Serotonin syndrome is a state of serotonin toxicity in the human body.It occurs infrequently but can contribute to a serious and life-threatening illness.1-4 Serotonin syndrome is caused by increasing serotonergic activities in the body either from a single serotonergic drug adverse reaction, drug-to-drug interaction or some illnesses that can cause a high serotonin level such as carcinoid syndrome. Nowadays its incidence tends to increase because of the use of multiple-drug-regimen, growing number of serotonergic drugs available and more common use of serotonergic drugs, early recognition by the physician and prompt treatment is necessary to save patients.1-4
A 22-year-old female presented with fever and a runny nose, excessive sweating and worsening tremor in her limbs and head for 2 days. She had a history of learning disorders and a major depressive disorder. She noticed that these tremors started during the last month after a new medicine, agomelatine, was administered. Details of current medications were agomelatine (a melatonergic antidepressant, a melatonin receptors agonist and 5HT-2C receptor antagonist) 25 mg/day, sertraline 50 mg/day, lorazepam 1 mg/day, clonazepam 0.5 mg/day and methylphenidate 27 mg/day. Physical examination revealed temperature of 38.8 degrees celsius which went up to 39.4 degrees celsius after taking acetaminophen; heart rate was 110 beats per min, blood pressure 120/66 mmHg, and respiratory rate 20/min. There was mild pharyngeal injection on general physical examination. Mild agitation and inducible ocular myoclonus were noted on neurological examination. According to the inappropriate degree of fever, inducible myoclonus and history of concurrently using two serotonergic medications, diagnosis of serotonin syndrome was made. The treatments given were intravenous fluid, discontinuing causal drugs sertraline and agomelatine. Medications given were antibiotic, lorazepam, clonazepam, and an antidote cyproheptadine. Clinical features of serotonin toxicity significantly improved after titrating cyproheptadine from 4 mg every 8 hours to 8 mg every 8 hours.
Serotonin or5-Hydroxytryptamine is a biologic amine that is synthesized from the human body and functions as a neurotransmitter. Ninety percent of serotonin is synthesized at the periphery and ten percent is synthesized from the central nervous system (CNS). This small amount from the CNS is thought to be responsible for serotonin toxicity in humans.5,6 The word serotonin comes from two Latin words: serum and tonic. In 1948, it was found in platelets and acts as a vasoconstrictor substance. Serotonin was later found in many cells, including enterochromaffin cells of the gastrointestinal (GI) tract, brain, lungs, and kidneys. In the GI tract, it causes smooth muscle contraction. Circulating serotonin is stored in platelets and is responsible for hemostasis. Peripheral serotonin is associated with many diseases including migraine, irritable bowel syndrome and, systemic and pulmonary hypertension. In the central nervous system, it is a neurotransmitter that plays a role in controlling mood, behavior and sleep cycles.5,6
Tryptophan is a precursor of Serotonin. After being hydroxylated by specific tryptophan hydroxylase, it is changed into 5-HTP (5-hydroxytryptophan). Then 5-HTP is decarboxylated, by decarboxylase to become 5-HT (5-hydroxytryptamine) or serotonin. In the central nervous system, this process is found in pre-synaptic neurons in midbrain and pons.5-7 When neuronal depolarization occurs serotonin will be released into the synaptic space and bonded to post-synaptic serotonin receptors or will reuptake back to the presynaptic space as a negative feedback mechanism. In the presynaptic space most of the serotonin is metabolized by MAO-A (Monoamine oxidase-A) to 5-HIAA (5-Hydroxyindoleacetic acid) which will be rapidly excreted in urine.2, 5
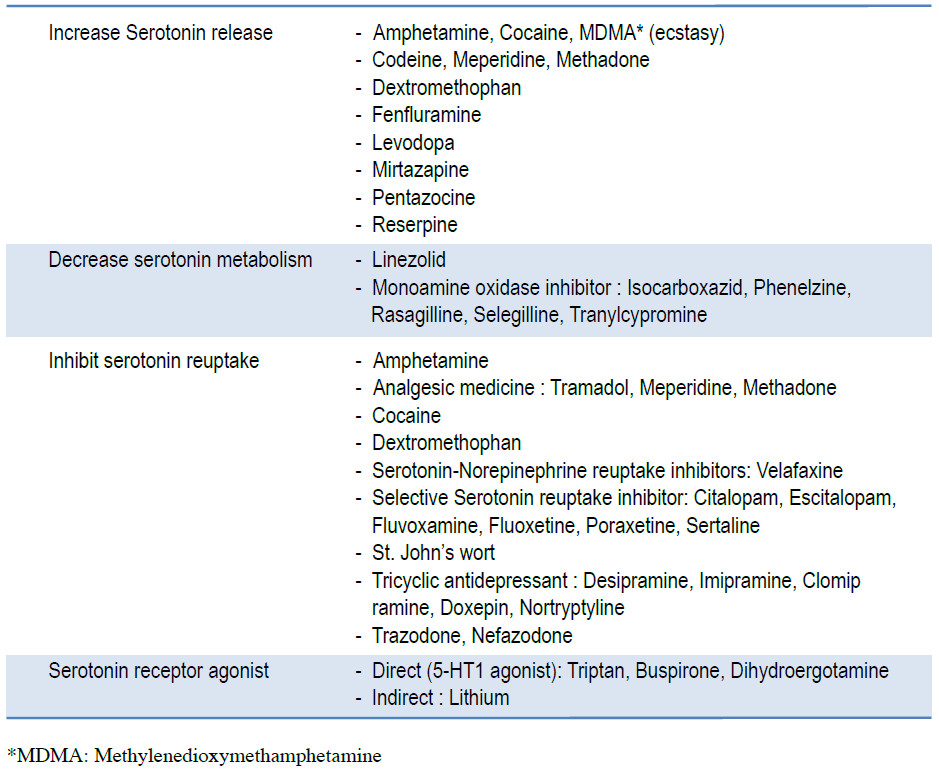
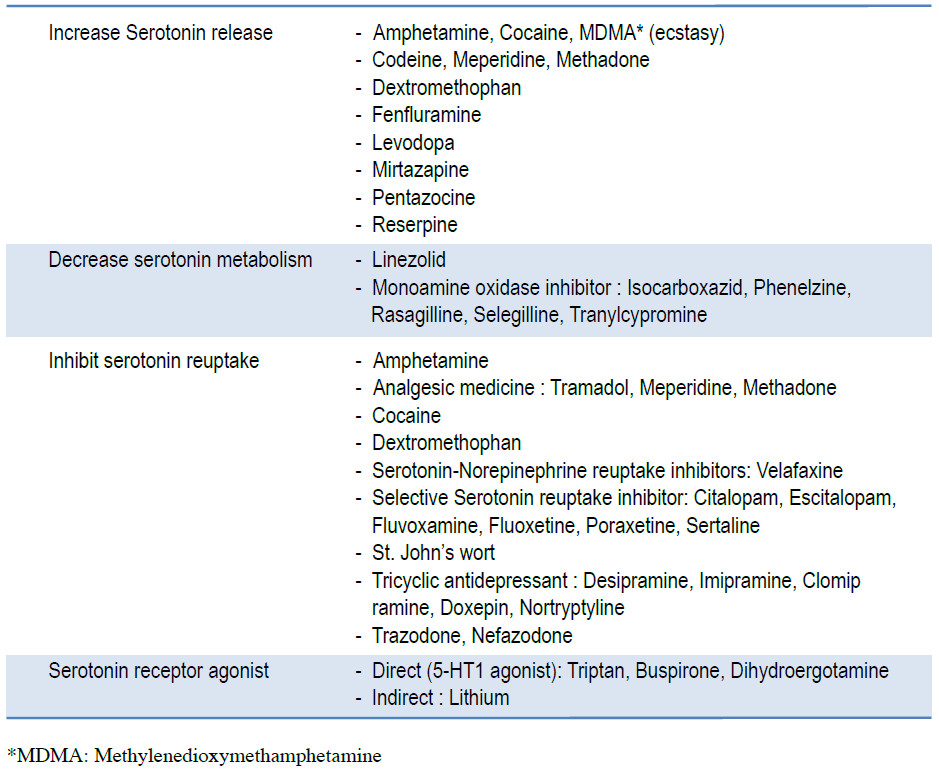
Most clinical manifestations occur from factors that interfere with serotonin transport, binding or metabolism and causing abnormally high serotonin level.5 Serotonin toxicity appears to be a dose related response, unlike neuroleptic malignant syndrome that is idiosyncratic.6 In a major proportion of cases, Serotonin syndrome has been caused from drug-to-drug interaction. But patients with renal or liver disease and patients with Cytochrome CYP 2D6 deficiency can be at risk of serotonin intoxication from single drug use. 2,5,6 Drugs that cause increased serotonin levels are divided into 4 groups according to their mechanisms of action which are: increased serotonin production and release, decreasing serotonin metabolism and decreasing serotonin reuptake1,2,5 and serotonin receptor agonist action (Table 1).1, 2
Table 1 : Medications that can cause increasing serotonin activity
Clinical presentations of serotonin syndrome consist of autonomic changes with abnormal mental status findings and abnormal neurologic findings.1,2 In mild cases the onset can be subacute or chronic.1,2,8 In severe forms, clinical onset tends to be acute within 6-8 hours following the increase in serotonin levels. Findings on physical examination differ, depending on the severity of disease.1,2
Clinical manifestations in mild cases can be non-specific such as tachycardia, shivering, mydriasis and diaphoresis. In these cases, hyperreflexia and myoclonus may be the only positive findings on neurological examination.2,4,8 Other non-specific symptoms that can be found in serotonin syndrome are dizziness, generalized body pain, nausea, insomnia and restlessness.8
In moderately severe cases, high blood pressure and high temperature can be found accompanying with increased bowel sounds, hyperreflexia that is greater on lower extremities, ocular myoclonus, altered mental status (for example, pressured speech, mild agitation, hypervigilance, easily startled) and peculiar head turning behavior.2, 4
In moderately severe cases, high blood pressure and high temperature can be found accompanying with increased bowel sounds, hyperreflexia that is greater on lower extremities, ocular myoclonus, altered mental status (for example, pressured speech, mild agitation, hypervigilance, easily startled) and peculiar head turning behavior.2, 4
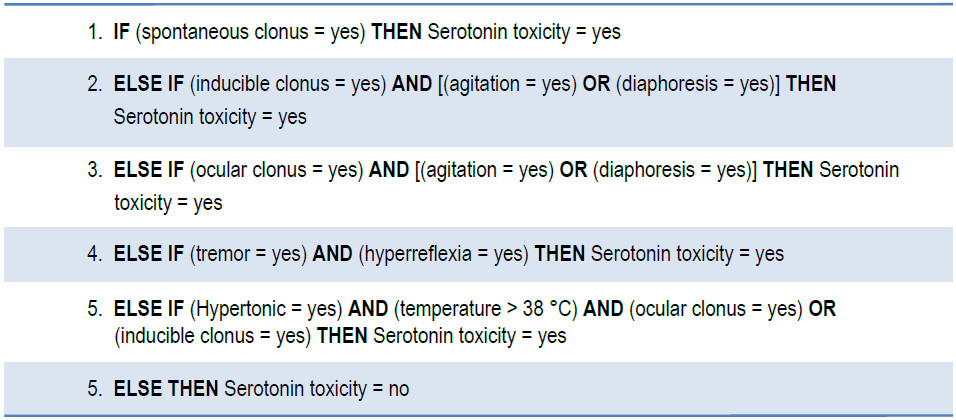
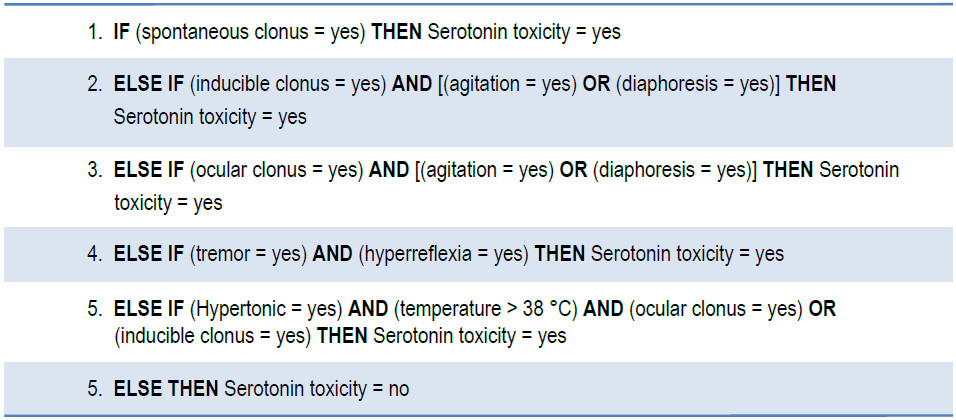
A serotonin syndrome diagnosis criterion was first proposed by Harvey Sternbach in 1991. After many revisions, the Hunter serotonin toxicity criterion (Table 2) was developed by Dunkley et al.1 in 2003 and is currently used to help the diagnosis of serotonin syndrome with 84% sensitivity and 97% specificity.
The mortality rate of patients with serotonin syndrome is between 2-12%.6 To date, there have been no specific randomized controlled trials or treatment guidelines for the treatment of serotonin syndrome. The most important course of treatment is to discontinue all offending drugs.2,5 However supportive care including intravenous fluid, treatment of hyperthermia and administering muscle relaxant are also important.5,6
Most patients showed significant improvement after withholding the causative agents but the time to clinical recovery varies depending on the half-life of those specific agents.4,5 In mild cases, supportive treatments along with giving benzodiazepine and discontinuing offending medicine are sufficient.2,3,5,8
In more serious cases, increased muscle tone caused increased core temperature. Treatment of the fever by using only anti-pyretic medicine such as acetaminophen would not decrease body temperature.7 In these cases muscle relaxants such as benzodiazepine is the sole treatment.6,7 Other supportive treatments to lower body temperature are cool intravenous saline and cool blankets. In severe cases when the patient’s core temperature was more than ∞C, intubation with sedation and induction of muscle paralysis are indicated.2,4,6 Physical restraints should be avoided because they can lead to increased muscle tone, increased hyperthermia and worsening lactic acidosis and rhabdomyolysis.4,6
Some medicines are considered to be antidotes such as antagonists to 5-HT1 and 5-HT2 receptors. Cyprohepta dine is a first generation histamine-1 receptor antagonist with non-specific antagonist at 5-HT1A and 5HT2A receptor.5 Dose recommendations for cyproheptadineis oral loading 8-12 mg then 2 mg peroral every 2 hours in severe cases, and 8 mg peroral every 6 hours in mild to moderately severe cases (32-36 mg/day).1-2 Sublingual olanzapine and intramuscular chlorpromazine are both antipsychotics that were reported to be effective.2,4,5,7 But both of them can also lower the seizure threshold.4,7 Chlorpromazine has a long half-life and has the potential to induce hypotension; it may have a possible role only when cyproheptadine could not provide adequate clinical response.2, 4 Chlorpromazine should not be used in patients who are already hypotensive.4
In patients with severe hypertension, the suitable anti-hypertensive medicine should be short acting because the blood pressure would be lower spontaneously after serotonergic activity decreases.2, 4, 6
We report a case of serotonin syndrome who presented concurrently with acute respiratory tract infection. In general practice, serotonin syndrome itself can be overlooked easily because the presenting symptoms can be non-specific. It should be suspected in all patients who currently receive serotonergic medicines and had either new medical or new neurological symptoms. Prompt recognition, withdrawal of precipitating agents and both specific and supportive treatments are essential.
Serotonin syndrome results from an adverse reaction to medicines that have serotonergic effect and can also result from drug-to-drug interaction. In this case, the timing of the onset started after the second serotonergic agent had been added. Patient safety is a priority and one drawback of additional serotonergic agents can lead to serotonin syndrome. Therefore the physician should be cautious when prescribing multiple medicines that have a serotonergic effect and these medications should only be administered when absolutely necessary.
Table 2: Hunter Serotonin Toxicity Criteria: Decision Rules In the presence of a serotonergic agent: