The associations between cardiac problems and neurological problems are common. The most well known one is EKG changes in patients with subarachnoid hemorrhage (SAH).EKG changes can be seen as much as 50-100% in acute stage of SAH.1,2 The echocardiography also reveals the abnormalities in left ventricular (LV) function in these patients. Many neurological conditions can result in transient LV dysfunction which can be demonstrated clearly by echocardiography with or without EKG change. This finding was first reported as “Takotsubo syndrome” in 1991 by Satoh.3 We report cases of intracerebral hemorrhage with low ejection fraction without EKG change.
A right handed male patient aged 46 years, without prior serious medical history came to the hospital with symptoms of dysarthria, right facial palsy and right hemiparesis. CT scan revealed large left parietal intracerebral hematoma. The preoperative EKG showed nonspecific ST-T change. The patient underwent echocardiography on the first day of onset. The echocardiogram revealed dilated left ventricle and global poor contraction in which ejection fraction (EF) was 35-40%. No blood clot was seen. No other abnormality was seen. He underwent the cranial surgery uneventfully and no cardiac event occurred during intraoperative period. Post operative period was uneventful. The follow up echocardiogram performed on the 2nd day after surgery revealed normal LV size, fair to good contraction, EF=50%. The exercise stress echo was also negative. The echo- cardiogram was performed again, two years later. The results were normal LV size, normal contraction, EF 51%.
A 56-year-old, right handed female patient who was otherwise healthy, suffered from sudden onset of severe headache and loss of consciousness 4 hours before arrival. CT scan showed the subarach- noid hemorrhage with brain edema. CT scan showed Fisher grade III. (Figure 1) She underwent the 4 vessels cerebral angiogram and was diagnosed as having a ruptured anterior communicating artery. (Figure 2-3) Her chest film showed pulmonary edema. (Figure 4) Her blood pressure dropped to 80/40 mmHg. The EKG showed normal sinus rhythm. The echocardiography (Figure 5) showed dilated left ventricle,poor left ventricular systolic function (EF=33%), akinesia of anterior, anteroseptal and anterolateral wall, therefore her diagnosis was congestive heart failure. Although the inotropic drug, dobutamine, was maximally infused, her systolic blood pressure remained under 100 mmHg. The intraaortic balloon pump (IABP) was inserted to augment the heart to maintain the systemic blood pres- sure. She did well with the IABP. The aneurysm was successfully coiled.
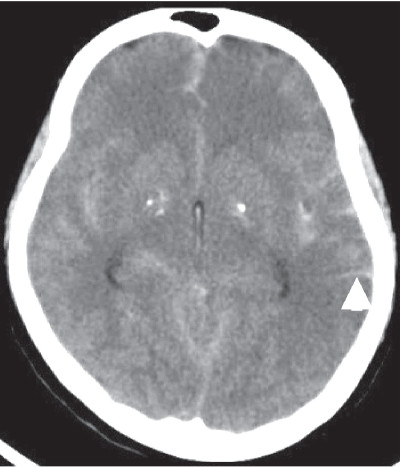
Figure 1: Subarachnoid hemorrhage in non contrast CT scan (see arrow head)
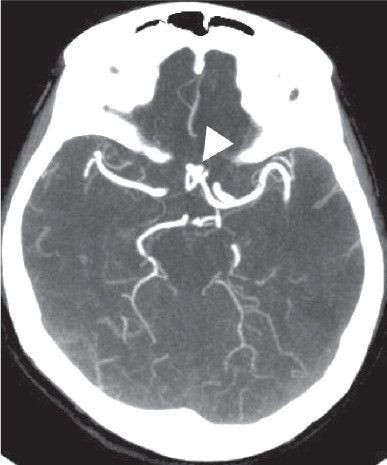
Figure 2: CTA shows anterior communicating artery aneurysm. (see arrow head )
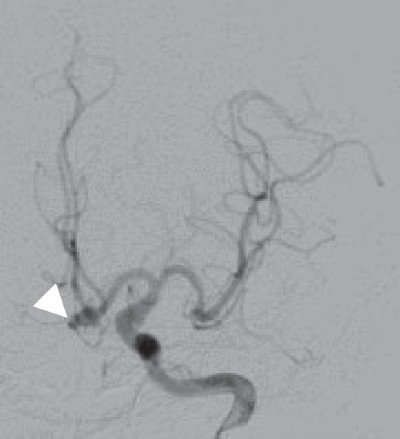
Figure 3: Left ICA angiogram shows anterior communicating artery aneurysm.(see arrow head)
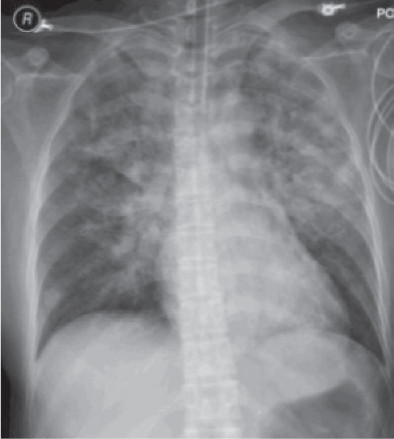
Figure 4: The Chest x-ray shows pulmonary edema
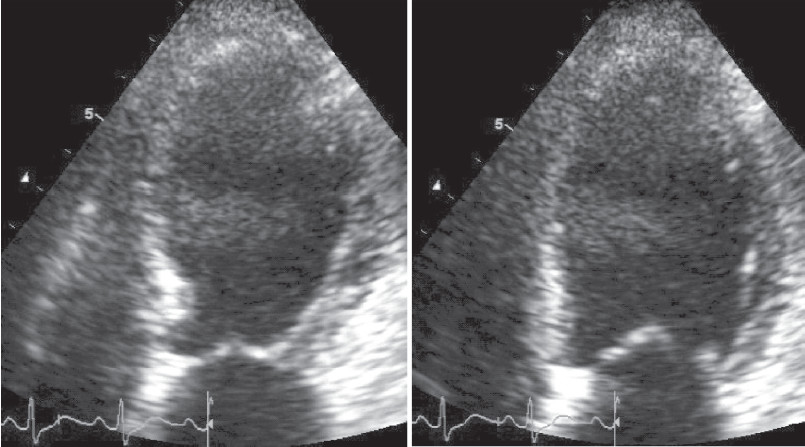
Figure 5: Echocardiograms show dilated left ventricle, poor left ventricular systolic function.
Although the mechanism of neuro-cardiac syndrome is not well understood, there have been many reported cases concerning this particular syndrome. The most well known syndrome is Takotsubo syndrome. The name Takotsubo originates from the shape of the left ventricle, which resembles a Japanese octopus-trapping pot.
The classic Takotsubo syndrome is characterized by transient, often severe left ventricular dysfunction and EKG changes that might mimic acute myocardial infarc- tion in the absence of significant obstructive coronary disease.4 Since being first described in 1991, there were more than 789 cases reported as of May 2008.4 Elderly women are most commonly affected.
We present cases of LV dysfunction in the intracere- bral hemorrhage and subarachnoid hemorrhage patients. The clinical findings of these patients were similar to Takotsubo syndrome. The EKG changes in our patients were non-specific ST-T changes. The cardiac enzyme did not change; therefore the coronary angiogram was not performed. However the echocardiogram revealed the LV dysfunction which spontaneously resolved. As for the first case, the recovery of the heart was evidenced at 6 months after initial echocardiogram. There was no period of systemic circulation problem during his admission.
The other case was more severe and quite complex.The patient suffered from a ruptured anterior communicating artery aneurysm and pulmonary edema. Her systemic blood pressure could not be maintained, despite inotropic drugs being maximally administered. The IABP was introduced to maintain her systemic blood pressure. In subarachnoid hemorrhage, the main ratio- nales of treatment are to avoid cerebral vasospasm and maintain cerebral perfusion pressure (CPP) which can be calculated by the subtraction of intracranial pressure (ICP) from mean arterial pressure (MAP) [CPP=MAP- ICP]. The options of treatment include triple-H therapy which consists of hypervolemia, hypertension, and hemodilution. In the patient with signs of congestive heart failure, the volume control is crucial. Accompanying the hypertensive goal, the IABP played more than one role for this particular patient.
Incidence and Demographics
The incidence of Takotsubo syndrome in intracerebral hemorrhage patients remains as yet unknown. 5 N. Banki, et al., in his large prospec-tive studies of LV dysfunction after SAH, reported 28% of 173 patients had evidence of regional LV dysfunction and 15% had global LV dysfunction, with an LVEF less than 50.6 However, due to its similarity to atherothrombosis-mediated acute coronary syndromes and its unfamiliar diagnosis, it is likely under-reported. The mean age of patients presenting with this syndrome is approximately 62–75 years of age.28 Approximately 85–100% of patients diagnosed with Takotsubo are women.
Pathophysiology
Although the mechanism of Takotsubo is unknown, several theories regarding the cause for this syndrome have been proposed. The relationship between stressful events and the onset of symptoms was observed in several reports. Increasing of catecholamines has been reported in many patients following Takotsubo cardio- myopathy. Elevated catecholamine levels have been shown to cause direct myocyte injury via an increase in intracellular calcium and oxygen-free radicals. This pathologic process is seen in catecholamine-induced cardiomyopathy (i.e., secondary to a pheochromocytoma) which histologically and morphologically results in abnormalities similar to Takotsubo.
It is hypothesized then that excessive activation of cardiac catecholamine receptors may be the origin of the cardiomyopathy.7,8,9 The unique distribution of sympathetic nerves and receptors on LV contributes to this hypothesis.10,11 The catecholamine receptors on left ventricle are composed of β1,β2 85%, and α1,α2 for the rest.3 This causes hypercontractility of the affected left ventricle. In addition, there is a possible loss of elasticity following extreme expansion together with the presence of a thinner layer of myocardium at the apex as compared to other regions of the LV.12 This explains why the syndrome affects the LV apex and result in apical ballooning. Direct myocyte toxicity due to calcium overload, microvascular dysfunction due to excessive catecholamines or primary metabolic abnor- malities are also possible mechanisms.4
Temporary occlusion of a variant left anterior de- scending (LAD) due to ruptured atherosclerotic plaque is another hypothesis.29 Although this coronary anatomy was not observed in all patients, it has been suggested as an alternative explanation in some cases.
The most common affected segments were the basal portions of the anteroseptal and anterior walls and the middle ventricular portions of the anteroseptal, infero- septal, anterior, and anterolateral walls.6
Clinical feature and diagnosis
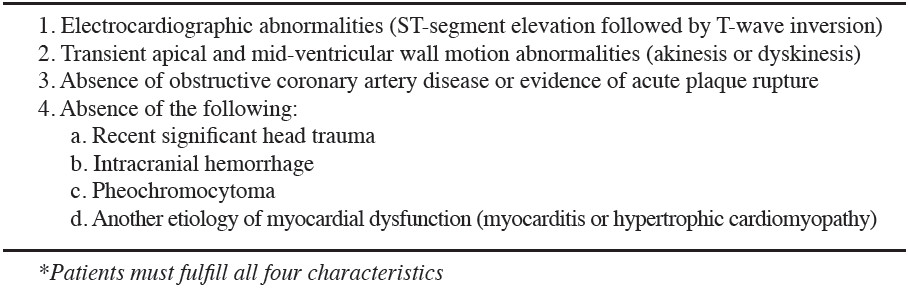
Patients often present with chest pain, and/or dyspnea, after suffering acute physical or emotional stress. Patients’ symptoms may range from mildly symp- tomatic to critically ill. Bybee et al. have proposed criteria for the diagnosis of this syndrome (Table 1)
Table 1: Proposed Mayo Criteria for the Diagnosis of Takotsubo Cardiomyopathy*14
Management
The management of Takotsubo syndrome is primarily empirical and should be individualized depending on the LV function. There is emerging data which supports the role of β-blocker, propanolol, in decreasing peak gradients in midventricular obstruction.12,13 β-blockers decrease LV contractility and increase the diastolic filling time which augmented LV end diastolic volume (EDV).14,15 In the patients with coronary artery vaso- spasm, dihydropyridine calcium channel blockers are recommended instead of β-blocker.14,16 Dobutamine is contraindicated in this kind of patient.16,17,18 Phenyleph- rine may represent an alternative approach in patients presenting with outflow tract obstruction and severe hypotension. In hemodynamically unstable patients, early administration of intra-aortic balloon pump coun- terpulsation should be considered.32
Generally, Takotsubo syndrome is a quite benign and self-limiting condition. But if systemic blood pressure cannot be maintained, Intra-Aortic Balloon Pump is an effective treatment option. In rare situations Takotsubo syndrome can progress into refractory cardiogenic shock with limited therapeutic options available. Bonacchi M, et al. reported their application of Extracorporeal life support in order to rest the heart, sustain circulation and end-organ perfusion. They concluded that ECLS might be the selected treatment and seems to be an effective and useful ultimate therapeutic strategy for preventing death.33
Management of Takotsubo syndrome after subarachnoid hemorrhage
In patients with subarachnoid hemorrhage who need hypervolemia and permissive hypertension, the low EF can reduce the cerebral perfusion and cause brain damage. Although the systemic blood pressure can remain in normal acceptable range, this patient group almost always needs a mild to moderate degree of hypertensio in order to treat the vasospasm. When Takotsubo syndrome occurs, even maximized inotropic agents could not raise the systemic blood pressure high enough to correct vasospasm.
The author used IABP in conjunction with inotropic agents in order to sustain circulation and promote potential ventricular recovery. The IABP can maintain the systemic blood pressure and allows additional space for volume infusion. As mentioned earlier, Takotsubo syndrome is a self-limiting condition, therefore within or two weeks, the patient will no longer need IABP.
Prognosis
Takotsubo syndrome does not cause permanent myocardial damage. Contrast enhanced MRI scan of heart shows no residual scaring, although there is severe residual regional wall dysfunction. In addition, the myocardial changes seen in myocardial biopsy are also completely normalized after functional recovery.19 Therefore the Takotsubo syndrome is generally a benign condition, mortality rate is less than 1% in hospitalized patients13,16 and recurrence rate is no more than 10%.31 Complete recovery of contractile function has been documented in nearly all cases and usually resolves within a few weeks.30 Only 5% of the patients with Takotsubo syndrome have the significant finding on coronary angiogram and rarely develop fulminant myocardial infarction (<1% of all acute myocardial infarction).20,21
Takotsubo cardiomyopathy differs from common cardiac dysfunction in its reversible nature. This charac- teristic must be taken into consideration when treating patients with intracerebral hemorrhage to avoid misclas- sification of the disease. Takotsubo syndrome is now a known complication in the severe neurological condition such as subarachnoid hemorrhage. Physicians taking care of these patients should become familiar with it. Both IABP and ECLS have a role in more severe scenarios or in the patient who needs systemic blood pressure augmentation such as vasospasm.