Cardiovascular diseases (CVD) i.e. ACS, stroke, remainsthe number one killer of people worldwide. In 2016, anestimated 17.9 million people died from CVDs,accounting for 31% of the global deaths. Of these deaths, 85%were from heart attack and stroke.1 In Thailand, a report fromthe Ministry of Public Health indicated a higher morbidity andmortality due to CVD more than the past. From 2007-2014, ourrate of morbidity from ischemic heart disease (CAD) and strokeincreased 24% and 41% respectively.2 The mortality of CADrose from 21.3 to 28.9:100,000 (2008-2014) and the stroke deathrate increased from 20.8 to 31.7:100,00 (2008-2012).2,3 Since2015, CVD has become the leading cause of death, in aboutone-third, of Thai military officers.4 With no effective prevention,it could compromise future military missions. However, therecently published 10-yr cohort study suggested that predictionand prevention of future CVD events in asymptomatic caseswas feasible.5 By using a screening tool, the modified CoronaryRisk Chart (mCRC), available at http://caprecvdrisk.com/CVDRiskScore/5, allowed for the high (> 20%) predicted CVD riskofficers to be identified, treated early and their subsequent CVDevents have been reduced.5 At the same time, failure in riskreduction also led to the worst outcomes. Most ACS (100%) orstroke (72.5%) cases developed clinical events after sustainingtheir high risk status for three consecutive years.5 It remainedunknown why these high risk officers, who received groupeducation for life style modification and free of charge medication,still failed to improve their CVD risk. Thus, our study intendedto explore the etiology of risk reduction failure. By correctingthe cause, they might be saved from future catastrophic events.We also believed that their spouses could be the strongfacilitators for creating a healthy environment at home so theFamily Partnership Intervention Program (FPIP) was created.The result of the FPIP was studied at the end of 8 weeks.
The study was divided in two parts, the descriptive study,to define the cause of failure in risk reduction by personalinterview, and the quasi-experimental study, to analyze theresult of applying 8-week FPIP. Inclusion criteria:Asymptomatic male AF officers, of age range 35-60 years,who had persistent high mCRC risk (predicted 10-yr CVDrisk > 20%) for two consecutive years, had no CVD and hadan available spouse to participate in the FPIP. Exclusioncriteria: We excluded any symptomatic officers, age < 35 or > 60 years, who had CVD or serious illness such as cancer,psychological disease, secondary causes of hyperlipidemiaand had unavailable family members. After approval by theresearch committee, these persistent high risk AF officersvoluntarily enrolled in the Preventive clinic, Division ofPreventive Medicine, Directorate of Medical Office, RoyalThai Air Force.
The detail of the study flow is shown in Figure 1. Thepersonal interview and discussion were conducted in aseparate room of the Preventive Clinic in additional timeallocated to their regular physician visit. The candidate lifestyles were focused in five areas: dietary habit, smokingcessation, stress by self-evaluation, exercise pattern andcompliance of medication. Results of pre and post interventionafter eight weeks of FPIP were compared for bothbehavioral risk profiles and the biochemical variablesincluded fasting blood glucose, total cholesterol, triglyceridesand HDL cholesterol. The continuous variables weredisplayed by mean ± standard variation and median. Thecategorical data was shown by percent proportion. Themedian variables before and after intervention were comparedby the Wilcoxon signed - rank test. Statistical significancewas considered if the p value was below 0.05. The FamilyPartnership Intervention Program (FPIP) was created to bringfamily members (spouse) participating in life style modificationby recognizing the pre-existing risk, setting a commongoal and supporting the program. In this study, no homevisit was done due to the time constraints and to preventinconveniencing candidates.
The definition of major coronary risk factors5,6 included:hypertension (defined as blood pressure, BP > 140/90 mmHgtaking after rest for at least 10 minutes on two separateoccasions), hypercholesterolemia (total serum cholesterol ≥200 mg/dl), hypertriglyceridemia (serum TG ≥ 180 mg/dl),low high density cholesterol (HDL-C < 39 mg/dl in men and< 43 mg/dl in women), impaired fasting glucose ( plasmaglucose > 100, < 125 mg/dl after fasting for 12 hours), diabetesmellitus (fasting glucose was ≥ 126 mg/dl). Heart healthy lifestyle recommendations were adapted from the 2016 EuropeanPreventive Guideline8 which we simplified into five areas:healthy diet (low cholesterol, high fiber and low sugar),encourage smoking cessation, self-management stress reduction,regular aerobic exercise for 30 minutes at least three times aweek and regular medication.
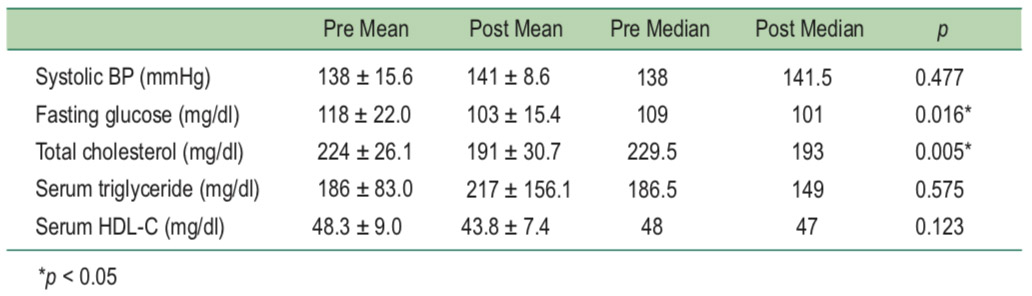
Ten participants voluntarily signed the informed consentfor participation. All of them met the above criteria and hadan average age of 55.2 ± 5.3 years. Most of them (70%) hada sedentary job and all of them were overweight with the meanbody mass index of 26.3. The common pre-existing risk factorswere hypercholesterolemia 80%, hypertension 60%, DiabetesMellitus 40% and impaired fasting glucose 40%. Intervieweddata analysis indicated that all of them did not know the detailsof a heart healthy life style. All candidates (100%) frequentlytook atherogenic (low fiber, high cholesterol and high sugar)diet and most of them (90%) exercise less than twice a week,see Table 1. Cigarette smoking was found in 30% and one-third of cases admitted having mental stress. Six of sevencases (85.7%) who had prescribed medication had full compliance.None of the candidates took any supplement drugs.After eight weeks of FPIP, all but one (90%) of them hadchanged their dietary pattern by reducing animal fat (90%),carbohydrate (60%), oily food (30%), adding more vegetables(70%), see Table 2. Most (80%) of them exercised more thanthree times a week and improved medical compliance to 100%,see Table 2. However, mental stress and cigarette smokingremained unchanged. While the HDL cholesterol (HDL-C)and triglycerides (TGs) were not statistically significantlydifferent, the median total cholesterol and blood glucosereduced from 224 ± 26.1 to 191 ± 30.7 mg/dl, p = 0.005 andfrom 118 ± 22.0 to 103 ± 15.4, p = 0.016 respectively, see Table 3. After intervention, 60% of these high risk participantswere able to lower their risk to 10-20% in five cases and verylow risk (< 5%) in another
Table 1: The baseline parameters of ten persistent high CVD risk candidates is shown below. The laboratoryvalues were obtained from the day of risk assessment. Seven cases (70%) took current prescribed medication butonly six of them (87.5%) had full compliance. Case no. 8 and 10 were on diet control.
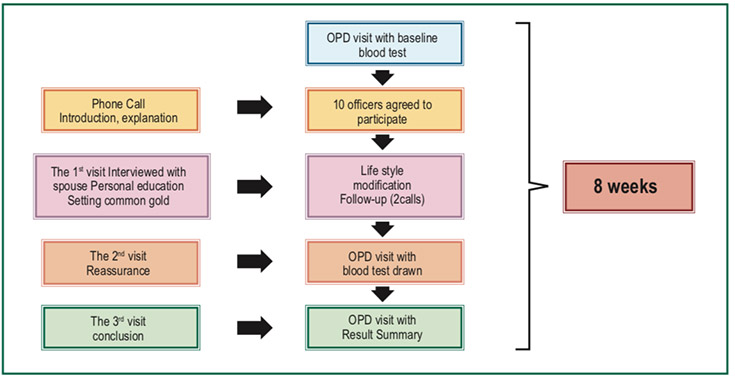
Table 2: The outcome parameters after 8 weeks of FFP are displayed below. All but one of the participants reducedanimal fat which was the major source of cholesterol-rich diet. Most of them (80%) exercised
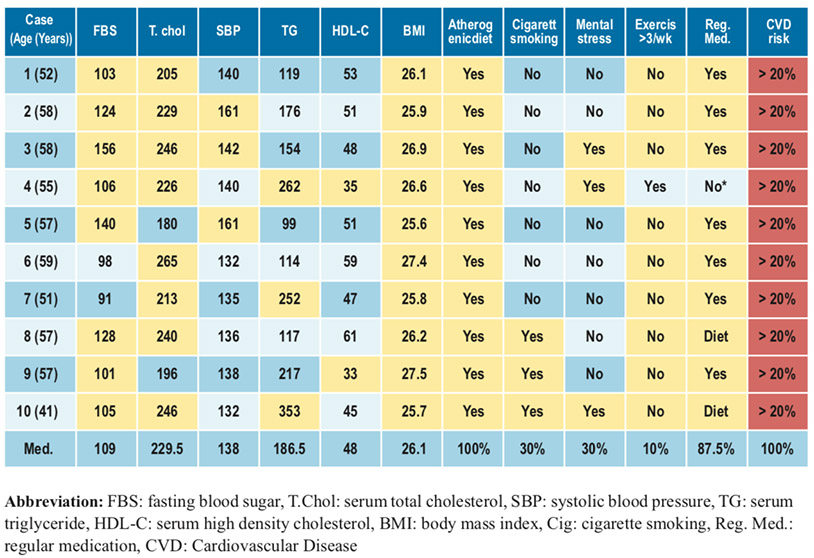
Table 3: The biochemical parameters at baseline and after 8-wk of FPIP were compared. The mediantotal cholesterol and fasting glucose were significantly reduced with the p-value of below 0.05.
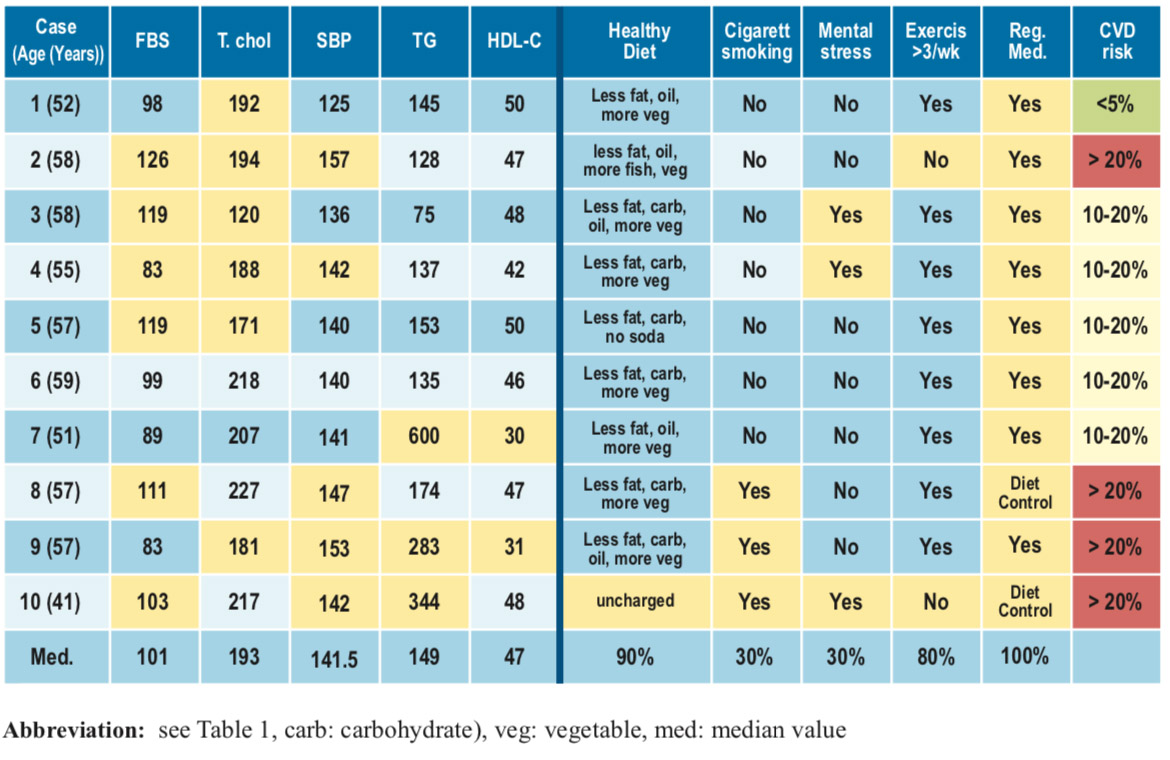
Table 4: The major coronary risk profiles of our case study andthe ACS patients in the Thai ACS Registry 12 were compared.
CVD has multifactorial causes and a long latent period ofmanifestation. The cardiovascular risk increased by the timeof exposure to underlying risk factors. While age, gender andgenetic background could not be modified, other risk factors(high serum cholesterol, hyperglycemia, cigarette cessation,sedentary life style, mental stress etc.) are still correctable.9Previous epidemiological studies had confirmed the impact ofcontrolling these risk factors in CVD events reduction.5,10,11In Finland, the decline of CAD mortality (1972-92), 55% inmen and 68% in women, were mostly due to the reduction ofthree major risk factors, hypercholesterolemia, hypertensionand smoking.10 Controlling similar risk factors in US men alsocontributed to 44% reduction of age-adjusted death rate ofCAD, from 542.9:100,000 in 1980 to 266.6:100,000 in 2000.11 In Thailand, the 10-year prevalence of ACS and stroke inintermediate and high risk AF officers has been reduced aftercontrolling their major risk factors.5
Our studied population truly represented the high-riskcandidates for developing future CVD. Their pre-existingmajor risk profiles were close to those of the ACS patients inthe Thai ACS Registry (2002-5)12 except they were ten yearsyounger but had more hypertension, see Table 4. In addition,an impaired fasting glucose (IFG 100-125 mg/dl, pre-diabetes)or diabetes mellitus and hypercholesterolemia were found in80% of our study cases. The impact of pre-diabetes conditionon CVD risk has been documented in previous studies.13,14 Inthe four-year cohort study of the Framingham offspring, therate of CAD events increased along with the level of plasmaglucose, from 2.9% (100-109 mg/dl), 3.0 % (110-125 mg/dl)and 8.7 % (for 126 mg/dl or more).15 Systemic review of 8publications also confirmed the modest relative risk of IFG(100-125 mg/dl) of 1.18 (95% CI:1.09-1.28).16 Combinationsof these risk factors were synergistic and increased thelikelihood for development of CVD in future.5-9
By analysis of the interviewed data, it was clear that ourcandidates still had insufficient knowledge for healthy lifestyle. Most cases not only had a sedentary job but all of themexercised less than twice a week. Sedentary lifestyle andphysical inactivity are known modifiable risk factors forCVD.9,15 In addition, all candidates had regular atherogenicdiet i.e. high animal fat (cholesterol-rich), high sugar and lowfiber. Cigarette smoking and self-admitted stress was observedin 30% of cases. All of these findings not only explained whythey could not improve their CVD risk but also reflected thefailure of previous group education. By sitting with allcandidates and spouses, common target goals were set andplanned. They were followed by two additional phone callsand two more visits.
At the end of eight weeks, 90% of candidates reduceddietary animal fat, carbohydrate (sugar), oily food and addedmore vegetable by 90%, 60%, 30% and 70% respectively. Inaddition, full compliance was observed in all seven cases whotook prescribed medication and moderate aerobic exercise(at least three times a week) was performed in 80% of cases.Retarding or even regression of atherosclerosis had beenreported in CAD patients after vigorous risk factormodification16 including regular exercise, low fat,17 vegan diet andmedication.18 Regular aerobic exercise could increase coronarymicrocirculation, improve endothelial, muscular function andglucose utilization 19,20. All of these changes contributed to thedecline of the median total cholesterol from 229.5 to 193 mg/dl, p = 0.006, plasma fasting glucose from 109 to 101 mg/dl,p = 0.016 and the CVD risk status in 60% of cases. However,two metabolic parameters remained unchanged, the HDL-Cand TGs. Although regular aerobic exercise could increase theHDL-C level,21,22 it required continuous endurance trainingsuch as marathon runner or triathlon21-23 and for at least 20weeks duration.24 So we did not expect the increment of HDL-Cin our study. From Table 2, three candidates (case no.7,9,10)still had remarkably high triglycerides, ranging from 283-600mg/dl on the final blood test. One case (no.10) did not changediet and later he admitted having alcohol beverage three daysa week which was likely the cause of hypertriglyceridemia.One case (no.7) had very high triglycerides and was lost atfollow-up after the study. It was common that officers did notwant to report drinking alcohol in their medical files. Anothercase (no.9) had stopped alcohol for two years and had beenfollowed up in clinic so the cause of dyslipidemia remainedto be established. Obviously, these failure groups needed moretime and probably additional programs to lower their risk.
Several limitations existed in our study including the smallnumber of cases, the short term of the study (8 weeks) andincluding only AF officers. Results might not be applicable toother population groups. In addition, the long term success inCVD reduction remained to be established. Despite havingspouse involvement, smoking and mental stress remainedunchanged in 30% of cases so more effective programs suchas smoking cessation, stress reduction should be provided.Metabolic evaluation should be improved, for examplemeasurement of HbA1C or serial lipid values would be moreaccurate to assess the average plasma glucose and lipid duringthe preceding eight weeks. Candidates should be morestrictly informed not to take alcohol during the study period.
Despite the above limitations, this is the first study inasymptomatic AF officers to clarify the probable causes ofpersistent high CVD risk. It also offers a better way of riskreduction by FPIP. It was clear that all six successor candidatesdid exercise more frequently (100%), taking regular medication(100%) and changed to a healthier diet (100%). Other optionsfor lowering CVD risk in non-successor group should beinitiated such as coaching by a patient expert (a volunteeredformer CAD case), stress reduction program and smokingcessation with nicotine supplement should be provided. Longterm study is mandatory to establish the success of CVD riskreduction. Finally, we would like to sincerely thank allcandidates and their spouses for their dedication, members ofPreventive clinic, Division of Preventive Medicine, Directorateof Medical Office, Royal Thai Air Force and all advisors fortheir tremendous support.