Cardiac catheterization and percutaneous coronary intervention (PCI) is the gold standard diagnostic test and management for coronary artery diseases.1 A femoral artery catheter insertion site is commonly used for the procedure. After the procedure, patients are restricted to complete bed rest with no hip flexion for up to 6-10 hours to prevent bleeding and/or hematoma occurrences at the site of incision, which as a result causes back pain and lower extremities self-care deficits to the majority of these patients.2 Several studies have shown that based on the long duration of complete rest and unchanging position, patients experience back pain, dissatisfaction, there is an increase in costs, and also an increase in nursing task loads.2-5 To reduce patients’ discomfort, several studies revealed that modified positions could result in significantly reducing back pain and improving patient comfort.6-8 However, previous studies recommended that the position after coronary angiography should be that the head of the patients’ bed should be raised about 30 - 45 degrees. This position could increase comfort and decrease back pain of patients without increasing vascular complications.3,4
Bangkok Heart Hospital, Thailand provides cardiac catheterization and PCI service to more than 800 patients with coronary artery disease (CAD) each year. After the procedure, the patients are required to rest in bed and remain in a supine and flat position for up to 6 -12 hours as routine care. Concerning patient patient discomfort without increasing the incidence of vascular complications. According to previous evidence, this study was designed to examine the effect of a nursing intervention for patients receiving cardiovascular angiography and interventions by applying a 30 - 45 degrees reverse Trendelenburg position (RTP) and to investigate the incidence of vascular complications of the intervention and routine care.
Study Design
A pilot randomized controlled trial was conducted in 70 patients. The patients were randomly assigned to either the experimental or control group. The control group (35 patients) received routine care after the intervention, whereas the experimental group (35 patients) received RTP at 30 - 45 degrees. The allocation sequence was put into a sealed opaque envelope. The blinded randomization was drawn by the principal investigator.
Study Population and Sample
The populations in this study were patients who received cardiovascular angiography and interventions via the femoral artery and received post procedural care at the intermediate cardiac care unit, Bangkok Heart Hospital from December 2015 to February 2016. The sample sizes in this study were 70 patients. The control group was 35 patients and the experimental group was 35 patients. The calculation of the sample size was based on the “rule of thumb” that 30 participants is common for pilot studies.7 A sample size of 35 will be adequate given the specific quantitative aims of this pilot.
The inclusion criteria included: elective cardiovascular angiography and interventions via the femoral artery, age between 21-90 years, can communicate and cooperate well with the sedation score = 1 and hemodynamically stable.
The exclusion criteria included: being an emergency case for cardiovascular angiography and interventions, having a history of bleeding disorders or the internatioal normalized ratio (INR) > 2, having a history of back pain disorders and active bleeding and hematoma at the femoral access site immediately after the procedure.
Intervention
After the procedure, patients received care at ICCU, Bangkok Heart Hospital. The patients randomized as the experimental group received a 30 - 45 degrees RTP (Figure 1). That is, the head is elevated higher than the feet with the affected leg straight up to 30 to 45 degrees. The patient is still lying on his or her back and facing the ceiling. The patients received routine care, remaining in a supine and flat position for 6 - 12 hours, with the affected leg straight. Patients were asked to assess their back pain and rate its severity using the numeric rating scale (range 0 = none -10 = severe pain). Blood pressure and vascular complications were measured at the zero, 1st, 2nd, 4th, and 6th hours as well as in the next morning after the proce- dure.
The data collection tools in this study included demographic questionnaire, patient’s clinical profile form, numeric rating scale to measure back pain scores and Kristin Swain’s checklist for checking vascular complication.
Ethical consideration
The data collection was conducted after receiving approval from the Human Research Ethics Committee, Institutional Board Bangkok Hospital (Head Quarters) with approval BMC-IRB No 2015-09-038. All patients were informed of the study objectives, procedure, and possible benefits and barriers. They were assured of confidentiality and the ability to decline participation or withdraw from the study at any time.
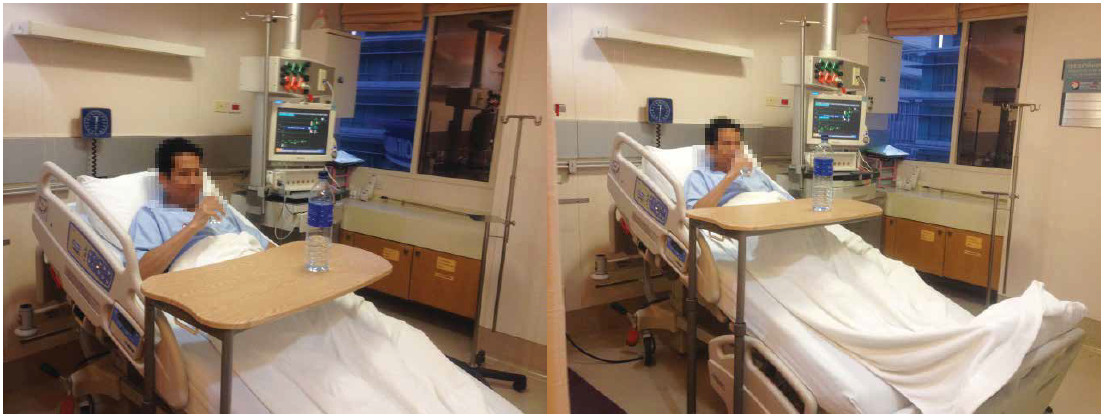 Figure 1: Reverse Trendelenburg Position 30-45 degrees.
Figure 1: Reverse Trendelenburg Position 30-45 degrees.
Data Analysis
The collected data were analyzed by the Statistical Package for the Social Sciences (SPSS version 22). Descriptive statistics (mean, standard deviation, and percentage) were used for all variables. Demographic data age, body weight, height, time for procedure and blood pressure were compared between the experimental and control groups using Independent samples t-test to determine whether any difference between group. The difference of back pain between the two groups was compared using Independent samples t-test.
Of all participants, 35 patients took part in the experimental group (11.4% women and 88.6% men) and 35 patients participated in the control group (34.3% women and 65.7% men). The mean age of the experimental group was 59.51 ± 8.03 and the control group was 62.66 ± 8.90. The average of body weight in the experimental and control groups were 70.41±15.90 and 73.82±14.17 respectively. The average of height in the experimental group was 167.00 ± 10.26 and in the control group was 163.77±10.71. Average of time for procedure in the experimental group was 119.57±37.54 and in the control group was 131.57 ±76.93. There were no statistically significant differences in age, body weight, height and the time for procedure (p > 0.05) as shown in Table 1. In addition, there was no significant difference in the arterial blood pressure at each determined interval (Table 2).
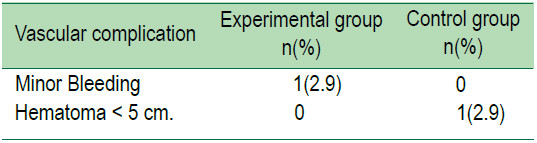
Comparing back pain levels, there were statistically significant differences between the experimental group and the control group at each of the six pain assessment time periods. The experimental group had lower levels of back pain than the control group at all the assessment time periods (p < 0.05) (Table 3). Back pain scores in the experimental group were less than in the control group, and significantly different (p < 0.05). The incidence of minor bleeding was 2.9% in the experimental groups and hematoma was 2.9% in the control group (Table 4).
Table 1: Demographic and clinical characteristics of the participants.
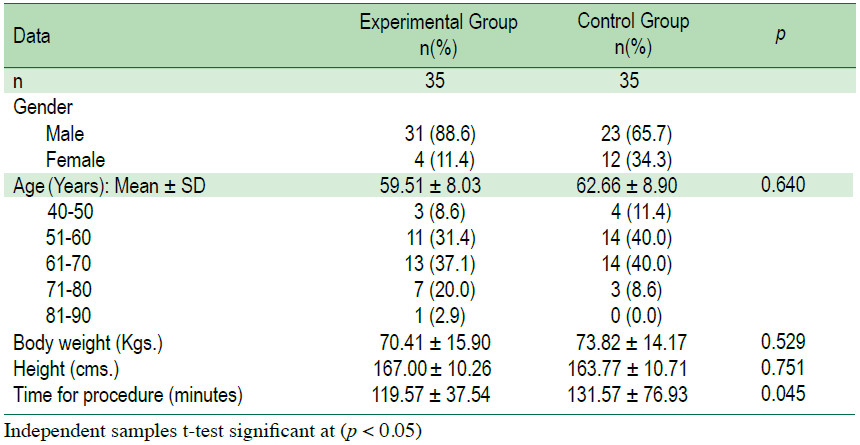
Table 2: Average levels of blood pressure in each determined interval in the experimental and control group
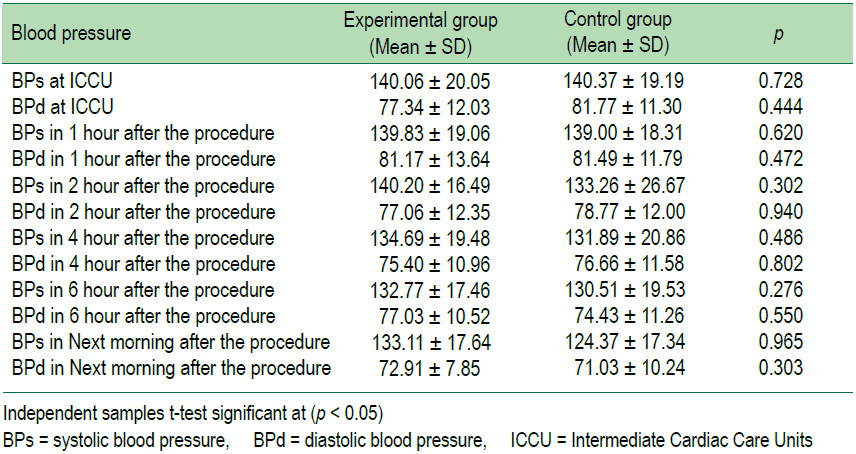
Table 3: The comparison of the degree of back pain scores between the experimental group and the control group.
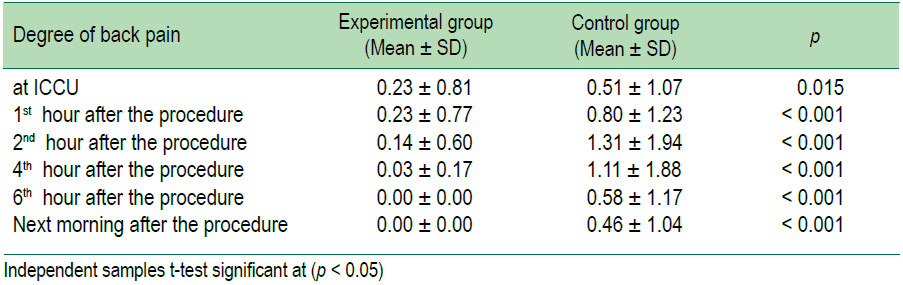
Table 4: Vascular complication rate in the experimental group (n=35) and control group (n=35).
The results obtained in this study show that reverse Trendelenburg position (RTP) can reduce patients’ back pain after cardiovascular angiography and interventions, the degree of back pain scores in the experimental group was less than in the control group, with statistical significance (p < 0.05). This is due to the patient being placed in RTP at 30-45 degrees position and this had less/no effect on inner-muscle pressure in the lumbar muscles.8Patients were allowed to be ambulated and to undertake their self-care activities. Patients could freely and more frequently move other parts of the body, thus requiring less assistance from nurses. The findings of this study are similar with the results from a previous study.2,9,10 It has been shown to be safe and to promote physical comfort. This new technique is not only practical; it is also time-saving and beneficial for both patient and nurse.
The findings of this study show that RTP after cardiovascular angiography and interventions can reduce or prevent back pain without increasing the chance of vascular complications.
In addition, the results demonstrated that the number and percentage of patients with bleeding was not different. Minor bleeding was found in one patient (2.9%) of the experimental group and hematoma < 5 cm. was found in one patient (2.9%) of the control group as well. There was no active bleeding in both groups. This finding showed changing body position in to reverse Trendelenburg position (RTP) after cardiovascular angiography and interventions has minimal or no effect on vascular complications. The results of this study are consistent with previous studies indicating changing positions is safe with no significant difference between the control group and the experimental group in the incidence of vascular complications at the access site after cardiovascular angiography and interventions.3-6,11
We would like to extend our special thanks to The Bangkok Health Research Center at Bangkok Hospital, and all staff members for fully supporting this study. We would also like to thank to all the patients and nurses at the intermediate cardiac care unit, Bangkok Heart Hospital, for their assistance and cooperation.