Since its introduction in 2000, digital mammography has become an accepted standard of care in breast cancer screening and has paved the way for a new groundbreaking technology-breast tomosynthesis. With breast tomosynthesis, images of a breast are acquired at multiple angles during a short scan. The individual images are then reconstructed into a series of thin, high-resolution slices typically 1mm thick, which can be displayed individually or in a dynamic ciné mode. A tomosynthesis data set virtually elimi- nates detection challenges associated with overlapping structures in the breast, which is the primary drawback of conventional two dimensional (2D) mammography. Figure 1 illustrates the basic principle. As is known from standard computed tomography (CT) body imaging, three dimensional cross sectional slices often improve visibility through the reduction of superimposed structures.
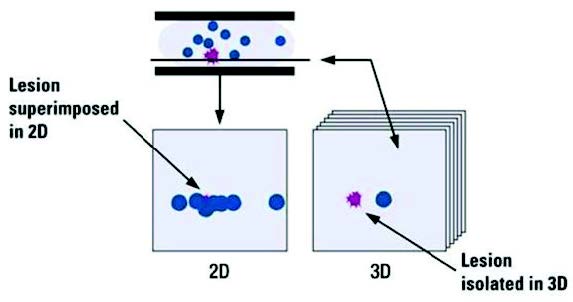
Figure 1: Overlapping structures hides lesions in two dimensional (2D) that can be clearly seen in a three dimensional (3D) cross sectional slice.
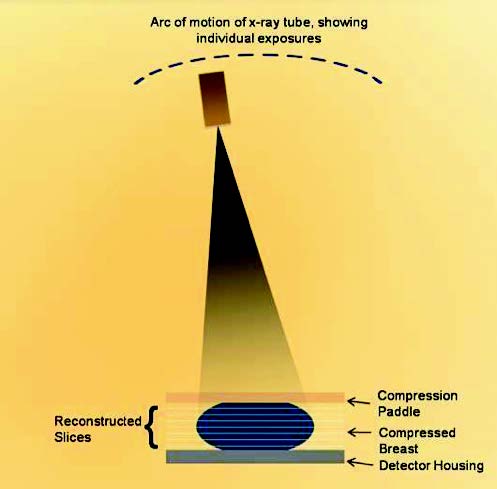
Figure 2: Schematic shows principle of operation of tomosynthesis system.
Figure 2 shows the geometry used in tomosynthesis imaging. The breast is compressed in a standard way as is done in conventional mammography. While the breast is compressed, the x-ray tube rotates around the breast in a limited angular sweep, acquiring a number of low-dose projection mammograms. These are then reconstructed into the cross-sectional slices, typically 1mm in separation. Each slice is parallel to the detector housing. Different manufacturers use different acquisition geometries, but all share a common method of performing limited angle tomography. Table 1 shows the system details for four systems. They differ in the scan angle, number of projections, and the scan time.
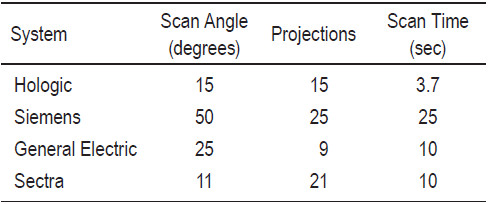
Table 1: Scan parameters used in some tomosynthesis systems.
Breast tomosynthesis systems from several major manufacturers have been available in Europe and other countries recognizing the CE mark since 2008. In February 2011, Hologic’s Selenia® Dimensions® tomosynthesis system was the first commercial system approved by the United States (U.S.). Food and Drug Administration (FDA). The FDA approved the system for use in the same clinical indications as 2D mammography including breast cancer screening and diagnosis.Other manufacturers have announced plans to bring tomosynthesis to the U.S. but as of today, Hologic is the only vender with a commercial system in the U.S.
This article reviews the results of a number of clinical trials of tomosynthesis systems.
The first multi-center tomosynthesis trial was the one performed by Hologic in support of their FDA submission. This trial compared the performance of 2D digital mammography plus tomosynthesis imaging (combo-mode) to that of 2D mammography alone. All subjects in the trial had bilateral 2-view mammograms (mediolateral oblique (MLO) and craniocaudal (CC) in both 2D and tomosyn- thesis imaging modes).
Two reader studies were conducted by Hologic using images from the initial clinical trial data set. The reader study results were analyzed using Receiver Operating Characteristics (ROC) methodology, with the area under the curve measuring the ability of individual radiologists (readers) to correctly characterize the presence or absence of disease.
Results from the first reader study were presented by Rafferty at the Radiological Society of North America (RSNA) annual conference in 2007, and both reader studies were presented at an FDA panel meeting in September 2010.1,2 In both studies, the performance of 2D mammo- graphy plus tomosynthesis was shown to be significantly superior to the performance of 2D alone. In addition, both studies showed a reduced non-cancer recall rate. These results were consistent with those of an independent third reader study from University of Pittsburgh researchers who found a 7% improvement in the area under the ROC curve for 2D plus tomosynthesis compared to 2D alone.3
The clinical benefits of tomosynthesis as demonstrated by Hologic’s clinical trials and independent trials conducted by a variety of researchers world-wide are discussed below.
Hologic’s clinical trials showed that radiologists reading in combo-mode compared to 2D alone demonstrated improved sensitivity in the measure of how many cancers are detected. The figure below shows a hypothetical example of ROC curves based on 2D plus tomosynthesis imaging.
A Comparison of the Ability of Readers to Correctly Characterize the Presence or Absence of Cancer with Conventional 2D Mammography and 2D Mammography Plus Tomosynthesis.
The first trial results on improved cancer detection in a screening environment were presented by Skaane at the RSNA 2011 conference.4 In an analysis of the first 3,500 patients entering a prospective trial of over 20,000 women, Skaane observed a relative increase of 47% in cancer detection using tomosynthesis compared to 2D mammo- graphy alone.
A reduction in recall rates was reported for 2D plus tomosynthesis compared to 2D alone in the two Holog- ic reader studies and the reader study by Gur et al.5 The Gur reader study suggested that the use of tomosynthesis during baseline screening mammography may reduce the recall rate by 28%. Rafferty1, in her 2007 RSNA presentation, estimated the recall reduction rate to be over 40%. Subsequent studies have also found a significant reduction in recall rates with tomosynthesis.
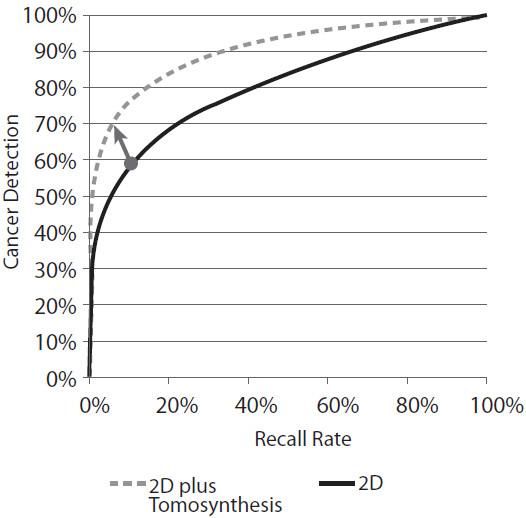
Figure 3: The diagonal arrow shows how an individual’s cancer detection rate can be improved and their recall rate reduced using a technology that has a higher ROC curve.
The three reader studies referenced above used two-view mammography for both 2D and tomosynthesis imaging. One of the reader studies also investigated a 3rd arm: single-view tomosynthesis (MLO) imaging in combination with 2-view (CC and MLO) 2D imaging.2 In this reader study, the performance of 2D imaging plus tomosynthesis MLO showed that the tomosynthesis MLO-only arm per- formed better than 2D imaging alone, but not as well as 2D plus both tomosynthesis views.
These results are consistent with several other studies, illustrating that MLO-only tomosynthesis is likely to be inferior to two-view tomosynthesis:
- Rafferty6 found that 12% of lesions were better seen on the tomosynthesis MLO image, 15% better seen on tomo CC and 9% of lesions were visible only on tomo CC.
- Similar results were reported by Baker7, who found 8% of lesions were visible only on the tomosynthesis CC view and 1.4% only on the tomo MLO.
The clinical trial data in Hologic’s reader studies has been analyzed by separating the image sets into calcifi- cation and non-calcification cases. Rafferty1 found that 2D plus tomosynthesis offered a very significant increase in performance relative to 2D imaging for cases involving masses and distortions. For the imaging of cases involving microcalcifications, there was a small, but not statistically significant, improvement in the ROC performance with the addition of tomosynthesis. Other studies have looked at calcifications and their visibility with tomosynthesis. For example, Kopans8 found that the characterization of calcifications in tomosyn- thesis was equal or superior to their characterization in conventional digital mammography in 92% of the cases studied.
Other studies have looked at calcifications and their visibility with tomosynthesis. For example, Kopans8 found that the characterization of calcifications in tomosyn- thesis was equal or superior to their characterization in conventional digital mammography in 92% of the cases studied.
Tomosynthesis has been shown to improve the per- formance of mammography in both fatty and dense breasts. Researchers have performed an analysis on cases following their grouping into fatty breast (defined as Breast Imaging-Reporting and Data System (BI-RADS) 1 and 2) and dense breast (defined as BI-RADS 3 and 4) sub-groups. Rafferty9 studied the performance of tomosynthesis in women with dense breasts and found an increase in the recall for cancer cases and a reduction in the recall rate for non-cancer cases.
In a separate study, Rafferty10 found that 2D plus tomosynthesis was significantly better than 2D mam- mography alone in ROC performance for both fatty and dense breasts. While there was a gain in the area under the ROC curve in both breast density types, the gain was 2-3 times higher in dense breasts than it was in fatty breasts. Rafferty10 also reported large recall rate reduc- tions in both fatty and dense breast types.
The use of tomosynthesis in diagnostic assessment offers the opportunity for both improved performance and a reduction in the number of x-ray images needed, as well as superior performance compared to 2D mammography in predicting tumor size, demonstrating margins, extents of lesions, and in staging.
Zuley et al.11 found comparable sensitivity and speci- ficity in the use of two-view tomo imaging in place of the additional diagnostic 2D views typically taken.
Tagliafico12 found that tomosynthesis could replace spot compression views, lowering both radiation dose and offering the potential to reduce biopsies on nonmalignant lesions.
Svahn13 showed that the combined diagnostic perfor- mance of digital mammography and tomosynthesis is superior to either digital mammography or tomo- synthesis alone.
Michell14 showed that tomosynthesis is superior to 2D mammography in predicting the histological tumor size because tomosynthesis demonstrates the margins and extents of the mammographic lesions more clearly.
Fornvik15 found breast tomosynthesis superior to digital mammography in the assessment of breast tumor size and stage.
Meacock16 found that tomosynthesis was more accurate than 2D in tumor size measurement.
Early investigators using tomosynthesis hypothesized that three dimensional (3D) breast imaging would replace 2D imaging. That may yet happen, but so far the best clinical performance of tomosynthesis imaging has been shown when combined together with a 2D exam, i.e. 2D plus 3D imaging.
There are several reasons why acquiring both a 2D mammography and tomosynthesis image together are useful, especially in screening. It is well known that com- parison of current images with prior images is standard mammography practice and critical to perceive subtle changes which may be associated with a cancer. Obtaining a 2D exam along with the tomosynthesis exam allows direct comparison of current 2D images with prior 2D images.
The 2D exam is also useful for the rapid detection of calcifications. Clusters of calcifications are more easily and quickly appreciated with 2D because all the calcifica- tions appear together in one image.
The tomosynthesis portion of the 2D plus 3D exam is also critical. The tomosynthesis image reduces structure overlap, minimizing recalls for overlapped structures and better demonstrates masses and architectural distortions. Thus we see that 2D and Tomo are complementary and acquired together offers an advantage in clinical use.
There may be methods to eliminate the need to separately acquire the 2D exam through mathematical algorithms that generate a synthesized 2D image reconstructed from the Tomo dataset. This approach is being evaluated in a screening clinical trial in Oslo, Norway, with principal investigator Per Skaane.
Breast tomosynthesis is an exciting new technology that offers the potential for improvements in both breast cancer screening and diagnostic evaluations. Clinical trial results demonstrate that:
- 2D mammography plus tomosynthesis is superior to 2D alone
- The sensitivity of 2D mammography plus tomosyn- thesis is higher than 2D alone
- The screening recall rate of 2D mammography plus tomosynthesis is lower than that of 2D alone
- Performance using both tomo CC and MLO views was greater than tomo MLO alone
- 2D mammography plus tomosynthesis provides improved performance in both fatty and dense breasts, compared to 2D alone, with the performance gain in dense breasts higher than in fatty breasts.
- Tomosynthesis is useful in diagnostic imaging of the symptomatic patient. Tomosynthesis has the potential to reduce the number of exposures needed for diagnostic imaging and provide other diagnostic benefits including enhanced performance in assessing tumor size and stage and more clearly demonstrating margins and extent of lesions.
A 42-year-old female presented with a small mobile mass on the inner aspect of the left breast for a period of two months. Previously her annual mammogram check-ups were negative. The 2D mammogram reveals a heteroge- neous dense breast with a craniocaudal (CC) view, and no abnormality is seen (Figure 6). The 3D breast tomosynthesis shows a well defined mass on the upper inner quadrant, the size is 16x18mm (Figure 7). The ultrasound is incon- clusive in identifying the mass (Figure 8).
The biopsy revealed a benign intraductal papilloma. No evidence of malignancy was observed. The 3D breast tomosynthesis is very helpful to ensure more accuracy and to give physicians additional information in the case of a dense breast.1-4 This modality will reduce the number of recalls and also reduce further sophisticated investigations in the case of clear cut criteria of imaging by BI-RADS.
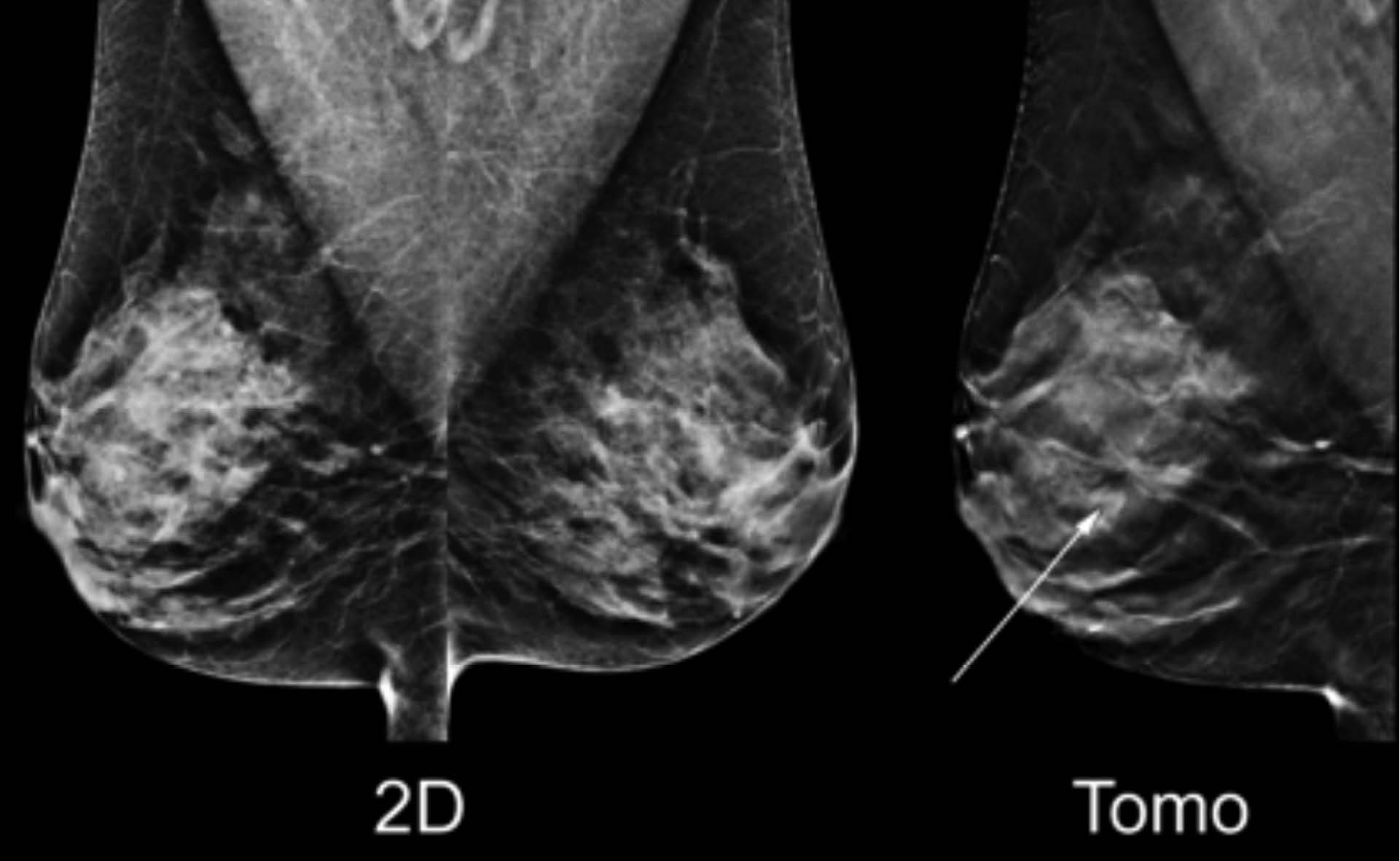
Figure 4: Increased cancer detection: the tomosynthesis reconstructed slice shown on the right reveals a defi nitive spiculated mass that is only faintly revealed in the 2D image shown on the left. (Diagnosis: Invasive Ductal Carcinoma)
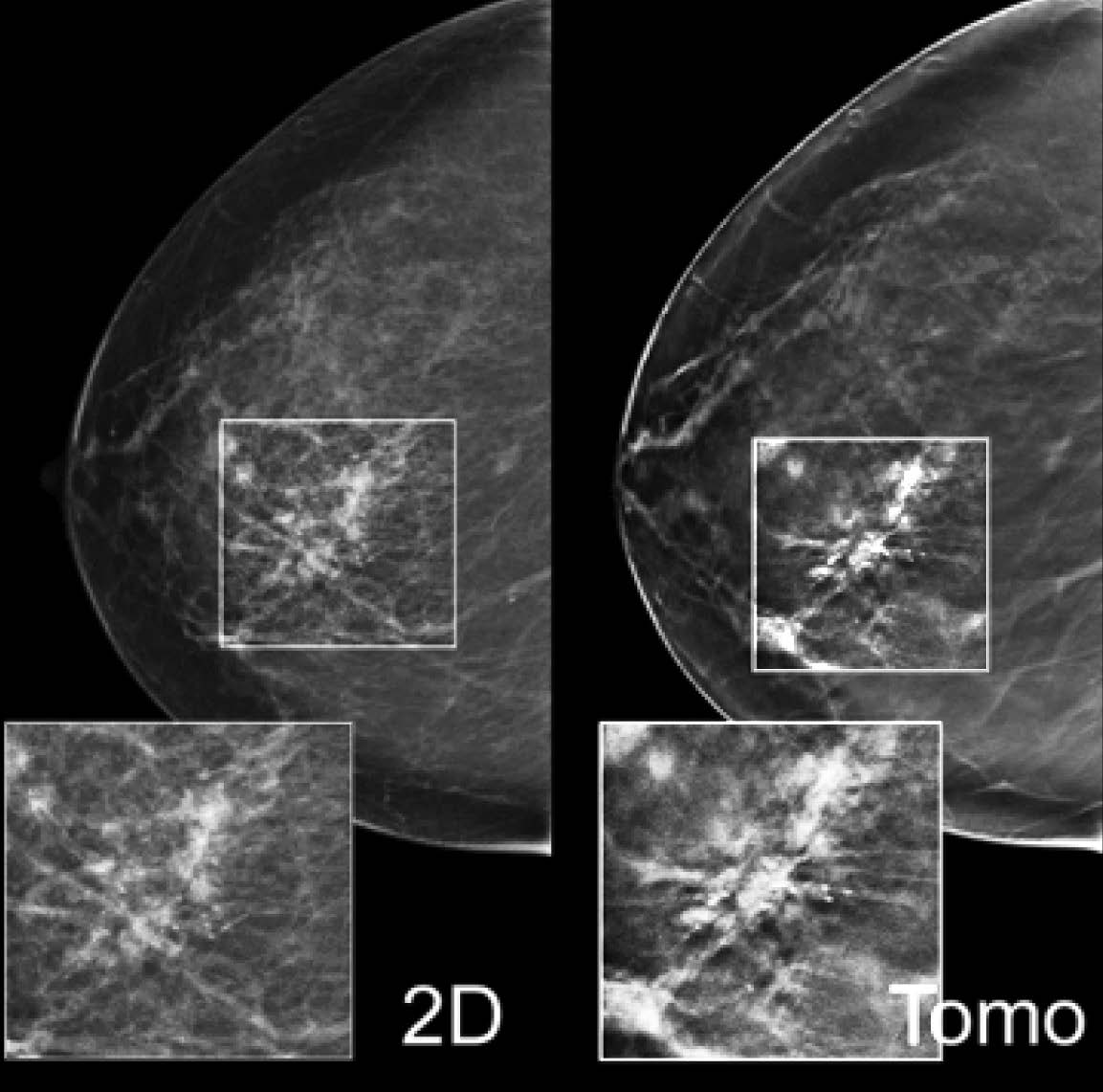
Figure 5: Added value for calcifications:the 2D mammogram on the left shows right medial microcalcifications. The tomosynthesis reconstructed slice on the right illustrates the associated architectural distortion only revealed on the CC tomosynthesis image and not shown on the mammogram. (Diagnosis: Ductal Carcinoma In-situ/High Grade)
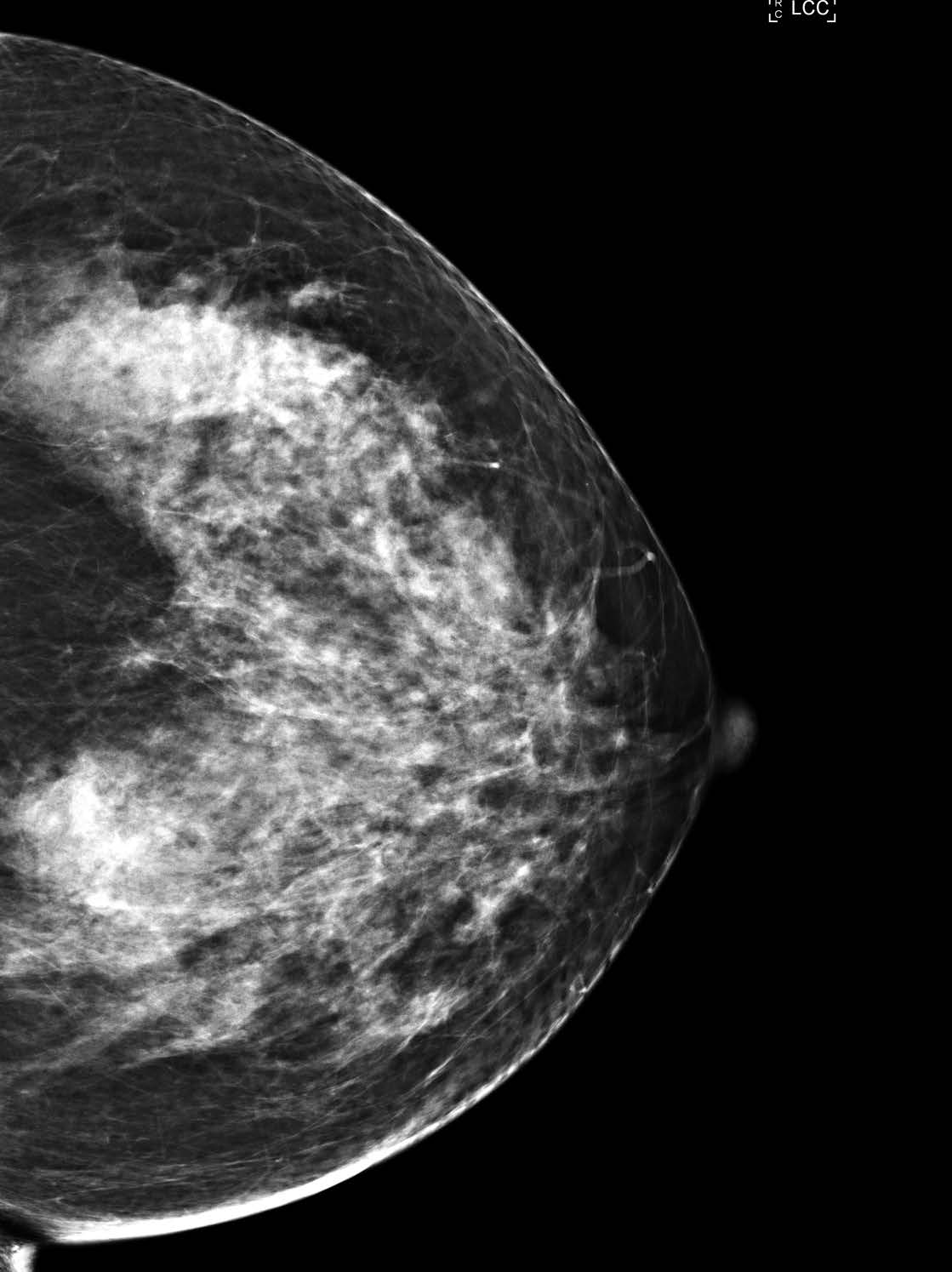
Figure 6: The 2D mammogram reveals a heterogeneous dense breast with a craniocaudal (CC) view.
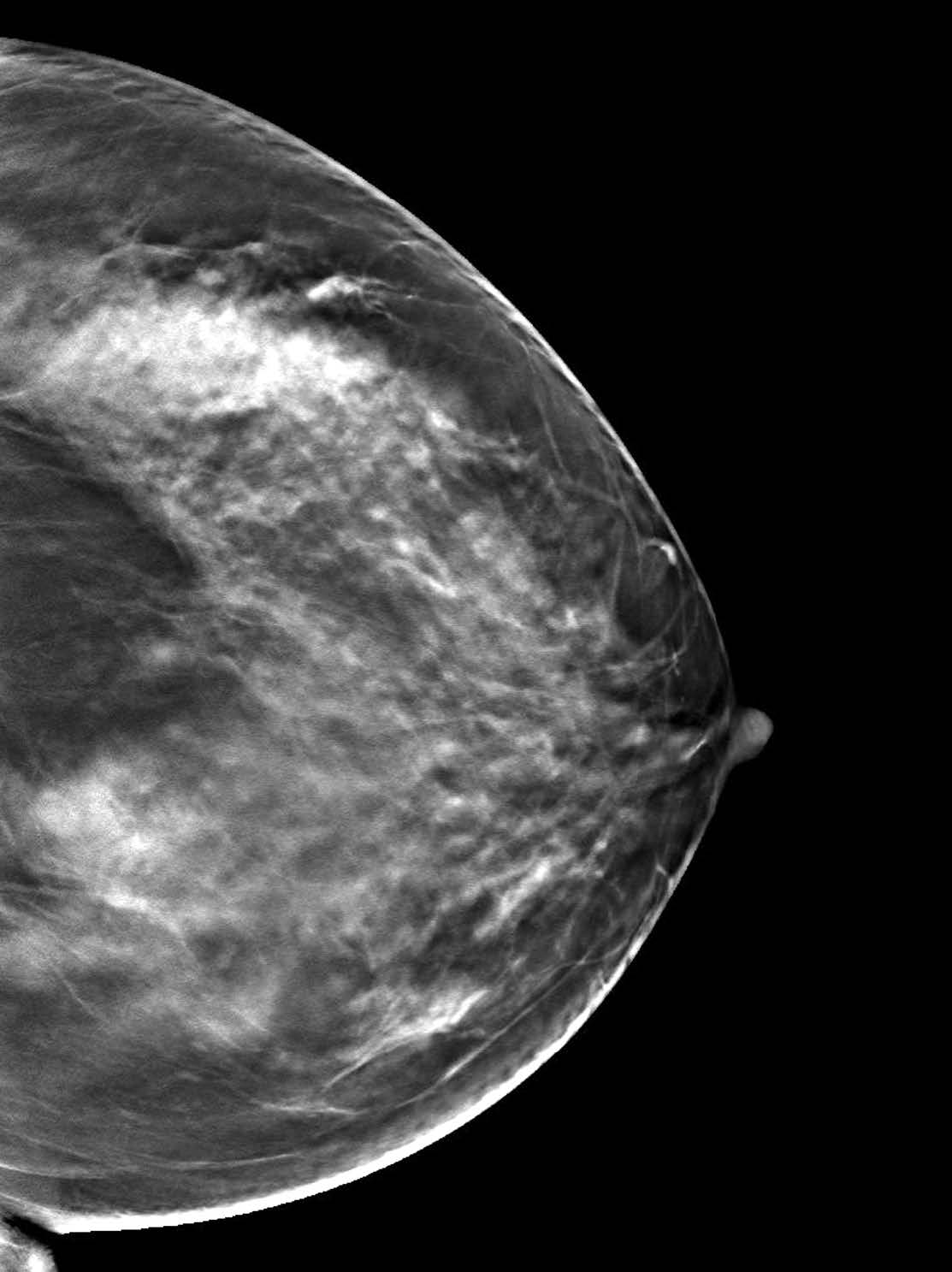
Figure 7: The 3D breast tomosynthesis shows a well defined mass on the upper inner quadrant; the size is 16x18mm (arrow).
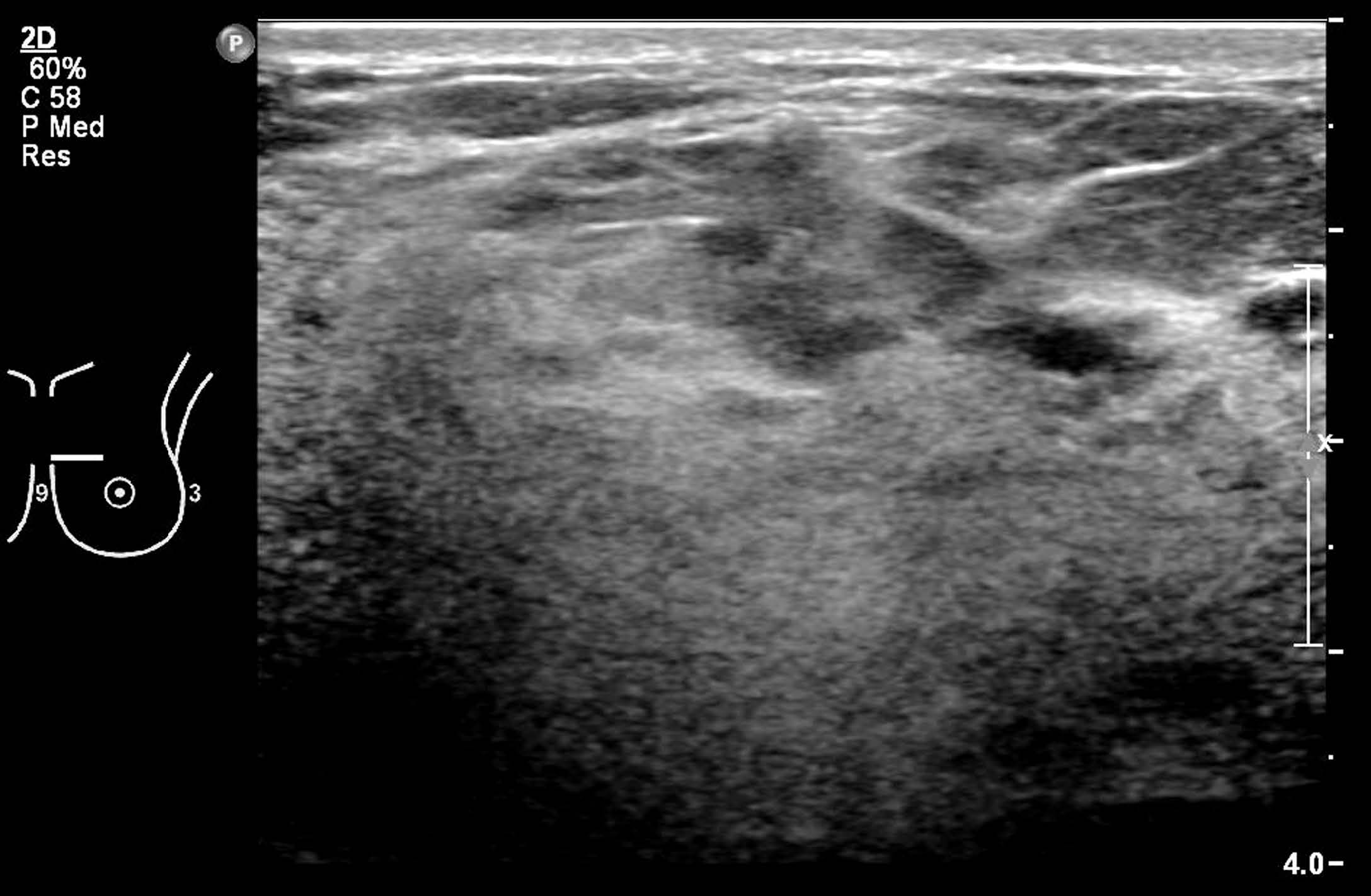
Figure 8: The ultrasound is inconclusive in identifying the mass