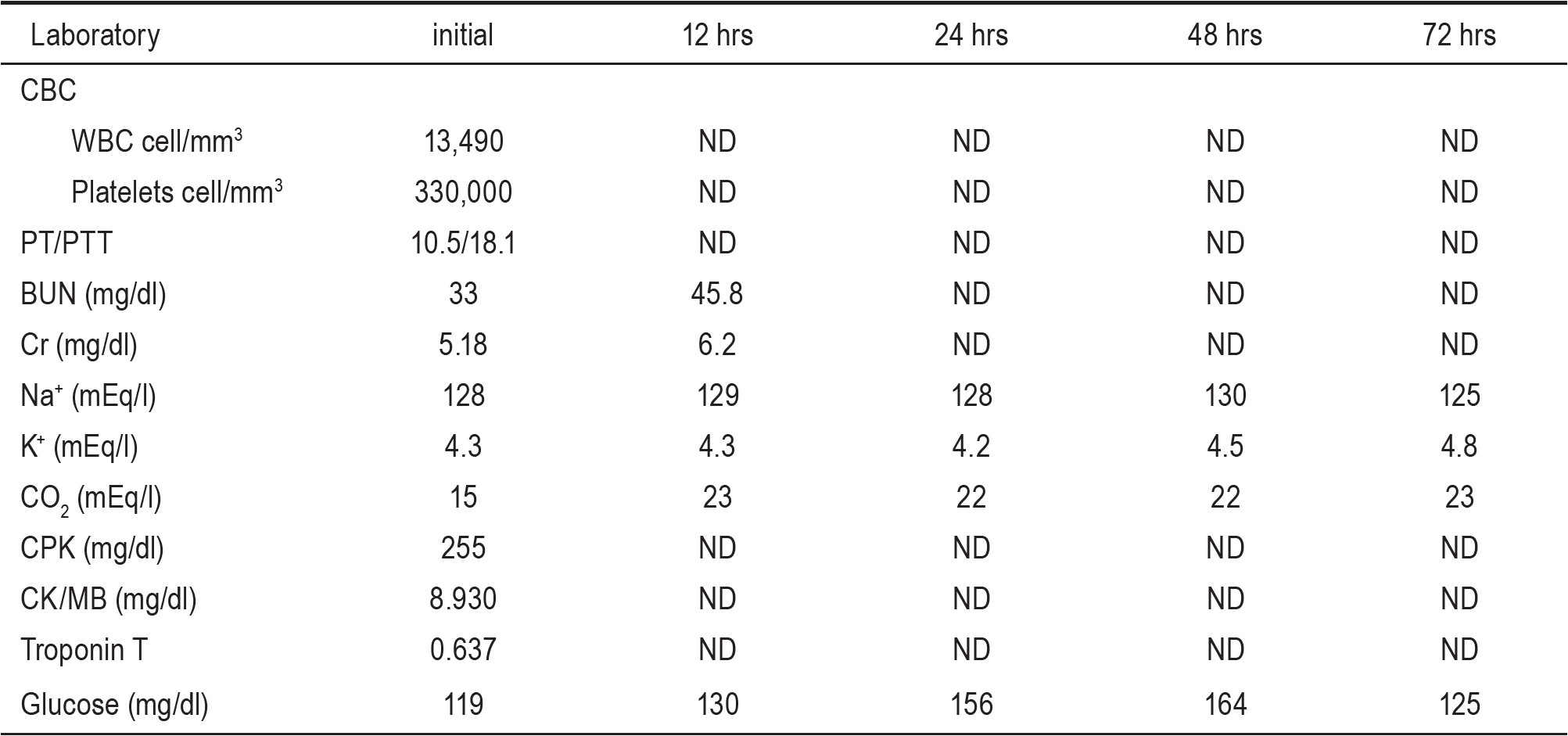
A 65-year-old man with non-insulin-dependent diabetes mellitus (NIDDM), hypertension, dyslipidemia was admitted to the Intensive Care Unit (ICU) because of acute inferior wall type of myocardial infarction with right ventricular infarction. Coronary angiogram showed triple vessels stenosis. Coronary Artery Bypass Graft operation was planned. Unfortunately, cardiac arrest due to ventricular tachycardia developed. After the first successful resuscitation, cardiac arrest due to ventricular tachycardia developed again. However, restoration of spontaneous circulation was achieved after the second resuscitation. He was sent to operating room with Glasgow Coma Scale of E1 VTM1 . Therapeutic hypothermia was started during the operation. The core temperature was 34.8°C when he came back from operating room. Therapeutic hypothermia with surface cooling method by Arctic Sun™ machine was continued. Core temperature was assessed via esophageal route. It took 45 minutes to bring core temperature down to the target of 33°C. Shivering was treated with pethidine and midazolam. The target temperature was sustained for 24 hours. Then, he was re-warmed at rate of 0.2°C per hour until core temperature reached 37°C (as shown in Figure 1). Some clinical parameters are shown in Table 1 and serial basic laboratory data is shown in Table 2.
Post-anoxic myoclonus with electro-clinical seizure was treated with multiple antiepileptic agents. Hemodialysis was initiated during hypothermic procedure for treatment of post-anoxic renal insufficiency. His condition gradually improved including recovery of renal function at 5 weeks of ICU care. He was transferred to a general ward with a tracheostomy tube. One month later, he was alert and able to follow one step commands. After 4 months of hospital rehabilitation program, he regained some motor and cognitive functions. He was able to maintain sitting position on the bed, follow some simple verbal commands, pronounce some words, and swallow pureed food. Finally, he was transferred to another hospital for long term rehabilitation.
Case 1
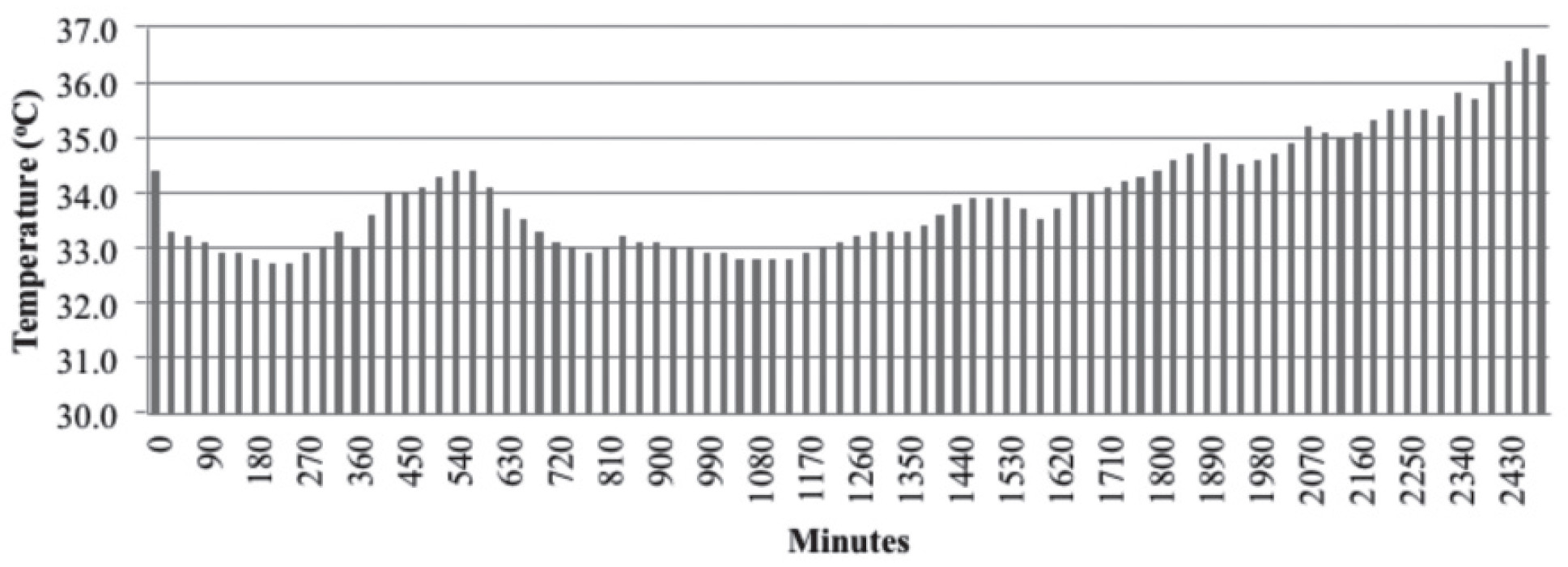
Figure 1: The temperature curve of case 1
Table 1: Baseline parameter of cases
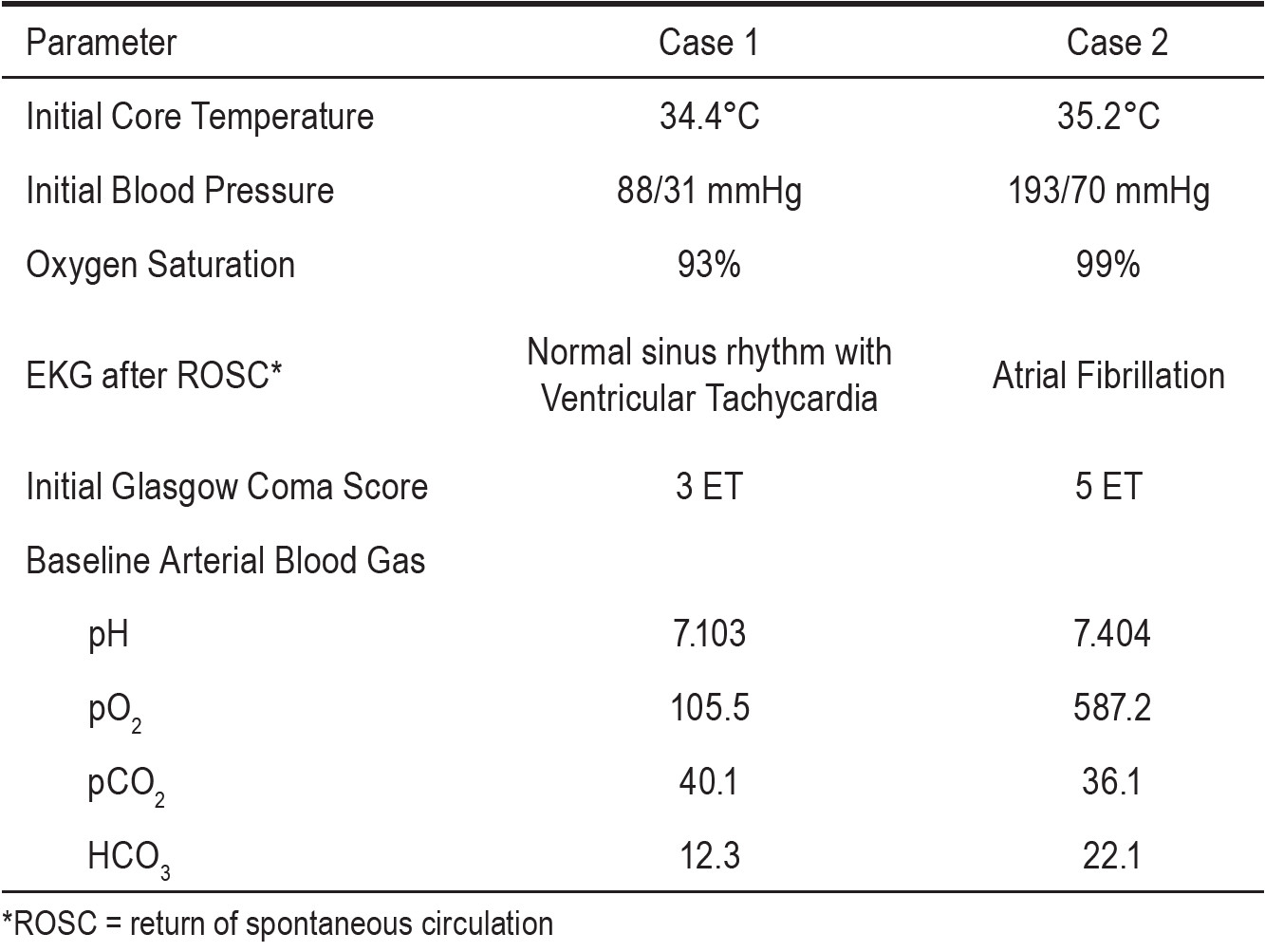
Table 2: Laboratory data of case # 1.
A 66-year-old woman with NIDDM, hypertension, coronary artery disease and chronic kidney disease came in for regular twice-a-week hemodialysis. Cardiac arrest due to ventricular fibrillation developed during dialysis at Dialysis unit. Advanced cardiopulmonary resuscitation (PCR) was started immediately. Restoration of spontaneous circulation was achieved after 20 minutes of CPR. She was sent to ICU and still remained unconsciousness with Glasgow Coma Scale of E1 M4 VT . Arrhythmia was controlled with xylocaine treatment. Therapeutic hypothermia with surface cooling method by Arctic SunTM machine was started. Esophageal temperature probe was placed for core temperature measurement. It took 4 hrs. 30 mins. to bring core temperature down to the target of 33o C. Shivering was found but successfully treated with pethidine and midazolam. The target temperature was sustained for 12 hrs. Then, she was re-warmed at rate of 0.15o C per hour until core temperature reached 37o C (as shown in Figure 2). Some clinical parameters are shown in Table 1 and serial basic laboratory data is shown in Table 3. Sedative drugs were gradually tapered down during re-warming phase. The patient regained consciousness and Glasgow coma score was raised to 10T (E4 M6 VT) after re-warming. She was extubated 5 days later after AICD implantation. Her motor and cognitive function fully recovered. She was discharged from hospital one week later. Currently, she continues to come in regularly for hemodialysis.
Case 2
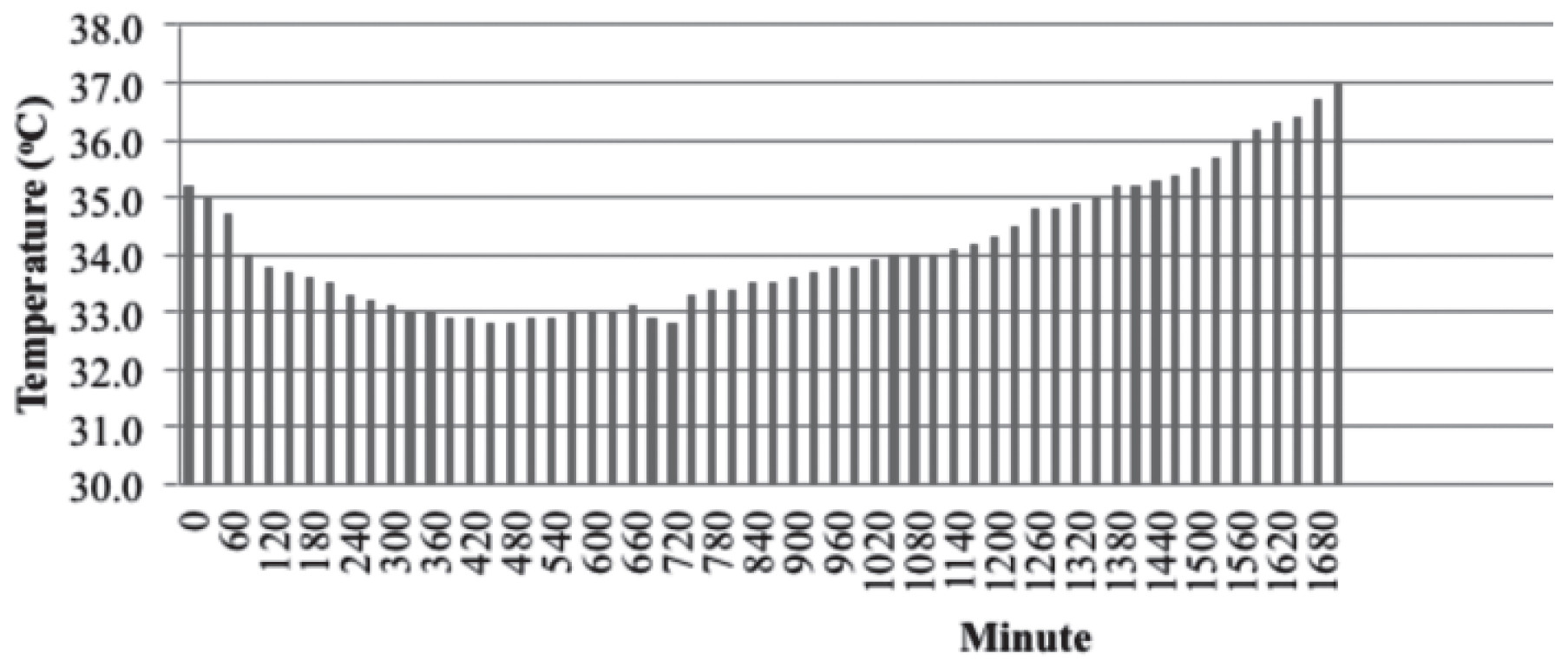
Figure 2: The temperature curve of case 2
Table 3: Laboratory data of case # 2.
Therapeutic hypothermia after cardiac arrest has been the Class 1 recommendation by International Liaison Committee on Resuscitation since 2003.1 In October 2010, the American Heart Association announced the class 1 recommendation for therapeutic hypothermia after cardiac arrest in part 9 of the guidelines for cardiopulmonary resuscitation and emergency cardiovascular care.2 The evidence of clinical benefit of therapeutic hypothermia after cardiac arrest derived from two major studies from Europe and Australia.3, 4 From pooled data analysis of therapeutic hypothermia in out-of-hospital cardiac arrest, one in six patients are helped by having neurological intact survival (number-needed-to-treat [NNT] = 6).5 Therapeutic hypothermia after cardiac arrest has been successfully implemented in many countries, including some countries in Asia.6-8 It is also however true to say that there is some controversy over the clinical benefits.8-9 One retrospective study reported no neurological benefit of therapeutic hypothermia in non-shockable patients with in-hospital cardiac arrest.10 As yet, therapeutic hypothermia after cardiac arrest is not well established in Thailand.
Several methods of therapeutic hypothermia have been tested. Surface and Endovascular Cooling methods are reliable. These two methods are the most commonly used for therapeutic hypothermia. Surface cooling is less invasive than endovascular method. Surface cooling provides an acceptable hypothermic efficacy. For these reasons, surface cooling is most commonly as the initial method for therapeutic hypothermia after cardiac arrest.11 However, multimodality methods may be necessary to facilitate achievement of temperature target.12 Shivering is the last resort defense mechanism to prevent hypothermia. To bring the core temperature down to target, shivering needs to be effectively defeated.13 Pethidine or Meperidine raises shivering threshold. Pethidine is commonly available worldwide, therefore, is generally used to reduce shivering.14 Therapeutic hypothermia has not yet been approved as a standard treatment of in-hospital post-cardiac arrest patients. Our initial experience of therapeutic hypothermia after in-hospital cardiac arrest with surface cooling method implies feasibility of its use in clinical practice and clinical benefits are also demonstrated in our patients. However, further clinical study is needed to confirm its clinical benefit in worldwide patients with in-hospital cardiac arrest.
Therapeutic hypothermia after cardiac arrest has been the Class 1 recommendation by International Liaison Committee on Resuscitation since 2003.1 In October 2010, the American Heart Association announced the class 1 recommendation for therapeutic hypothermia after cardiac arrest in part 9 of the guidelines for cardiopulmonary resuscitation and emergency cardiovascular care.2 The evidence of clinical benefit of therapeutic hypothermia after cardiac arrest derived from two major studies from Europe and Australia.3, 4 From pooled data analysis of therapeutic hypothermia in out-of-hospital cardiac arrest, one in six patients are helped by having neurological intact survival (number-needed-to-treat [NNT] = 6).5 Therapeutic hypothermia after cardiac arrest has been successfully implemented in many countries, including some countries in Asia.6-8 It is also however true to say that there is some controversy over the clinical benefits.8-9 One retrospective study reported no neurological benefit of therapeutic hypothermia in non-shockable patients with in-hospital cardiac arrest.10 As yet, therapeutic hypothermia after cardiac arrest is not well established in Thailand.
Several methods of therapeutic hypothermia have been tested. Surface and Endovascular Cooling methods are reliable. These two methods are the most commonly used for therapeutic hypothermia. Surface cooling is less invasive than endovascular method. Surface cooling provides an acceptable hypothermic efficacy. For these reasons, surface cooling is most commonly as the initial method for therapeutic hypothermia after cardiac arrest.11 However, multimodality methods may be necessary to facilitate achievement of temperature target.12 Shivering is the last resort defense mechanism to prevent hypothermia. To bring the core temperature down to target, shivering needs to be effectively defeated.13 Pethidine or Meperidine raises shivering threshold. Pethidine is commonly available worldwide, therefore, is generally used to reduce shivering.14 Therapeutic hypothermia has not yet been approved as a standard treatment of in-hospital post-cardiac arrest patients. Our initial experience of therapeutic hypothermia after in-hospital cardiac arrest with surface cooling method implies feasibility of its use in clinical practice and clinical benefits are also demonstrated in our patients. However, further clinical study is needed to confirm its clinical benefit in worldwide patients with in-hospital cardiac arrest.
This initial experience of therapeutic hypothermia after in-hospital cardiac arrest with surface cooling method possibly implies clinical benefit and feasibility of its use in clinical practice.