Pyogenic sacroiliac arthritis is a rare entity, and most cases are caused by Staphylococcus aureus. Usually, there are underlying diseases presenting, and in healthy persons it can occur in cases involving sport, over exercise, bike riding and running so on. Laboratory findings and imaging investigation is essential given the mild symptoms presenting for instant fever, and back pain. CT guide for aspiration, culture and sensitivity tests as well as appropriate antibiotics are recommended. This presentation is a case report as an example.
A 16-year old man, with no underlying disease presented with a history of pain in the left buttock for 2 months. He developed low grade fever and mild left gluteal pain. He was treated with non-steroid anti-inflammatory drugs (NSAID) but did not improve after 2 weeks. He felt more pain and was admitted to hospital. MRI of pelvis revealed evidence of left sacroititis with abscesses collecting at the left ileopsoas muscles. The abscess was drained under guided CT. Pus culture grew Staphylococcus aureus. It was susceptible to all tested antibiotics. The patient was treated with an unknown antibiotic for two weeks before travelling to Bangkok Hospital for a second opinion. The physical findings: he was febrile, with moderate pain at the left sacral area. Laboratory findings revealed a total WBC 3,590 cell/mm3 with Neutrophil 59%, Lymphocyte 34%, ESR 1 hour 71 mm. C-reactive protein was 2.96 mg/L. The plain film of the pelvic bone was unremarkable (Figure 1). No evidence of bone destruction was detected. CT of pelvis revealed bony erosion at subchondral region at left sacroiliac joint with residual abscess collection at left iliacus muscle (Figure 2).
He was treated with intravenous Cloxacilin for 2 weeks. The patient clinically improved. No fever was observed and he was able to walk with minimal pain at left pelvic girdle. He was discharged from the hospital with an oral antibiotic for up to 3 months.

Figure 1: Radiographic image AP of pelvis is unremarkable, no evidence of bone destruction or pelvic soft tissue mass is seen. Both sacroiliac joints appear intact.
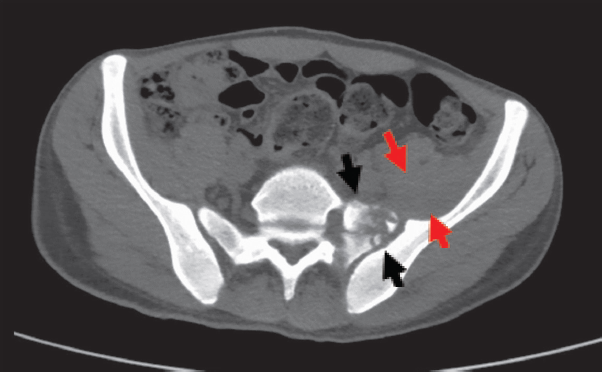
Figure 2: CT scan of pelvis, axial section reveals bony erosion at subchondral region at left sacroiliac joint (black arrows) associated with enlarged left iliacus muscle (red arrows). Small bone fragments are demonstrated.
Pyogenic septic arthritis of sacroiliac joint is a rare disease. Only 1-2 % of all septic arthritis are found.1 More than 50% have underlying diseases for instance trauma, immune deficiency, psoriasis, rheumatoid arthritis, intravenous drug abuse, septicemia, pelvic inflammation, post acupuncture,2 pregnancy. It occurs most frequently in children and adolescents.3,4 In healthy persons it presents in those involved in sports choices caused by over exercise, by riding a bicycle (bike), or by running etc. Most cases are delayed in their diagnosis because of a lack of specific symptoms. Common symptoms are fever, pain at lower back, gluteal, hip, or posterior thigh pain. The misleading diagnosis is sciatica, prolapsed disk or spondylolisthesis. The radiographic findings are normal in the early phase. CT with contrast enhancement demonstrating bone destruction at sacroiliac joints. Multiloculated abscesses collection at nearby muscles such as ileopsoas, obturator internus muscles might be demonstrated. MRI findings are the most sensitive test and more specific diagnosis by showing early cartilage damage (T1W low signal within subchondral bone, T2W high signal at perisynovial edema, synovial enhancement on Gd study).5 Staphylococcus aureus is the most common causative organism.6 CT guided needle aspiration and pus culture are recommended. Clinical improvement is observed with adequate drainage and appropriate antibiotic treatment usually up to 3 months. Role of surgical drainage intervenes when no clinical improvement shows within 48 hours after initial antibiotic treatment. H Ahmed et al.,7 described the flowchart of the surgical treatment pathway in case of acute or chronic sacroiliitis form including debridement and or arthrodesis.
A case of pyogenic sacroiliac arthritis caused by Staphylococcus aureus. Occurrence in healthy person with fever, left back pain and partially treated with antibiotic. He had missed lead of up to 2 months. Routine imaging investigations plain film of pelvis might have no benefit, CT and/or MRI with Gd enhancement are recommended. CT guided needle aspiration for bacterial culture and sensitivity test for appropriate antibiotics is essential.