Nowadays,the 64 slice MDCT has become a reliable, standard tool for diagnosing coronary stenosis in mild to moderate risk patients. The overall reported sensitivity and specificity were reasonably accepted.4,5 However, several limitations of the 64 MDCT existed, which included a long acquisition time, and the often required administration of beta-blockades to lower the motion artifacts from patients with high heart rates. With the new 256 MDCT, more data was collected within a shorter time, patients received reduced doses of radiation and the image quality was also much improved.
To verify the diagnostic accuracy of this new scanner in daily practice, we decided to perform the comparative study between the 256 MDCT and the standard ICA.
From January-December 2009, a total of 1,707 patients, (regardless of having any cardiac arrhythmia including atrial fibrillation), had undergone coronary artery scanning by the 256 MDCT. Exclusion criteria included acute myocardial infarction, patients at risk for iodinated contrast agents, or elevated serum creatinine >1.5 mg/dl. Among those,147patients were requested to do an additional ICA by their cardiologists owing to indecisive degree of stenosis and/or divergent clinical presentations.
To verify the diagnostic accuracy of this new machine, we retrospectively compared the coronary images from the 256 MDCT with those from the standard ICA. All epicardial arteries were segmented according to the guidelines developed by the BARI investigators.1,2 Significant coronary stenosis was defined as the reduction of luminal diameter ≥ 50% in comparison with an adjacent angiographically normal segment.1,2 The degree of coronary stenosis was classified by severity of luminal reduction; mild (reduction of luminal diameter <50%), moderate (reduction of luminal diameter 50-69%) and severe (reduction of luminal diameter ≤70%). This study was approved by our institutional ethics committee and all participants gave their written informed consent.
CT coronary angiography (CTA)
CT studies were performed on 256 MDCT (Brilliance ICT 256 MDCT, Philips, Netherlands) scanner with a 0.27s rotation time. A bolus of iodinated contrast injection volume was calculated by the formula of scan time (5 sec. for coronary artery scanning) plus post threshold delayed time (~5 sec.) and multiplied by flow rate (4.5-6 ml./sec.) (Phillips company protocol). A contrast bolus was injected into brachial vein at a flow rate of 4.5-6 ml./sec. (Flow rate 6 ml./sec. of contrast injection was preferred if the patient’s body weight >90 kg), followed by 50 ml. saline solution injection. The tracking position was placed at the ascending aorta and scan started automati- cally at 5.0 sec. after reaching the threshold (100-120 Hounsfield units, HU). Cardiac scan length covered from the tracheal bifurcation to 2-3 cm. below the diaphragm using the following parameters; X-Ray tube potential 120-140 KV, tube current 471 MA, slice collimation 128x0.625 mm2, table speed of 44 mm/sec.,and pitch 0.16. The mean coronary scan time was 5.0 sec. The retrospective electrocardiographic gating was routinely used for cardiac phase selection. The coronary scan data was completely obtained from two to three consecutive heart beats, the axial slices were recostructed and synchronized to the ECG. If the heart rate remained above 70 beats per minute, beta-blockade might have been administered if there were no contraindications.
The slice thickness was of 0.67 mm. The CT data was independently and blindly analyzed by three experienced cardiac CT specialists. The vessel analysis was assessed on at least two planes, one parallel and one perpendicular to the course of the vessel.
Invasive coronary angiography (ICA)
ICA was performed by standard technique via femoral approach. At least two orthogonal views were taken for each of the epicardial arteries. The angiograms were separately analyzed by experienced interventionists who had not done a prior review of the MDCT images. ICA was performed after cardiac CT scan if the results of cardiac scan showed significant coronary artery stenosis or showed controversial results relative to the patient’s clinical signs. The coronary arteries (LMA, LAD, LCX, RCA) were segmental located (proximal, mid, distal) according to the guidelines as mentioned above.1,2 The coronary segment was considered for significant stenosis by the same criteria as used in CT.Coronary artery dominance refers to the artery that supplies the posterior descending artery (PDA). Coronary artery lesions were described by their locations (proximal, mid and distal) and classified according to severity. Severity of coronary artery stenosis was estimated with percentage of stenosis defined as the ratio of reference luminal diameter divided by the reference diameter vessel measurement.1
Statistical analysis
By using ICA as the gold standard, images from CTA and ICA were compared and analyzed. The sensitivity, specificity and accuracy including positive andnegative predictive values were calculated.Chi-square test was used to an lyze observed differences, and p statistically significant difference.
Of total 147 consecutive cases, 80% were men (124 male, 23 female) and the mean age was 60 ±12 years. Of total 588 coronary arteries, all 1470 coronary segments (147 segments of LMA, 441 segments of the LAD, 441 segments of the LCx, 441 segments of the RCA) were studied.
By ICA, as shown in Table 1, 73.2% (1076/1470) were angiographically normal, 18.9% (278/1470) had significant stenosis (luminal stenosis ≥50%) and the remaining 7.9% (116/1470) had non significant lesions.
By CTA, 98.9% (1455/1470) coronary segments were eligible for analysis. Only 1.1% (15/1470) of coronary segments were ineligible due to unusually high calcium clumps (n=13) and motion artifacts (n=2). Calcium scoring was calculated and the severity level was classified using Agaston system criteria.
Table 1: Distribution of coronary artery stenosis evaluation result using the gold standard ICA
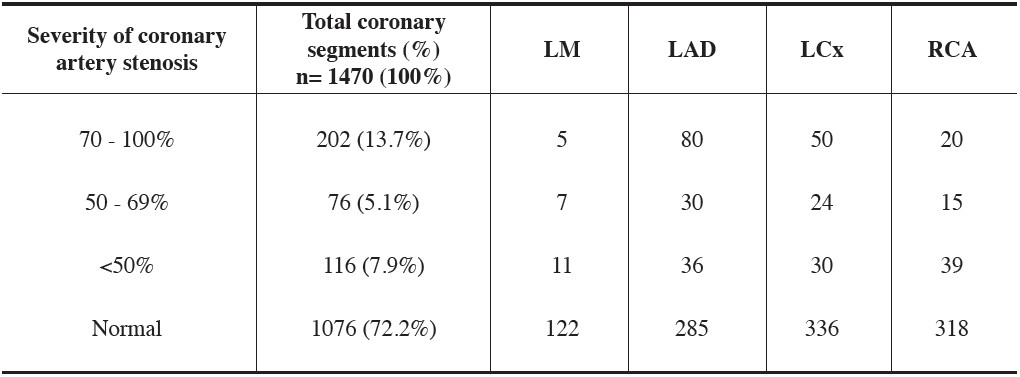
Table 2: Correlative findings of coronary artery stenosis between the CTA and ICA
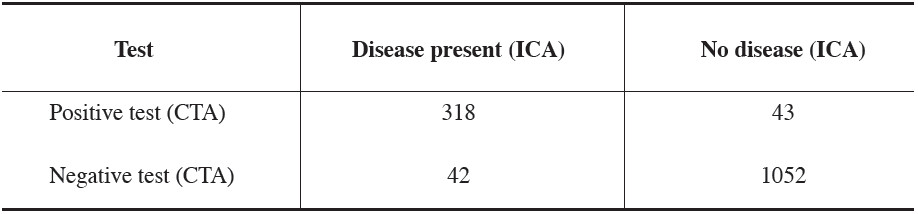
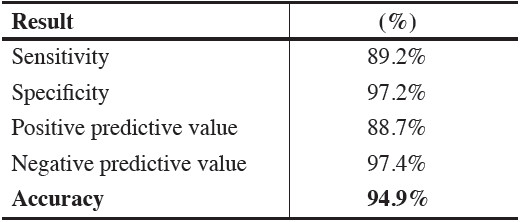
Table 3: Overall diagnostic accuracy of the 256 MDCT in diagnosing coronary artery stenosis comparing to the gold standard ICA
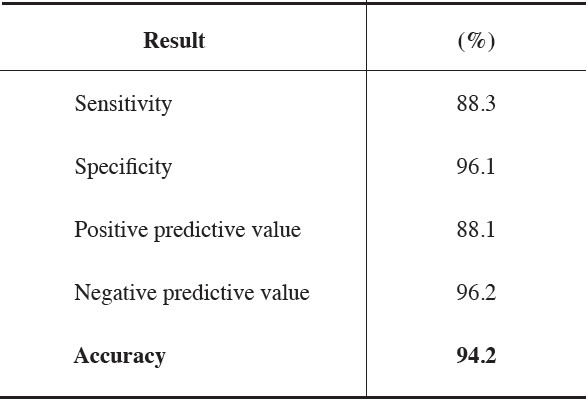
Table 4.1: Correlative findings of coronary stenosis between the CTA and ICA in massive calcium score (CAC>400 U) subgroups
Table 4.2: Diagnostic accuracy of the 256 MDCT in diagnosing significant coronary artery stenosis comparing to the gold standard ICA in subgroup with massive calcium score (>400)
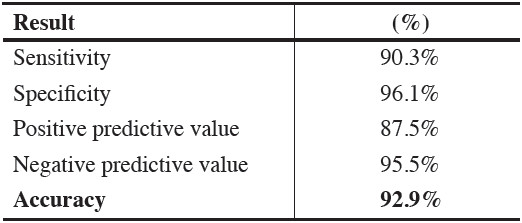
Table 5.1: Correlative findings of coronary stenosis between the CTA and ICA in non massive calcium score (CAC

Table 5.2: Diagnostic accuracy of the 256 MDCT in diagnosing coronary arterystenosis comparing to the gold standard ICA in subgroup with non massivecalcium score (<400)
61 patients (41.2%) had calcium scoring >400 U Table 2 & 3 show correlative findings between ICA and CTA. Of a total 1455 segments, the agreement between ICA and CTA were 72.3% (1052/1455) for non-stenotic lesions and 21.2% (318/1455) for non significant and significant lesions. The discordant readings were 2.9% (43/1455) that appeared to have significant stenosis by CT only and 2.8% (42/1455) by ICA only.
Table 4.1 and 5.1 below delineated the correlative findings of coronary stenosis between ICA as a gold standard and CTA in massive calcium score (CAC >400 U) and non massive calcium score (CAC
The overall sensitivity of the 256 MDCT in detecting coronary artery stenosis was 88.3%, specificity was 96.1%, the positive predictive value of MDCT was 88.1% and the negative predictive value was 96.2% and the overall accuracy was 94.2% (p-value = 0.20) (Table 2-3). In massive calcium scoring cases (calcium scoring >400 U) sensitivity for detecting coronary artery stenosis was 90.3%, specificity was 96.1%. The positive and negative predictive values were 87.5% and 95.5% respectively with the overall accuracy of 92.9% (Table 4.2).
In non massive calcium scoring cases (calcium scoring <400 U)sensitivity and specificity were 89.2% and 97.2%respectively. The positive predictive value was 88.7% and the negative predictive value was 97.7% and the overall accuracy was 97.4% (Table 5.2). For CTA, 13 segments of 610 segments (2.1%) of massive calcium scoring (CAC >400) and 2 segments of 860 segments (0.002%) of non massive calcium scoring (CAC <400) subgroups were not be able to evaluate the degree of stenosis, owing to the blooming artifacts from severe calcification and motion artifacts respectively. The diagnostic accuracy of these two subgroups were not significant different (p=0.30). The total volume of iodinated contrast use was 60 ±10 ml for coronary artery scanning. The minimum and maximum value of calcium scoring were of 0 and 3506 U respectively (mean =275.5). Only 10 patients (0.007%) with a heart rate of more than 80 beats per minute were considered to be given beta blocker drugs before CT scanning.
Currently, MDCT offers analternative way to evaluate coronary artery stenosis without the risks of an invasive procedure. The overall diagnostic accuracy of the standard 64 MDCT ranged from 94-95% of sensitivity, from 67-97% of specificity and the positive and negative predictive values were 78-87% and 92-97% respectively.4,5 However, several limitations existed including amount of contrast used, radiation exposure and motion artifacts from high heart rate.
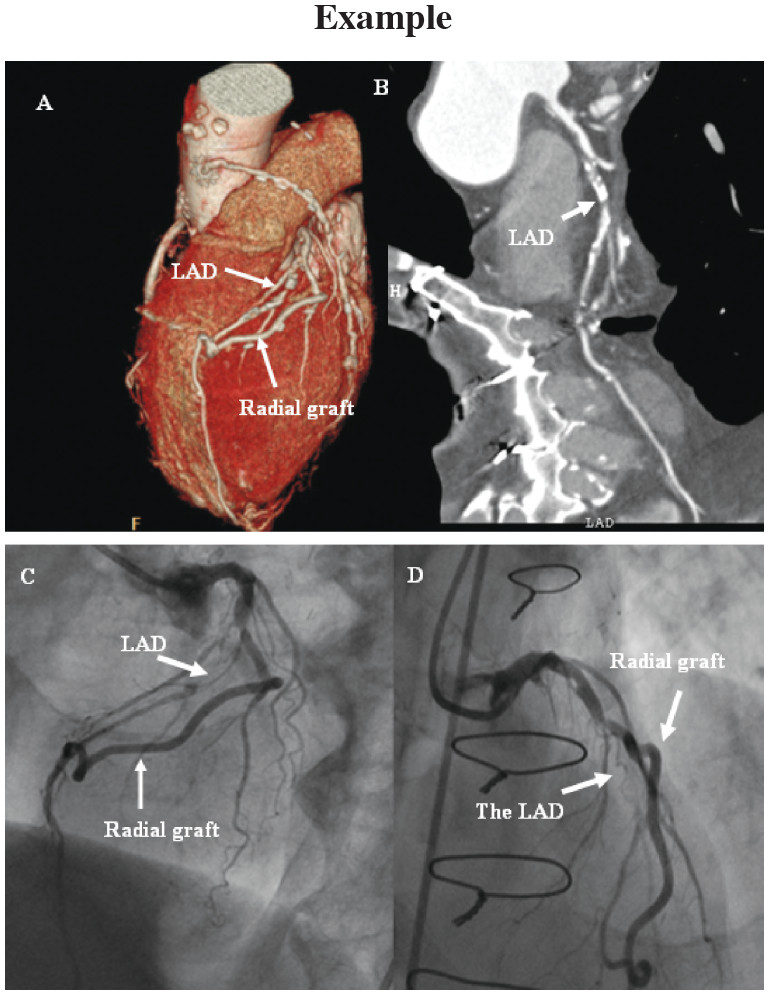
Figure 1: The images of 256 MDCT coronary angiography and ICA of a 78 year old man with history of coronary bypass graft, who came to the hospital with chest pain. The CT scan showed the total calcium volume to be more than 400 (539.8).
By increasing number of detectors, the 256 MDCT could obtain sufficient data faster (within 2-3 heart beats) and was able to examine patients with higher heart rate without requiring them to take beta-blockade medicine. Bycuttingdownthescantime,theaveragepatienteffective radiation dose equivalent was reduced from 15-21 mSV in 64 MDCT scanner6,7 to around4-17 mSV (20-30% reduction) for coronary artery scanning and the iodinated contrast volume decreased by 30%.(We compared the radiation doses and contrast volumes with our initial experiences in the previous two years using 64 MDCT). However, the further investigation for clinical application in real world is still needed.
In daily practice, high risk cases of coronary artery disease (CAD) would go for invasive coronary angi- ography and only borderline or non high risk patients would be referred for CTA. In our study, total of 147 non high risk patients with clinically suspicious CAD were referred for CTA but their cardiologists still requested ICA owing to the positive or undetermined CTA results. By ICA, 80% of angiogram showed either normal or non-significant stenosis suggested the low risk popula- tion. By using ICA as a gold standard, the sensitivity of 256 MDCT was 88.3% and the positive predictive value was 88.1% which were acceptable compared to the ICA. In addition, the high specificity of 256 MDCT, 97.5% made this machine very reliable for exclusion of CAD in low risk subgroups.
Blooming artifact effects remained a major limitation of CTA owing to massive calcium deposits. Our study showed non significant differences in the diagnostic accuracy between the massive calcium scoring (CAC >400) and non massive (CAC <400) calcium subgroups (92.9% and 94.9%, p=0.30). It indicates that high total calcium score seems not to have much effect on coronary artery assessment. However, the personal experiences of the reader might need to be taken into account. In addition, the negative predictive values of these two groups were impressive as 95.5% and 97.4% and could be use for exclusion of CAD in low risk candidates.
Finally, it is not only the non high risk patients who benefit from the new scanner. To verify graft patency in high risk patients who have undergone bypass surgery is another valid application. Without angle limitation, the patency and quality of graft especially at anastomotic site is well appreciated as delineated in Figure 1.
Study limitation
In addition to the relatively small number of subjects, our study represented the correlative findings between CTA and ICA of major epicardial arteries in only non high risk CAD suspicious patients which we believed would be the majority of CTA cases in daily practice. Unfortunately, we also do not have the long-term follow up with all patients. The future clinical outcome is of interest especially in the cases with nonsignificant lesion which could be subjected to acute plaque rupture.
The 256 MDCT offers a reasonably high diagnostic accuracy in detecting coronary artery stenosis in non high risk patients with clinically suspicious CAD. The shorter scan time of the 256 MDCT also benefits the patient who has contraindication to beta blocking drugs. High negative predictive values (regardless of calcium score) mean that the 256 MDCT could be confidently used for exclusion of CAD in low risk candidates.