The proximal humeral fracture is common and is the third most prevalent fracture after hip and distal radius fractures in patients aged over 65.1 Historically, the conservative treatment of this type of fracture is satisfactory in 80% of cases,2 but the rate of complications such as displaced tuberosity fragments, malunion, nonunion and avascular necrosis (AVN) of the humeral head3,4 increases, depending on the complexity of fracture, energy of trauma and soft-tissue njury.5
Different techniques have been described for surgical treatment of commi- nuted displaced proximal humeral fractures, including suturing, cerclage wiring, K-wires fixation, screws, plates, intramedullary fixation, and shoulder arthroplasty.6,7 In the past decade open reduction and internal fixation with angular stable anatomical plate and locking head screws is one of the methods that provides adequate stability, early rehabilitation and good clinical outcomes. Various studies have suggested that the implants have been suggested to have more reliable fixation in osteoporotic bone with primary stability.8,9 However, the associated complications remains high (over 10-49 %).10 This including varus malunion 33%, reoperation rate 14%, AVN 10%, screw perforation of humeral head 8%. Many of those complications were related to the intraoperative procedures.11-13
To reduce complications related to intraoperative techniques,a surgeon has to follow the principles of reduction and fixation, and this is already well known and recommended. Good preoperative planning and performing a stepwise operation helps each step in sequence to be completed successfully before the next one is undertaken. This will ensure that the proper techniques have been applied from start to finish.
The purpose of this study was to present a retrospective evaluation of the clinical outcomes and radiologic outcomes of 30 fractures of the proximal humerus after being treated with open reduction and internal fixation with the Proximal Humeral Internal Locking System (Philos) plate and importantly to guide and recommend the 6 stepwise intraoperative criteria described below in moredetail which has been developed and used in all the study cases.
This study retrospectively reviewed all 2, 3, and 4-part proximal humeral fractures that were consecutively treated with our 6 stepwise intraoperative criteria for reduction and fixation with locking plate, between January 2012 to December 2015 at a Level 1 and a Level 2 trauma center. The operations were done by one orthopedic trauma surgeon. Inclusion criteria were all patients aged over 18 years old who had 2, 3 and 4-part fractures according to Neer’s criteria of classification for proximal humeral fracture with displacement of each fragment more than 1 centimeter or angulation of the fragment more than 45 degrees.We excluded open fractures, polytrauma patients, segmental fractures, injuries with diaphyseal extension, and patients with less than 12 months of clinical follow-up.
Preoperative imaging consisted of orthogonal radio- graphic views, AP and Lateral, CT scan of the shoulder and perioperative fluoroscopic evaluation of all patients before performing open reduction and internal fixation. According to Neer’s Classification, fractures were 2-part in 13 (43%), 3-part in 12 (40%), and 4-part in 5 (17%).
Postoperative evaluation consisted of assessment through patient interview and questionnaire, physical examination which included routine assessment, active range of motion and clinical assessment of anterior branch of the axillary nerve for muscle weakness. Functional outcomes were assessed using Constant score and graded as poor (0–55 points), moderate (56–70), good (71–85), or excellent (86–100).
Postoperative radiographic analysis was standard orthogonal radiographs obtained during routine follow-up at 2, 6, 12, 24, and 52 weeks. Preoperative and postoperative radiographs were retrospectively analyzed in a serial fashion by an independent observer to evaluate fracture union, time to union, fracture alignment, head shaft angle in AP, and lateral and secondary loss of reduction. The humeral head-to-shaft angle (Figure 1) was an angle of the head axis (a line drawn through the apex of the humeral head which was perpendicular to anatomical neck) and humeral axis. This was measured using viewing software, Picture Archiving and Communication Systems software (PACS). The angles were further categorized as major varus (155 degrees). Observation of avascular necrosis, posttraumatic arthrosis, and hardware-related complications was also recorded.
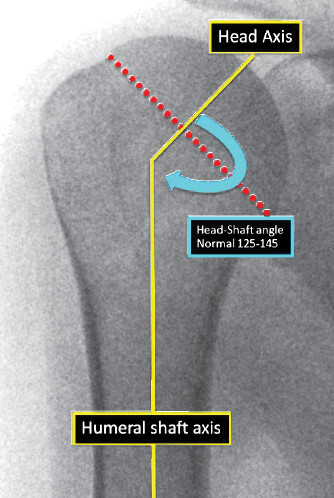
Figure 1: Head-Shaft angle is formed by drawing a perpendicular line of the head axis and shaft axis.
Patients were in a supine position on a radiolucent table and orthogonal fluoroscopic images were obtained before the surgical operation to ensure adequate radiographic visualization intraoperatively. The C-arm was positioned and approached from the opposite side

Figure 2: Demonstrates the C-Arm setting from the other side of the operating table, opposite to the fracture side.
(Figure 2). True AP view was assessed by simple antero- posterior projection and lateral view was obtained by manipulation of the head fragment after temporary fixation was applied. The implants were PHILOS plates (Synthes, Switzerland). Open reduction and internal fixation was performed on all 30 patients using same operative technique which followed standard principles.A standard delto-pectoral approach was used to expose the fracture area without detachment of periosteum and any rotator cuff attachment. After identification of the humeral head, biceps tendon, greater tuberosity and lessor tuberosity, the operation was performed step by step with our 6 stepwise intraoperative criteria as follows:
Reduction and fixation of head fragments
Plate positioning with the humeral head
Fixation the proximal part of the plate to the humeral head
Correct placement of the plate to the humeral shaft
Fixation the shaft to the side plate
Secure the sutures of the cuff to the plate
Procedures of 6 stepwise are described as follows:
1. Reduction and fixation of the head
The humeral head, greater and lesser tuberosity fragments were mobilized by placing a non-absorbable (No. 2 Fiber Wire) suture through the rotator cuff tendon adjacent to the tuberosity fragments. The sutures were used to manipulate and reduce the tuberosities to the humeral head fragment (Figure 1A). The fragments were fixed together with K-wires to form a normal configuration of the humerus head under true AP fluoroscopic image which is easily recognized as a familiar beetle car appearance (Figure 1B). If necessary all the sutures could be tied up together to maintain the reduction of the humeral head fragments before K-wire fixation (Figure 1C).
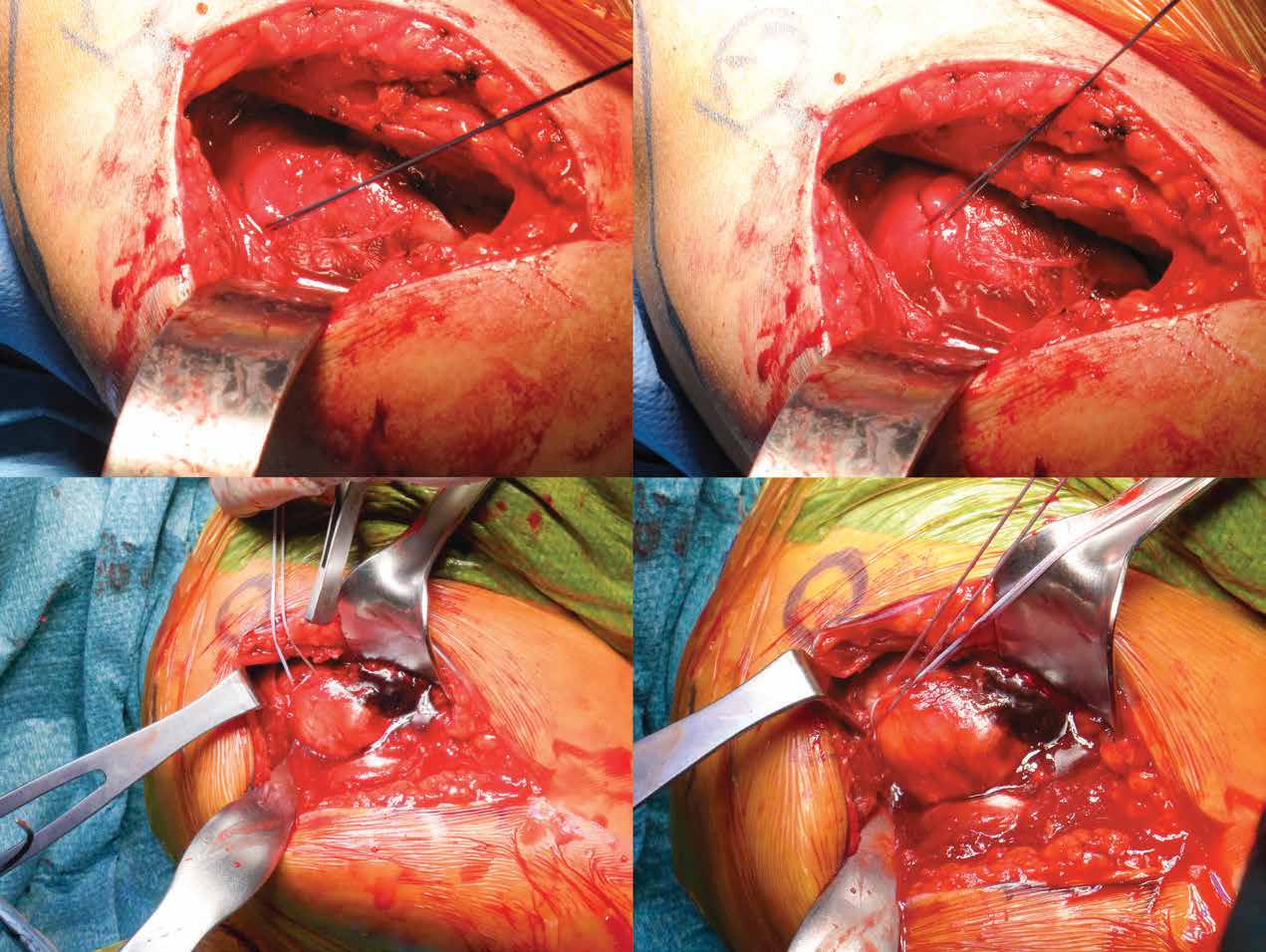
Figure 1A: Shows suturing of the displaced fragments of the humeral head with non-absorbable suture material. The sutures were passed into the tendon attachment of greater tuberosity, and lesser tuberosity, as required to pull and mobilize the fragments for reduction. If necessary these sutures can be tied up together to keep the reduction before plate application.
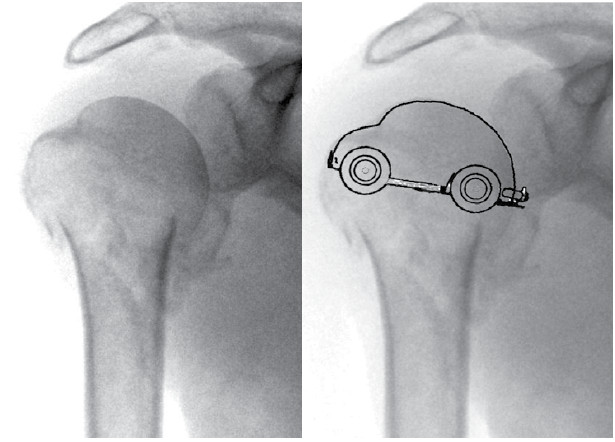
Figure 1B: The humeral head was reduced by pulling of sutures and tying all sutures together to form a “beetle car” appearance in true AP of fluoroscopic view.
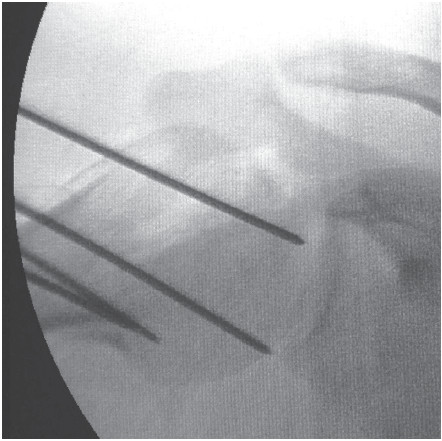
Figure 1C: The reduction can be facilitated by abduction of the shoulder to release the tension of deforming forces, sutures are placed to aid reduction and K-wires are fixed provisionally before plate application.
2.Plate positioning with the humerus head
The plate was positioned on the lateral surface of the head, the upper end of the plates were placed about 5-8 mm. inferior to the upper end of the greater tuberosity and the plate anterior surface is 5 mm. lateral to the bicipital groove (Figure 2A). The proper positioning was confirmed by direct visualization and fluoroscopic AP image which showed true lateral profile of the plate while the head shows the “beetle car appearance” (Figure 2B). The fluoroscopic lateral image is also used to confirm that the plate is placed on the center of the head (Figure 2C).
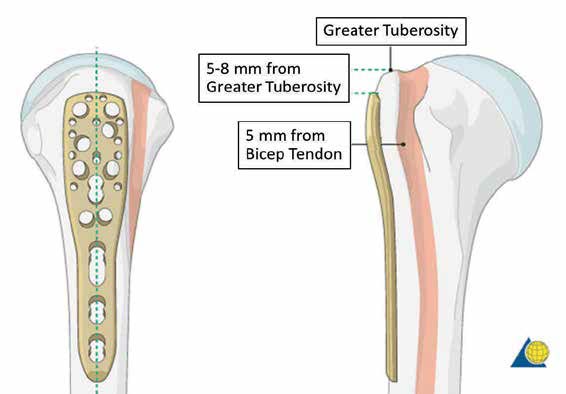
Figure 2A: Recommended PHILOS plate positioning from AO.
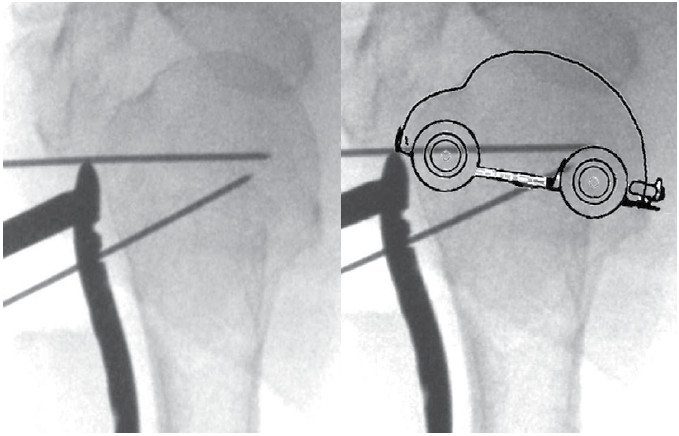
Figure 2B: The true fluoroscopic AP view shows the beetle car appearance,and the plate has to be positioned in such a way to show the “True lateral profile the plate” while the most proximal tip of the plate is 5-8 mm inferior to the greater tuberosity tip.
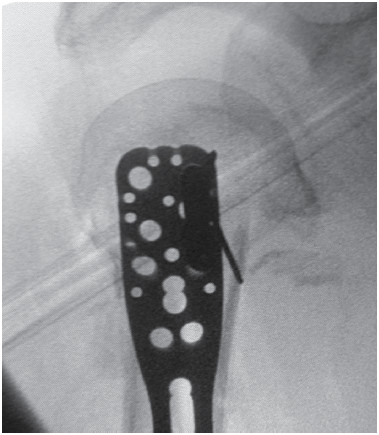
Figure 2C: In lateral view shows the plate is placed on the center of the head.
Three important fluoroscopic image findings required prior moving to the next step are
(I) “Beetle car appearance” of humeral head in AP view,
(II) True lateral profile of the plate in AP view and
(III) the proximl part of the plate lies in the center of the head without deviation in lateral view.
3.Fixation the proximal part of the plate to the humeral head
Once Step 1 and Step 2 are performed and completed correctly and confirmed with the C-arm as described, the plate is fixed to the humeral head by a few K-wires or locking head screws to stabilize the plate to the humeral head (Figure 3).
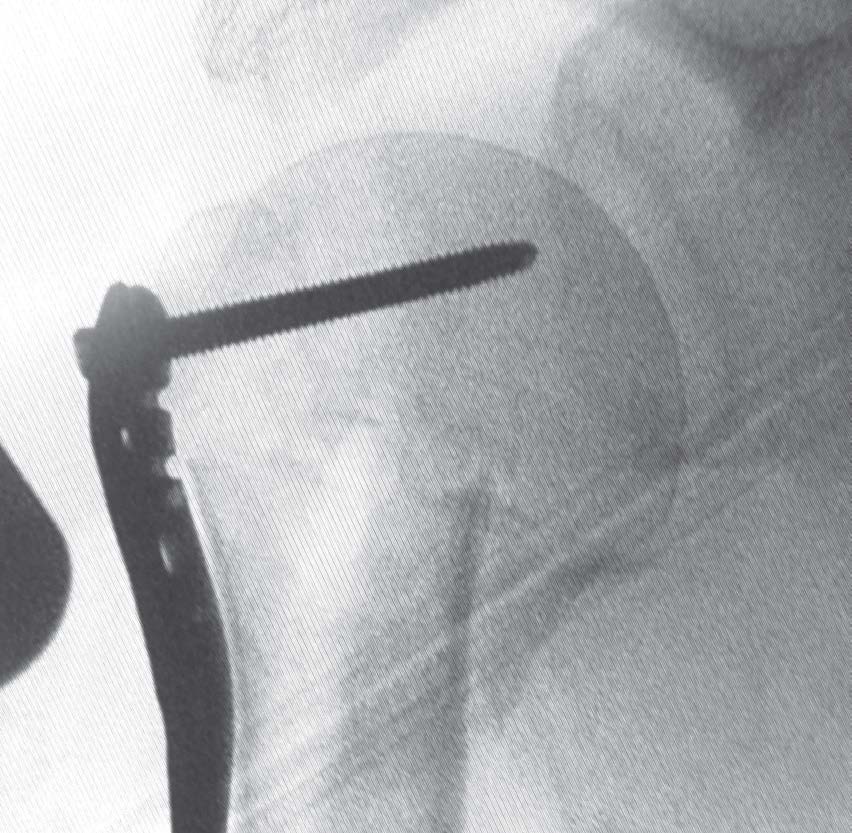
Figure 3: The humeral head is fixed by K-wires and some locking head screws prior to reduction and fixation of the shaft.
4.Correct placement of the plate to the humeral shaft
The humeral shaft is reduced to fit the plate, as the aim is to form a normal head shaft angle in fluoroscopic AP view (Figure 4A) and to position the plate parallel to the shaft in the lateral view (Figure 4B-4C).
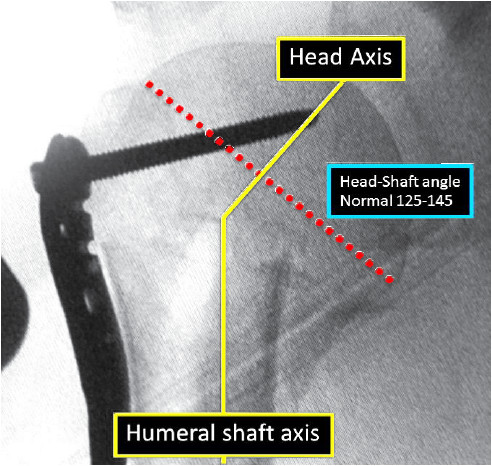
Figure 4A: Demonstration of measurement of Head-Shaft angle in AP view after reduction.
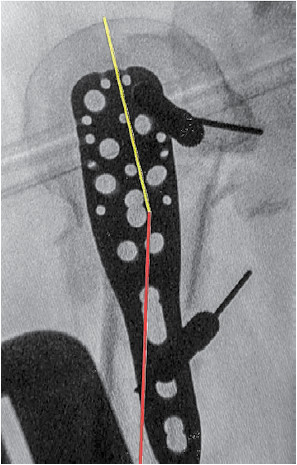
Figure 4B: Shows true lateral view of proximal humerus before correction of anterior fracture angulation. In this view the distal part of the plate is not parallel to the shaft.

Figure 4C: Shows after correction of anterior angulation of head shaft fragments by simple manipulation, the whole length of the plate is parallel to shaft.
5.Fixation the shaft to the side plate
This can be performed provisionally with a conven- tional screw to pull the shaft to the plate by using the plate as a reduction template (Figure 5A). Although there is a high threshold for accepting some rotational deformity of the upper arm when compared to the lower extremity, rotational misalignment remains a complication that may occur during surgery. Intraoperative assessment of humeral rotation may help surgeons obtain the correct rotational alignment. In uncomplicated fractures, several anatomic landmarks can be used as references such as the bicipital groove, the crest of the greater tuberosity, and the margins of the greater and lesser tuberosities. However, this is difficult during surgery in complex fractures. Correct rotational alignment assessment is helpful by intraoperative clinical examination which shows approximately 10 - 15 degrees of arm external rotation while under fluoroscopy, the humeral head shows true AP, the “beetle car appearance”, view. The conventional bicortical screw, then, can be inserted to fix the shaft. Intraoperatively, the rotation can be assessed by bringing the injured arm across the chest in internal rotation with 90 degrees of elbow flexion and allow 20 degrees of external rotation which is acceptable.
After completing 5 steps of the procedure, all additional locking head screws can be fixed in the head fragment, and the most important screws will be the calcar screws which support the medial head fragment to prevent varus collapse. In general, if the plate position at the humeral head is corrected, it is possible to fix the plate with calcar screws. The shaft can be fixed further with 2 to 3 more cortical or locking head screws depending on bone quality (Figure 5B).

Figure 5A: One cortical screw is fixed to the shaft and plate after rotational alignment has been assessed and corrected. Then the screw will keep the plate in the correct position before the placement of locking head screws.
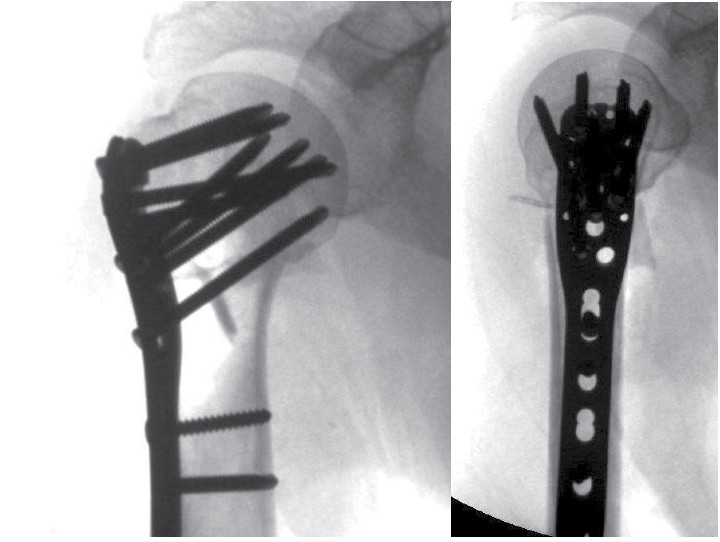
Figure 5B: Plate fixation in AP with good head shaft axis. Plate is placed parallel and along the shaft in lateral view.
6.Secure the sutures of the cuff to the plate
This is an important step to prevent any deforming forces from the head fragment and to maintain the reduction effectively, especially in osteoporotic bone (Figure 6A).
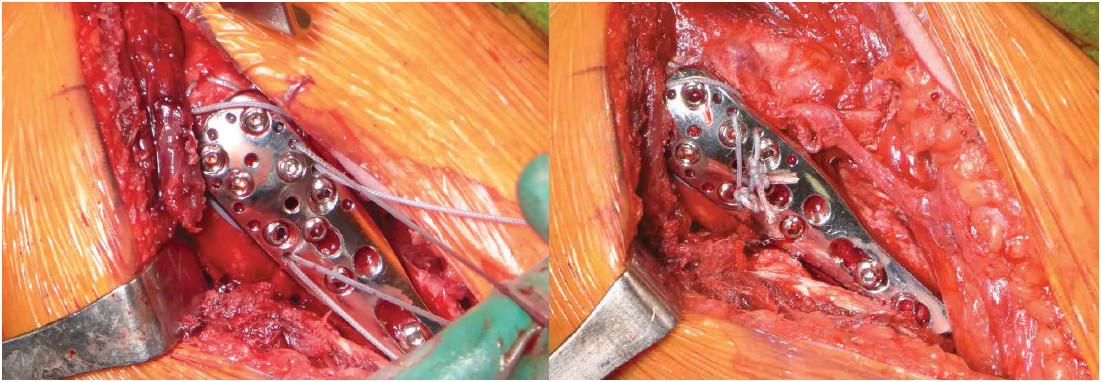
Figure 6A: Final step of attaching the cuff sutures to the plate holes to reinforce the fixation construction.
The postoperative regimen consisted of wearing an arm sling and starting active-assistive range of motion of the shoulder depending on the complexity of the condition,bone quality and stability of the whole construction. The skin sutures are removed at 2 weeks. Elbow, wrist and hand motion are encouraged initially.
 Figure 7: Final results after 12 months of follow up.
Figure 7: Final results after 12 months of follow up.
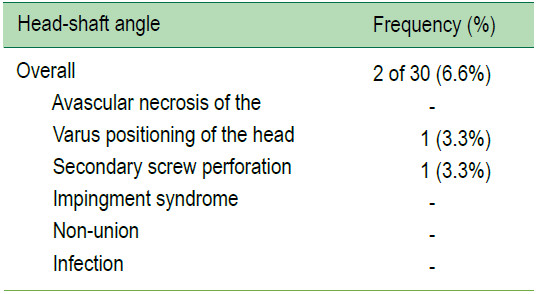
From January 2012 to December 2015, there were a total of 30 patients, 12 males and 18 females who met the criteria and underwent surgery. Average age was 51.7 years. According to Neer Classification, 43% (13) was 2-part fracture, 40% (12) 3-part and 17% (5) 4-part (Figure. A). Mean Constant scores at final follow up was 84, 47% (14) excellent, 37% (11) good, 13% (4) moderate, 3% (1) poor (Figure. B). A comparison of head shaft angle at immediate post-operatively with final follow up, 73%(22) was in normal range between 125-145 degrees which 1 case had secondary change into minor varus,17%(5) minor varus initially, 3%(1) minor valgus, 7% (2) major valgus (Table 1). The overall rate of complication was 6.6% in 2 cases, 1 case had secondary varus and 1 case had secondary screw perforation due to fracture axial displacement which resulted in limitation of range of motion of the shoulders (Table 2).Both these cases presented with severe osteoporosis with 4-part fractures even though all screws were stabilized into the head. There was no impingement of the acromion, no infection and all fractures were united. There was no avascular necrosis of the humeral head detected at the one year follow up.
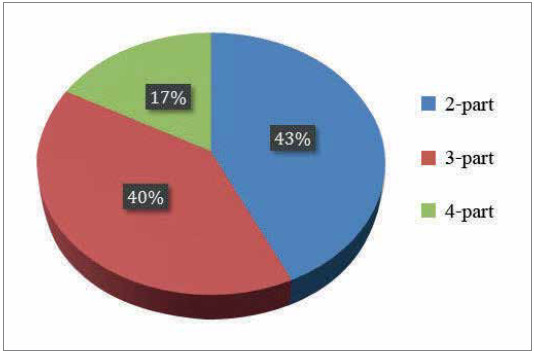
Figure A: Classification offracture type.
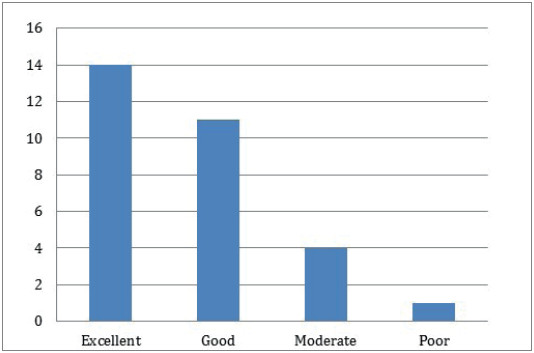
Figure A: Constant score result.
Table 1: Number of cases comparing Head-Shaft angle between immediate post-operative phase and final follow up.
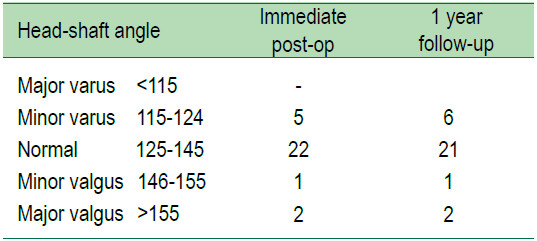
Table 2: Overall complications.
This study showed the functional and radiological outcomes of open reduction and fixation of displaced proximal humeral fracture with anatomical locking com- pression plate using 6 stepwise operative procedures. The finding of this study revealed reasonable good to excellent outcomes with low complications, thus the 6 stepwise surgical procedure is strongly recommended for surgeon. Furthermore, the procedures should be followed strictly in the correct order as a surgical strategy to prevent the complication of operative technique with internal fixation of the difficult proximal humeral fracture.
Although adopting the anatomical locking plates procedure revealed positive outcomes, the method is still debatable.Several studies describe a variety of surgical technique and implants to treat this complex fracture.14-19 Even though the anatomical locking plate is an efficient implant for proximal humerus fracture, there are report of surgical complications.20,24 According to Ruchholtz, 40% of complications are caused by in correct surgical techniques and complication rates are dependent on the surgeons’ expertise.20-22
These complications associated with the surgery included malalignment, subacromial impingements, screw penetration, malunions, tuberosity resorptions, AVN of the humeral head, and screw breakage. Several recent studies confirm that incorrect anatomical reduction is the strong predictor for failure as well as inappropriate position of the implant in relation to the proximal humerus.10,23-25 On this note, the intrinsic stability by proper reduction of the fracture is essential in order to prevent failure. Varus malreduction increases the effective lever arm of the rotator cuff which results in additional varus torque and high stress at the tip of the locking screws or pins.23 Anatomical reduction of the head with respect to the shaft reduces varus torque. Sagittal plane alignment can be compensated by shoulder motion, however in malalignment, the anatomical locking plate cannot be positioned correctly, and screws may be fixed eccentrically to the cortex and may result in unstable fixation or periimplant fracture. Some studies suggested the projection of the crest of lesser tuberosity in plain radiographs to be an important and useful landmark to assess humeral head rotation.26 In 3 or 4 parts fracture, anatomical landmark of proximal humerus, the bicipital tendon groove, ridge or lesser tuberosity may not be intact and be difficult to use as a landmark to determine rotation. This also probably causes rotational malalignment and malfunction. These 6 stepwise intraoperative criteria was designed to address these technical errors of practicing surgeons. The 6 stepwise operative procedures reflex well preoperative planning for common pattern of fracture of this part. All surgical steps effect each other especially the reduction of main fragment and implant positioning of specifically designed anatomical plate. The 6 stepwise starts with humeral head reduction, how to restore the fragments anatomically and evaluate the quality of reduction correctly. The configuration of familiar image of “beetle car” appearance is a helpful guide to determine correct AP projection of the proximal humerus. This step of reduction and maintain humeral head fragments using simple and well known technique of suturing and K-wires fixation. The second step is to assure that plate positioning is optimum to fix to the head which will determine the head-shaft angle in AP and lateral view in the following steps. After fixation of the plate to the head in step three, the fourth step will be reduction and positioning of the shaft to the well aligned plate and head fragment, these include sagittal, coronal and rotational alignment of the whole construction before fixation of the shaft with provisionally cortical screws in step five before complete fixation. Step six is the last step of securing the rotator cuff to the plate which will reduce the varus deforming forces of the humeral head. All of the procedures are standard procedures but doing in stepwise fashion helps easing surgical procedures and in this retrospective study showed that most of the patient (83%) had well to excellent result for Constant scores. The overall complications at final follow up were low (6.6%) which included 4-part fracture with severe osteoporotic ending with further varus and screw penetration.