The National Health Security Office (NHSO) of Thailand expects public hospitals to co-operate in implementing health behavior modifications in their patients, in order to reduce or prevent health problems, with a particular focus on metabolic disease, especially obesity. Since 1991, there has been a dramatic increase in obesity in Thailand. Data from 1991, 1996 and 2004, indicates that obesity in Thai people has increased from 20% to 25% and 34% respectively. There were 13 million obese people and 12 million overweight people in 2004.1 A survey in 2008-2009 showed the high correlation between increasing obesity and the risk factor for diabetes, high blood pressure, cardiovascular diseases and cancer in the Thai population.1
Programs to reduce health problems due to obesity have been set up in many hospitals with different approaches. The researcher, as a Head nurse who was in charge of the Health Promotion and Disease Prevention program of Lerd-Sin Hospital, considered that nurses play a crucial role in implementing health behavior changes at the practical level among the general public, since nurses are responsible for educating patients about self care management.2-6 She decided to put into effect a “Weight and Disease reduction program”, which would use the PROMISe model to encourage the “3 self” health behavior modifications (Self-efficacy, Self-regulation and Self-care) concentrated in 3 Topics, Diet, Exercise, and Emotion.
Starting in 2007, staff of the Hospital who were obese or staff who had a Body Mass Index (BMI) value greater than 25, participated in the Weight and Disease Reduction Program. The result of the program showed that 77.77 % of the participants were able to change their behaviors and reduce their weight after finishing the program. In 2009, the program expanded beyond the hospital to include the general public. In 2010, the participants of the program included overweight people or those with a BMI value greater than 23.8 There were 302 overweight participants who completed the program activities of training and practicing food control. Five days of food prepared by the hospital dieticians was part of the program. Total daily energy intake was 1,000 kilocalories. Ninety-three percent of the participants lost weight after five days of food controlled-intake. Two to three months after the program, the percentage of participants who were still losing weight dropped to 76.8%, although the participants had a better understanding about 3-Self health behavior changes and 80.5% of the patients reported satisfaction with the program.
Findings from the previous study showed that the improvement in health behavior change score and a high reported satisfaction with the program did not explain the sustainability of the health behavior changes. There appeared to be other factors that were responsible for the sustainability of the change. Therefore, the researcher decided to conduct a study into the relationship between the factors in PROMISe model and the sustainability of the 3-Self health behavior changes, concentrating on the 3 areas which affected weight reduction of the participants in their normal daily lives. The findings from this study would improve future program activities in order to create more sustainable 3-Self health behavior changes.
The objectives of this research were threefold. To study the PROMISe model in 3-Self Health behavior change concentrating on 3 areas in Weight and Disease Reduction program. Also to identify the sustainability of the health behaviors change both after the program had ended and 6 months later using the reduction of Body Mass Index (BMI) value as an indicator. Lastly, to study the relationship between 6 factors in PROMISe model to 3-Self health behavior change in 3 areas.
Research Method
This was a cross-sectional study.
Population
The population in this study was the participants in “Weight and Disease Reduction Program” in 2010, members of the general public who were divided into two groups. The first group included every participant in the program, which were 302 people. The second group was made up of the participants who either attended the focus group meeting or returned the completed management survey to the Health Promotion and Disease Prevention Department. The focus group meeting and management survey was set up 6 months after participants had finished the program. The second group numbered 173 people, of which 70% had been able to lose weight and 30% had not. The weight loss ratio of the members of the second group corresponded to the ratio of all program participants, those who could and those who were unable to lose weight, at the end of the program.
Data Collection
Data used in this research was collected in 2 phases. The first phase included data collected before the program started and at the end of the Weight and Disease Reduction Program for the general public in 2010: data was collected from all 302 program participants. Tools used were the Metabolic Risk Screening Form from NHSO, and participants’ self evaluation of their 3-self health behavior changes during the program, using the form developed by Ungsinun Intarakamheng.7 Participants provided their daily calorie intake, exercise record, weight change and so on. They also had to report on the effectiveness of program activities (which had been designed to relate to the PROMISe model’s 6 factors).
Developed by the researcher, tools used in the second phase were divided into 4: physical examination report, a questionnaire related to 3-Self health behavior changes in 3 areas (continuation of self evaluation as described in Phase 1) a questionnaire related to the current practice of behaviors which increase obesity risk, such as number of meals per meal, or eating between meals, (this was to see whether participants could apply the knowledge they had received during the program) and a questionnaire which asked questions designed to assess the influence of each of the 6 factors of the PROMISe model on health behavior changes. The researcher used validity and reliability assessments in order to test and improve the tools in the second phase. Two management specialists and 5 participants from the previous program in 2008-2009 analyzed the content validity. The confidence interval of the Cronbach’s alpha coefficient of the reliability test of 30 participants from the previous program in 2008-2009 was 0.89.
Data Analysis
The study used descriptive statistics such as frequency, percentage, mean, standard deviation for general data analysis. We used Chi-square and Pearson correlation coefficients to describe the relationship between 3-self health behavior changes, weight reduction, the 6 factors of PROMISe model and participants’ satisfaction with the program. Finally we used t-test and paired t-test to compare the differences between the health behavior changes and changes in BMI.
1. General Data Analysis showed that 83.4 % of the participants were females aged between 40 to 60 years old. Participants with an education level above or below bachelor degree were 49.3% and 50.7% respectively. About, 34.8% of the participants were housewives. Of those, 45.7% had health insurance and 44.7% had social security coverage, 13.9% of participants were civil servants or state enterprise employees. Most (67.9%) participants had immediate family members with metabolic disease. Forty-five percent of the participants were already sick or at risk of becoming being sick. Those with metabolic diseases (72.1%) which 38.1% of them suffered from high blood pressure, diabetes, gout, and brain infarction. Only 38.1% of participants who had metabolic disease took good care of themselves, or effectively controlled their disease. Participants who had a BMI value between 25 and 29.9 (61.3%) had high blood pressure and were at risk of developing metabolic disease.
2. The differences between the average 3-Self health behavior change, BMI value, and participants’ satisfaction before and after finishing the program were shown in Table 1. The average of 3-Self health behavior change significantly increased in all areas (Mean > 2.5), while there was a significant average decrease in BMI values, from 29.28 to 28.39. The average of the satisfaction with the program was 3.13.
3. The sustainability of 3-Self health behavior changes (which affected both BMI value and satisfaction) at the conclusion of the program and 6 months after the program was shown in Table 2. If we compared from beforethe program started (Table 1), to program completion and then 6 months after, the average of 3-Self health behavior changes for 173 participants still increased in all areas. The average BMI value continued to decrease from 28.10 at program end to 27.97. The average program satisfaction increased from 3.13 to 3.28. However, the average of 3-Self health behavior changes in 3 areas, between those participants who could and those who could not lose weight at the end of the program and 6 months after the program showed a significant difference for Self-efficacy and Self-Care at 0.05 confidence level and was illustrated in Table 3.
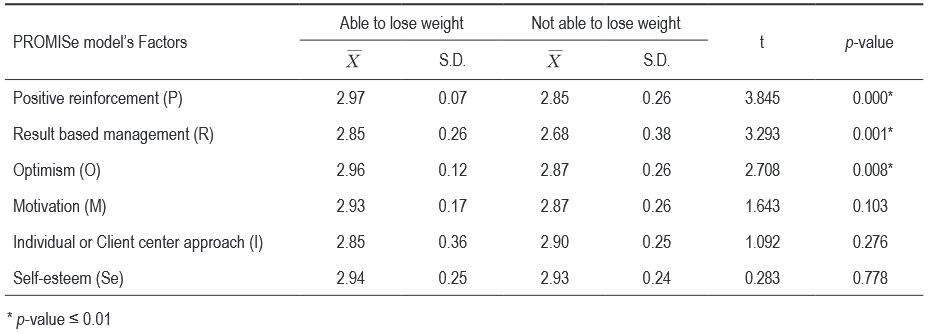
4. The statistical relationship between the 6 factors of the PROMISe model and the sustainability of the 3-Self health behavior change in 3 areas, BMI value, and satisfaction with the program 6 months after the program, showed all 173 participants agreed that using PROMISe Model to conduct weight loss program activities affected 3-Self health behavior change in 3 areas. The average of all factors was 2.88. The average of 6 factors of the PROMISe Model, which were Positive reinforcement (P), Result based management (R), Optimism (O), Motivation (M), Individual or Client centered approach (I) and Self-esteem (Se), equaled to 2.91, 2.77, 2.92, 2.90, 2.87 and 2.93 respectively. The relationship among 6 factors of PROMISe Model to 3-Self health behavior change and program’s satisfaction showed that Positive reinforcement was related to Self-regulation, Result based management was significantly related to Self-efficacy and Motivation significantly related to Self-regulation at 0.01 confidence level, as illustrated in Table 4.
The relationship between the 6 factors of PROMISe model, health behavior changes in 3 areas and weight reduction showed that Positive reinforcement, Result based management, and Optimism was significantly related to the sustainability of health behavior change in 3 areas and weight reduction at 0.05 confidence level as illustrated in Table 5 and Table 6.
5. The summary of the focus group meeting demonstrated the reasons that contributed to health behavior changes. The recommendations coming out of this session would lead to future program improvements. The purpose of the focus group meeting was to evaluate and review the effects of the health behavior changes during the program on daily life. The focus group discussions helped the participants to identify which factors led to sustainability in health behavior changes or what prevented changes. During the session, the participants shared their self control experiences in 3-Self health behavior change, answered the questionnaire about the activities management of the program using PROMISe model and then gave some suggestions of how the program could be improved in future.
5.1 The participants who either maintained the healthy behavioral changes or lost weight stated that their ability to apply their new knowledge in their daily lives, (for example, controlling their eating behaviors, regularly selecting food according to their individual daily energy needs or making changes during social events, improved emotional control, mind training, self control with regards to weight monitoring etc.) were what caused their health behavior changes to be sustainable.
Table 1: The differences in the averages of the 3-Self health behaviors, Body Mass Index (BMI) value and satisfaction (SAT) with the program, before and after the program. (n = 302)
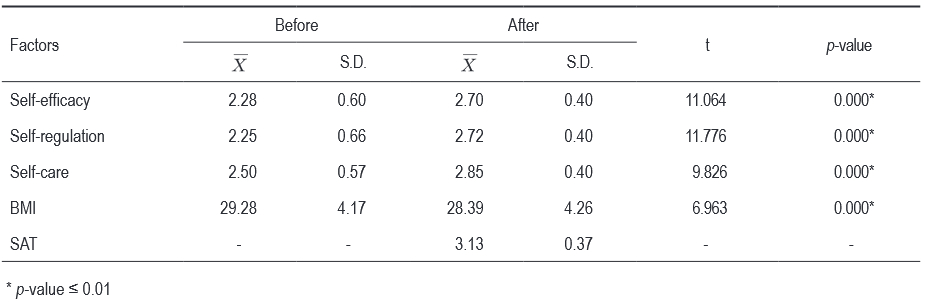
Table 2: The differences in the averages of the 3-Self health behaviors, Body Mass Index (BMI) value and the participants’ satisfaction (SAT) with the program at completion and 6 months later. (n=173)
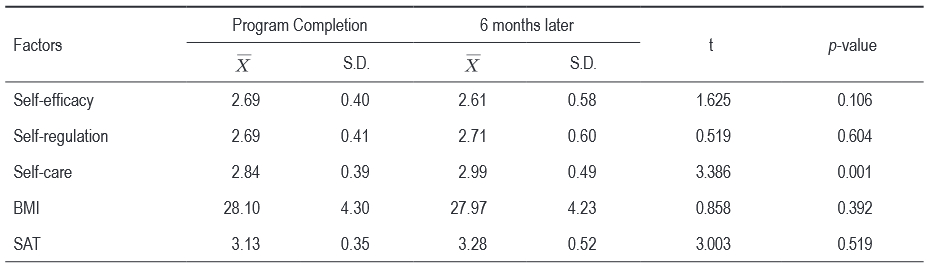
Table 3: The differences in averages of the 3-Self health behaviors to the ability of the participants to lose weight or not. (n=173)
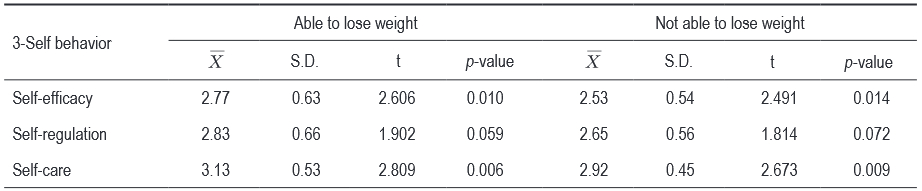
Table 4: The relationship between the average value of 6 factors of PROMISe model and 3-Self health behavior change and participants’ satisfaction with the program 6 months after finishing program. (n=173)
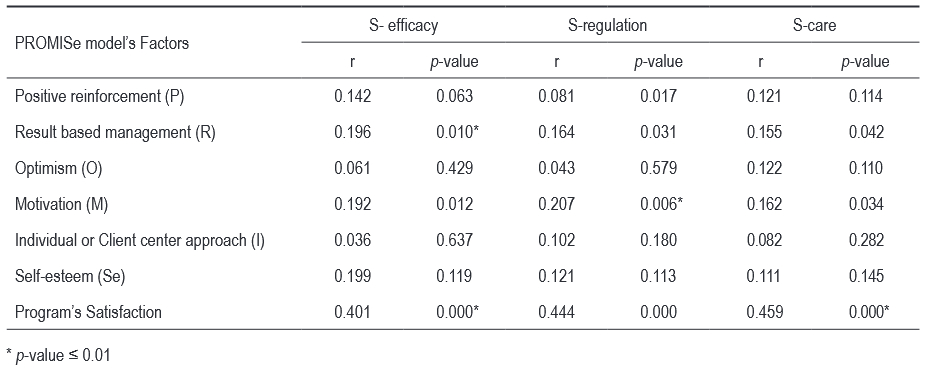
Table 5: The relationship between the average value of 6 factors of PROMISe model and the sustainability of health behavior change in 3 areas of the participants. (n=173)
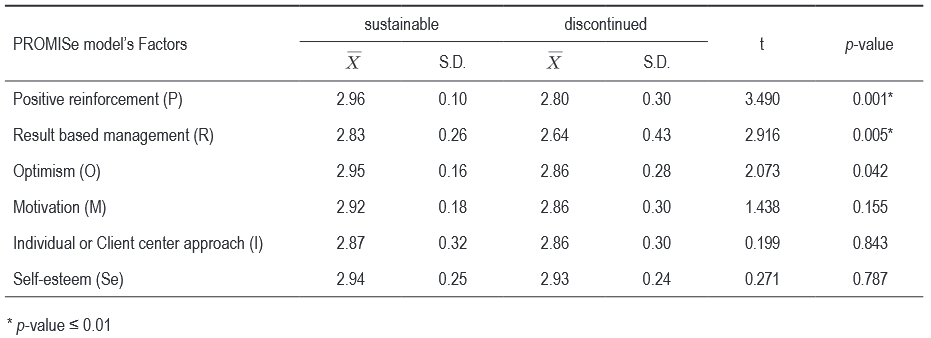
Table 6: The relationship of the average value of 6 factors of PROMISe model and the participant’s ability to lose weight. (n=173)
(for example, controlling their eating behaviors, regularly selecting food according to their individual daily energy needs or making changes during social events, improved emotional control, mind training, self control with regards to weight monitoring etc.) were what caused their health behavior changes to be sustainable.
5.2 The participants who neither maintained health behavior changes nor lost weight stated that their failure to change was due to inability to control their appetite, health problems (such as diabetes), poor time management, not having enough time for exercise, consuming food they didn’t cook themselves, and attending social events.
5.3 The participants suggested that the hospital should set up a Weight and Disease Reduction Club, conduct regular meetings on Saturday or Sunday, every few months, and extend group activities training. The training material should include some games and simple formulas for calculating calories. The extended group activities should include low calorie food cooking classes, exercise classes, and the daily diet/energy intake review with an advisor. The hospital should continue selling healthy food, create a distribution channel to disseminate useful information and news to the general public, develop a mentoring program, and establish a call center or special clinic for people struggling with obesity.
1. The results of this research showed that 3-Self health behaviors change in 3 areas had an inverse relationship to the BMI value. Using the PROMISe model to develop program activities was effective: 80.5% of participants were satisfied with the program. The aim of activities was obesity problem solving concentrated in diet, exercise, and emotional control. The principles behind activity organization came from behavioral and management sciences. The program started with Positive reinforcement (P). The specialist provided training related to the benefits of health behavior changes on reducing obesity. Result based management (R) was applied by using Appreciation-Influence-Control (AIC) management techniques (“appreciate through listening, influence through dialogue, control through action”) in a practical training which identified what self behaviors contributed towards obesity, set individual weight loss targets, and helped participants learn to figure out their own weight loss solutions.9,10 Optimism (O) was used to help change participants’ personal perceptions. The mentors, who were participants from the previous program, shared their observation of their personal experiences of failure in their daily lives and their perceptions of how they turned the failure into learning experiences to effect lasting health behavior changes. The researcher used Motivation (M) as the tool to cheer up the participants during the program. The research used positive language, conducted weight loss competitions similar to the U.S TV Program “The Biggest Loser”, and sent regular messages or program status updates to motivate the participants throughout the whole program. Individual or Client centered approach (I) was to focus on the participants’ perception. Nutritionists and mentors provided advice, recommendations and suggestions to participants during group activities and food control practices. This approach was to ensure that all participants had the same understanding. The researcher used rewards and complements to build Self-esteem (Se). The certificate ceremony at the end of the program enhanced the Self-esteem of the participants. The success in either weight loss or 3-self health behavior changes after the program increased the self-confidence levels of the participants, especially those with diseases. This was all consistent with Tanphaichi’s research: to solve obesity by changing the health behaviors requires an appropriate learning system about diet and exercise, especially developing awareness of weight control.11
2. The sustainability of the health behavior change at the end of the program and 6 months later, and the relationship between the 6 factors of PROMISe model to 3-Self health behavior change was described below.
2.1 The relationship between 3-self health behavior change in 3 areas and BMI value at the program’s end was similar to the relationship 6 months later: the better the health behavior changes, the lower the BMI value. Although the average of Self-care showed a significant difference, the result was in the same direction. Satisfaction with the program 6 months later was higher than than just after the program finished. The average of 3-Self health behavior change in 3 areas between those participants who could and those who could not lose weight at the end of or 6 months after the program showed significant differences in Self-efficacy and Self-care behaviors. Participants who lost weight showed more ability to control themselves than did the participants who could not, along with the understanding of appropriate health behaviors, food control practice, success in losing weight, and the belief that appropriate health behaviors which helped them lose weight would encourage them to maintain weight control and continue to positively change their health behaviors. On the other hand, the lower average in Self-regulation of the participants who could not lose weight showed their lack of self control both during or 6 months after the program. Back in daily life, although these participants realized the benefits of appropriate health behaviors and believed in their ability to lose weight, they seemed unable to control themselves to perform continuous positive health behavior changes.
The summary of the focus group meeting indicated the reasons that the participants used as excuses for not losing weight, but gaining instead. This evidence corresponded well to statements made in the 2010 obesity report from Bureau of Policy and Strategy, Minister of Public Health12 which mentioned that Thai people whilst able to lose weight during weight reduction treatments, were not able to maintain that loss and began to gain the weight back after stopping the program in a yo-yo effect. The stages of change theory of Prochaska & Diciemente (1983)13 stated that people have to maintain regular healthy behavior over 6 months in order to habitualise that behavior and arrive at the “maintenance” stage. They need to learn how to control and manage their hunger and emotions using motivation strategies to keep on with healthy behaviors.
2.2 The results of this study confirmed that targeted behavior monitoring on weight loss, together with a motivational environment during and after the program promoted continuous changes in health behavior. All 6 factors of the PROMISe model were influential in effecting changing behaviors changes with regard to diet, exercise and emotional control and thus weight reduction. The benefits of being healthy and the results of health behavior changes such as lowering blood pressure or blood sugar levels acted as Positive reinforcement (P) for the participants. Result based management (R) enhanced the participants’ ability to control their hunger and emotions as well as participating in regular exercise, in accordance with the weight reduction activities plan. Optimism (O) transformed the participants’ perception of their failures into to learning lessons for their eventual better health behavior change.
Recommendations
1. The Head of the Nursing department should introduce to obese patients and encourage their participation in the Weight and Disease Reduction Program, using the PROMISE model to effect health behavior changes in 3 areas.
2. The health behavior change activities should increase interpersonal connections by using mentors, to improve communication and relationship building among the participants, to share failure and success stories, to encourage the participants during and after the program, and to help create the community for better health behavior change.
3. The health behavior change activities should focus on participants’ self-practice. The patients should record and compare the results of each practice by themselves. The role of Nurses and Public health officers is only to arrange the motivational environment.
4. The management of nursing department should lead an integrated program of health promotion and disease prevention using the PROMISe model in the health care process of treating patients with metabolic diseases related to obesity.
Suggestions for future study
1. There should be a study to investigate what other factors contribute either to the success of the participants who are able to not only sustain health behavior changes and also lose weight and or failure of the participants who can neither sustain health behavior changes nor lose weight.
2. A follow up investigation into health behavior change sustainability should be conducted one to two years after participation in the program, together with continual improvements of motivational activities for the participants to practice on their own, after their return to their usual daily lives.
3. There should be a study on the effectiveness of the improvement program in health behavior change in participants who face particular challenges with the “yo-yo effect” using the PROMISe model, and focusing on Optimism.
4. There should be a study of knowledge management of the participants who are able to not only effect permanent changes in their health behaviors but who also achieved their targeted weight reduction.
Using the PROMISe model to design and manage activities leading to health behavior changes definitely influences and increases the sustainability of the changes. For the permanent sustainability of health behavior change, future program activities should concentrate on designing activities directly related to the factors which the study showed had the biggest impact, namely result based management, positive reinforcement, and optimism.
Program Participant
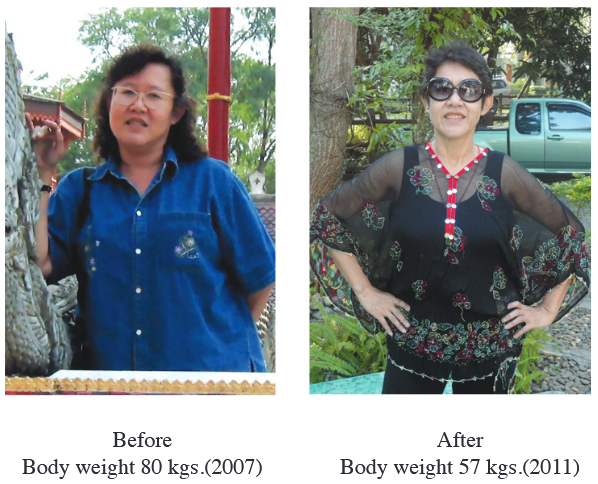
Thank you Mrs. S for the permission to print your pictures.