Over the past decades, the prevalence of cardiovascular disease (CVD) has shifted from the population in western societies to people in developing countries.1-3 In 2001, around 80% of global cardiovascular death occurred among people in the low and medium income countries.1,3 In the Republic of China, from 1984 -1999, the prevalence of coronary heart disease rose 41% in men (2.7% per year) and 39% in women (1.2% per year).4 In Thailand, the rate of Thai people presenting with cardiovascular disease increased from 68:100,000, in 1999 to 73.7:100,000 in 2002.5,6 In 2014-5, cardiovascular diseases (CVD) became the leading causes of death, in nearly one-third, of Thai military officers, outranking the death from cancer and accident.7 In addition, data from the myocardial infarction registry of the cardiovascular research and prevention center, Bhumibol Adulyadej hospital indicated that one-third of heart attack victims were either Air Force officers or family members.8 With no existing primary prevention program, we conducted a pilot cardiovascular screening in Air Force officers at the Air Flying training school and Chandrubeksa hospital, Nakorn Pathom in 2006.9 The main purposes were to identify the target candidates who carried the substantial risk of developing cardiovascular events and prevent them in advance.
The studied population
Inclusion criteria: It is government policy to perform an annual check-up for all in-service Air Force officers, from age 35-60 years. In 2006, of total of 1,021 available officers at the Air Flying Training school, Nakorn Pathom, 412 (40%) Air Force (AF) officers aged 35-60 years old were all voluntary enrolled. Informed consents were obtained after the risk/ benefit was explained. Exclusion criteria: Officers aged below 35 or above 60 years old in 2006, not willing to sign the informed consent or having known CVD would be excluded. This study was approved by the ethics committee and medical organization of Chandrubeksa Hospital in 2006.
Screening pathways
The screening pathway is shown in Figure 1 below. In 2006, all volunteers underwent an annual physical check-up and blood chemistry tests including fasting plasma glucose, total serum cholesterol, low and high density cholesterol (LDL-C, HDL-C) and plasma triglyceride. In addition, we included the family history of premature atherosclerosis (occurring before age of 55 years) and familial history of elevated serum cholesterol (Chol) and triglyceride (TG) as required for the mCRC calculator.
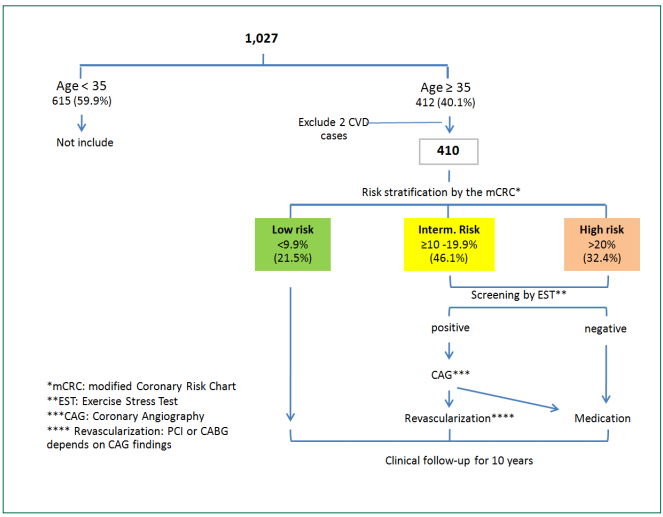
Figure 1: Screening pathway in volunteers aged ≥ 35 and < 60 years
The screening tool and risk estimation
Although several screening tools were available,10-21 we chose the CRC for specific reasons. In 1998, three major Joint European Societies introduced the CRC to predict the 10-year risk of both fatal and non-fatal coronary events.10 Before summation, the risk factors used in the CRC were graded by severity which it was better than using the categorized risk score.11 Although the CRC was not initially designed to predict stroke, cerebral and coronary vascular diseases also shared common risk factors,10-12 so we added all types of stroke to the clinical outcome. Based upon our previous study, as discussed in Asian Heart Journal 2012, 9 the CRC had been fairly reliable for retrospectively predicted events of Thai patients who already had documented coronary heart disease, compared to the Framingham12 and the Electric Generating Authority of Thailand (EGAT-RAMA) risk scores. The latter was derived from the longitudinal study of EGAT employees.13 In addition, by using impaired fasting glucose (>100 mg/dl) as an equivalent risk to diabetes mellitus, the mCRC appropriately identified the population at risk in asymptomatic AF officers in the 5-yr prospective study as well.9 This mCRC risk score is available at www.thaiafheart.com*. We did not use the SCORE risk calculators since it was based on the selected European population of high and low risk countries and it predicted only a fatal cardiovascular outcome.14 We realized that using the western tool in oriental population could result in an estimation error,15-20 therefore we conducted this 10-year cohort study for verification. According to the mCRC, three sets of the studied population were classified into low risk (10-yr risk < 9.9%), intermediate risk (10-yr risk 10-19.9%) and high risk (10-yr risk ≥ 20%) groups. The presumptive target group referred to those who had a predicted 10-yr risk above 10% (combined intermediate and high risk groups).9
Protocol and outcome
By physical examination, known CVD cases would be excluded. After the risk status was informed, group education for life-style behavior was provided for all candidates. Medications were started in the intermediate and high risk groups. All of them were followed from 2006-2016 by annual physical check-up as mentioned before. By setting the desirable values of the uncontrolled risk factors, physicians who took care these target groups would be able to treat them more effectively. After ten years, the clinical outcomes were compared between each group with the 95% confidential intervals. Death or sick certificates and hospital records were reviewed and analyzed to identify the causes of death or admission to hospital. The primary end points were the prevalence of 1). acute coronary syndrome (ACS); included both fatal and non-fatal of ST segment elevation ACS (STE-ACS) or non-ST segment elevation ACS (NSTE-ACS) events, 2). stroke (cerebral vascular disease included both ischemic and hemorrhagic types) and 3). total death (all types of death). Secondary end points were the composite events of ACS, stroke and total death. Each outcome was counted as a separate event. All ACS and stroke cases were individually confirmed by cardiologist and neurologist.
Cardiovascular test and intervention
Based upon our previous study,9 we performed the treadmill stress test (standard Bruce protocol) for candidates who had the predicted 10-yr risk above 10% (intermediate and high risk groups). The endpoints of the treadmill test were; achieving 85% of aged predicted maximal heart rate or having ischemic response: angina symptom in conjunction with ischemic ST segment changes. Candidates who had an ischemic response within 7 METs would be referred for coronary angiography. Revascularizations, either coronary bypass surgery (CABG) or percutaneous coronary intervention (PCI), were recommended only if indicated. The rest of them were medically treated and supervised for life-style modification particularly smoking cessation, regular exercise and dietary counseling. The risk profiles were reassessed annually.
The definition
The definition of major coronary risk factors9,10 included: hypertension (defined as blood pressure (BP) > 140/90 mmHg taking after rest for at least 10 minutes on two separate occasions), hypercholesterolemia (total serum cholesterol ≥ 200 mg/dl), hypertriglyceridemia (serum TG ≥ 180 mg/dl), low high density cholesterol (HDL-cholesterol < 39 mg/dl in men and < 43 mg/dl in women), impaired fasting glucose ( plasma glucose > 100 mg/dl after fasting for 12 hours), diabetes mellitus (fasting glucose was ≥ 126 mg/dl). Regarding to our previous study,9 we considered impaired fasting glucose as an equivalent risk to diabetes mellitus. The desirable body mass index (BMI) ranged from 18.5-24.9 kg/sq.m., overweight BMI ≥ 25, obesity BMI ≥ 30. Occult coronary artery disease included significant epicardial coronary stenosis (>70% of luminal diameter), microvascular dysfunction (slow coronary flow phenomenon), vasospasm, myocardial bridging and non-obstructive CAD (luminal diameter stenosis of ≥ 20% but ≤ 70%).
Statistical methods
The continuous variables were displayed by mean and standard variation and compared by the Student t-test. The categorical data was shown by percent proportion and compared by the Pearson Chi-square test. The relative risk, with a 95% confidential interval, was calculated between each group and the statistical significance was determined when the p value was below 0.05.
Demographic data
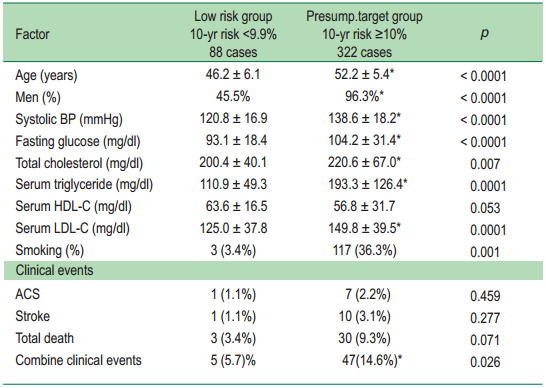
Of a total of 1,021 available Air Force (AF) officers, 412 (40.1%) candidates met the age entry criteria but two of them were further excluded due to having severe mitral valve stenosis in one and previous stroke in another. Of the remaining 410 cases, most of them were middle aged men (85.4%) and had the mean age of 50.9 years. As shown in Figure 1, the common risk factors were elevated cholesterol (62.2%), impaired fasting glucose or diabetes mellitus (36.8%), hypertension (34%) and cigarette smoking (29.3%). According to the mCRC assignment, all parameters in the presumptive target group (10-yr risk above 10%) were significantly higher than those of the low risk group except the HDL-C which had the p value of 0.05, see Table 1.
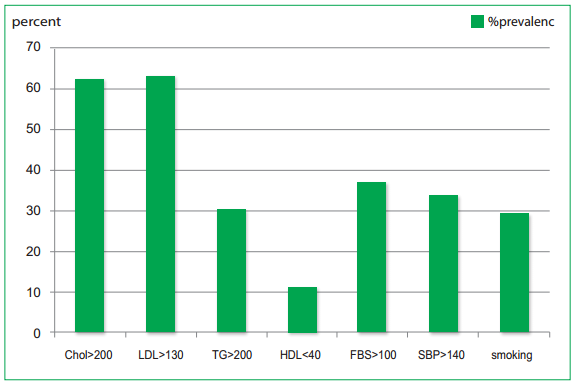
Figure 2: Major coronary risk factors in a total of 410 cases.
Chol = cholesterol, LDL = low density lipoprotein cholesterol, TG = triglyceride, HDL = high density lipoprotein cholesterol,
FBS = Fasting blood sugar, SBP = systolic blood pressure
Table 1: Comparing profles of major risk factors and outcome between the low-risk and the
presumptive target (intermediate plus high risk) group
Clinical end points
After 10 years, we were able to tract all (100%) of their health status. There were only five events (5.7%) observed in the low risk group, one of each was from ACS, ischemic stroke and three deaths (Table 2). In contrast, there was a total of 47 clinical events (14.6%) that occurred in the presumptive target group (combined intermediate and high risk; risk>10%) group including 7 ACS, 10 ischemic strokes, 2 CVD deaths and 26 non-CVD deaths. Although the combined events was significantly higher in this target group (14.6% vs 5.7%, p = 0.026), only death and composite events were statistically different when compared with those of the high vs low risk group. The event details in each group are shown in Table 2 and discussed below.
Table2: Clinical events among the low, intermediate and high risk sub-group
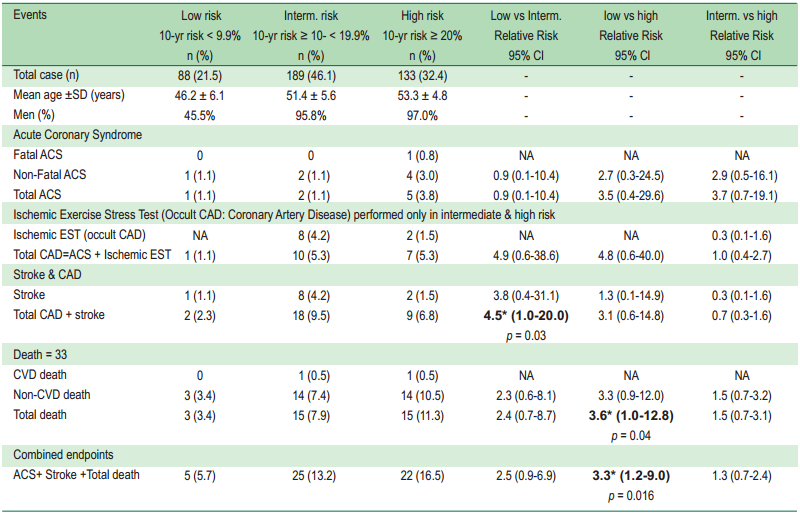
Acute coronary syndrome (ACS) events: During ten years, eight ACS victims (5 STE-ACS, 3 NSTE-ACS) occurred at the mean time of 4.9 years and had the mean age, at index event, of 55.1 years. Although the majority of them (62.5%) came from high risk candidates, the prevalence among the low (1.1%), intermediate (1.1%) and high-risk (3.8%) groups were not statistically different, see Table 2.
Besides the 8 ACS cases noted from the original 410studied volunteers, there were two additional STE-ACS casesthat we did not include in this analysis. The frst one was ahigh-risk 34 year oldman who was excluded by age entrycriteria in 2006. Three years later, he had STE-ACS at age of 37, see Figure 3A-C and the discussion that follows. Theother one was a 55 year old man who was transferred later in 2011. He was also a high risk candidate from diabetes mellitus,hypertension and hypercholesterolemia. With medication, hispredicted risk remained in the range of 10-20%. Unfortunately,he stopped all medicine in 2015 and the risk was up to 20-40% before having acute anterior STE-ACS a few months later.He received stent implantation and did well. These additionaltwo cases illustrated the important role of risk prediction and the consequence of unsuccessful risk reduction.
Stroke: No hemorrhagic stroke was observed during a 10-year period. All 11 strokes were of the ischemic type and had a mean age of 61.1 years. Time to stroke varied from 1-10 years with an average duration of 7.1 years. The common risk factors were men (100%), hypercholesterolemia (63.7%), hypertension (54.5%), impaired fasting glucose or diabetes mellitus (45.5%) and cigarette smoking 18.2%). Most of the stroke victims (72.8%) came from the intermediate risk group, only one and two stroke cases were from the low and high risk candidates respectively. However, there was no statistical difference observed among the three categorized groups, see Table 2. The only stroke victim from the low risk group was a 63-year-old man who had sick sinus syndrome, atrial fibrillation. These conditions were the known causes of embolic stroke and might not be relevant to his low-risk status. Therefore, apart from the atrial fibrillation, there was no stroke event in the low risk members.
Detected occult coronary artery disease: Exercise stress test (EST) was performed in 323 candidates who had an estimated risk of ≥ 10%, ten cases (3.1%) had ischemic response and the majority of them (72.7%) were from the intermediate group. Four cases (40%) had severe coronary stenosis and received coronary revascularization including coronary bypass surgery (CABG) in one case and percutaneous coronary interventions (PCI) in three other cases, see Figure 4. The remaining six cases received medical treatment for non-obstructive diffuse CAD, vasospasm, slow flow from coronary microvascular disease and myocardial bridging.
Death: There were 33 deaths observed during the 10-yr cohort and 94% of them died from non-CVD causes. The mean age of fatal cases was 59.4 years and average time to death was 6.7 years.
CVD death: Only two CVD deaths were observed, one from ACS and another from stroke. The ACS case was a 48 year old man who had a very high predicted risk (>40%) in 2006 from multiple risk factors; cigarette smoking, diabetes mellitus, hypertension, hypercholesterolemia and low HDL. He still smoked cigarettes, did not take medication so his risk remained consistently high. In 2009, at age 51, he had fever, diarrhea and suddenly collapsed at home. After cardiopulmonary resuscitation from asystole and ventricular fibrillation, electrocardiogram showed sinus rhythm with ST segment elevation in leads V1, V2 and 3 mm ST depression in inferior and lateral leads indicating of STE-ACS. He had prolonged shock and died within 24 hours from uncorrected acidosis. The other one was a 61-year old man who had an initial risk, in 2006, of 10-20% from impaired fasting glucose and hypertension. Moderately impaired left ventricular systolic function, ejection fraction of 0.30, of unknown etiology was also noted. Despite medication including aspirin 81 mg/day, enalapril, simvastatin, his risk still increased to 20-40% over the next two years. He developed acute right basal ganglion infarction and died suddenly from acute heart failure, three days after he went home.
Non-CVD death: From Table 3, the common causes of death were cancer, 36.4%, cirrhosis (18.2%), followed by accident (9%) and drowning (9%). Again, there was no statistical difference among the three categorized groups, see Table 2.
Table 3: Causes of 33 deaths observed during ten years (2006-2016).
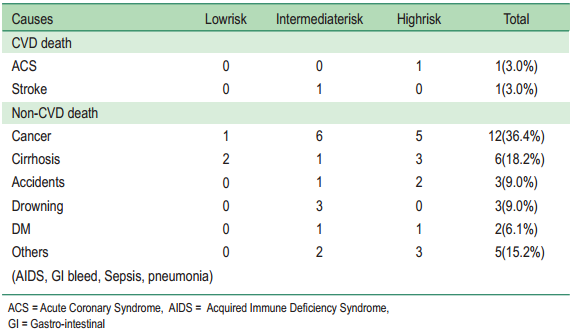
Table 4: Comparison of major risk factors between our study and ACS registry study
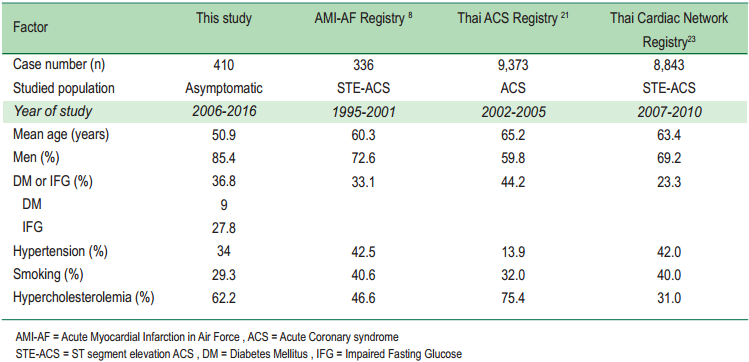
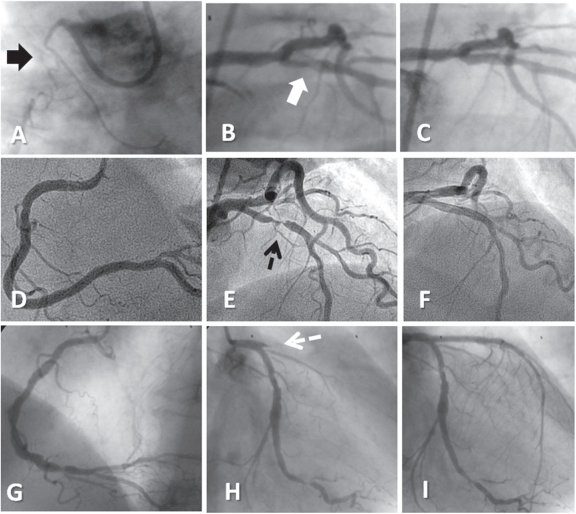
Figure 3: Sample coronary angiograms of three cases who had poor medical compliance and persistent high risk before ACS development: Upper-row (A-C); A 37 years old, high-risk man who he was excluded by age of 34 in 2006 and had STE-ACS three years later. Post thrombolysis angiogram showed an occluded RCA (A), a localized thrombus in the proximal LAD artery (white arrow, B) before and after stent implantation (C). Middle- row (D-F); A 51 years old, low-risk woman, who had risk progression contributing to STE-ACS over nine years. An unobstructed RCA (D), subtotal proximal LAD stenosis before (E) and after stent implantation (F) were shown. Lower-row (G-I); A 47 years old, high-risk man, who had an initial negative stress test and STE-ACS at age of 50. Distal lesion in the RCA (G) and a totally occlude proximal LAD artery before (dashed white arrow H) and after stent implantation (I) were illustrated.
ACS = Acute Coronary Syndrome, RCA= Right Coronary Artery, LAD= Left Anterior Descending Artery,
STE-ACS= ST segment Elevation Acute Coronary Syndrome
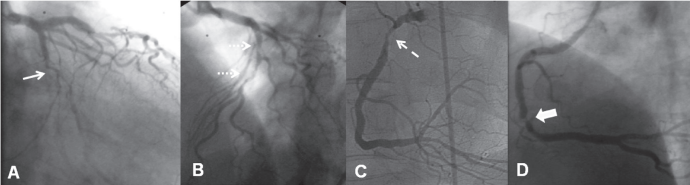
Figure 4A-D: Sample coronary angiogram of three asymptomatic, intermediate risk members who had occult CAD which were detected by a positive exercise stress test. Case 1: A 53 years old, ex-smoker, diabetic and dyslipidemic man, had a totally occluded mid Cx artery (A, white arrow) and diffuse severe LAD stenosis (B, white dashed arrow). He received coronary bypass graft surgery and did well thereafter. Case 2: A 51 year old man, with history of diet control diabetes mellitus and low HDL, who had a severe stenosis of the proximal RCA (C, dashed arrow). He underwent stent implantation and had negative stress test in 2015. Case 3: A 58 year old, asymptomatic man, with history of diabetic mellitus, dyslipidemia, who had a subtotal stenosis of the mid RCA (D) required stent implantation.
CAD = Coronary artery disease, Cx = Circumflex artery, LAD = left anterior descending artery, HDL= High density lipoprotein cholesterol RCA= right coronary artery
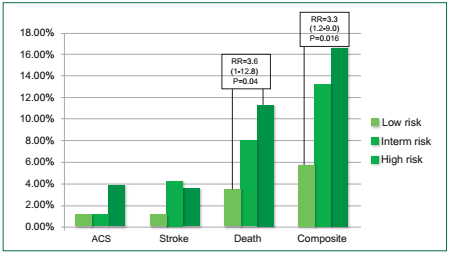
Figure 5: Histogram compared the clinical endpoints of each group. None of them were statistically different, except the death and composite events between the low vs high risk groups.
Table 5: Comparison of risk assessment in 410 cases by modified Coronary Risk Chart (mCRC), Thai CV (updated EGAT-RAMA) and Color Chart (SEARB) was shown. Low, intermediate and high risk were categorized by calculated risk of < 9.9%, ≥10-19.9% and ≥ 20% respectively. Exercise stress test was performed only in candidates with risk ≥ 10% by mCRC so it was not available in the mCRC low risk group. This positive (+) EST group was reassessed by the Thai CV and Color Chart. There were statistically significant different in +EST, death and combine events as shown by marker below.
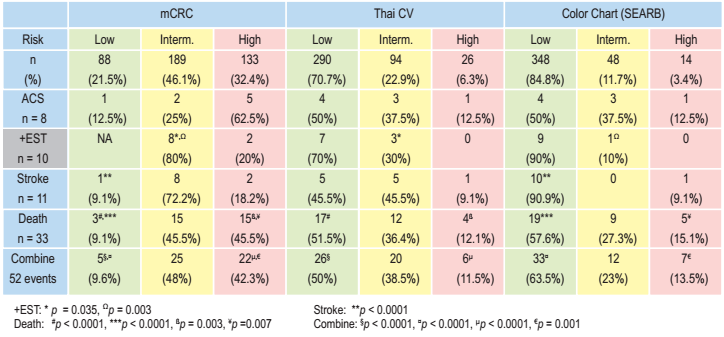
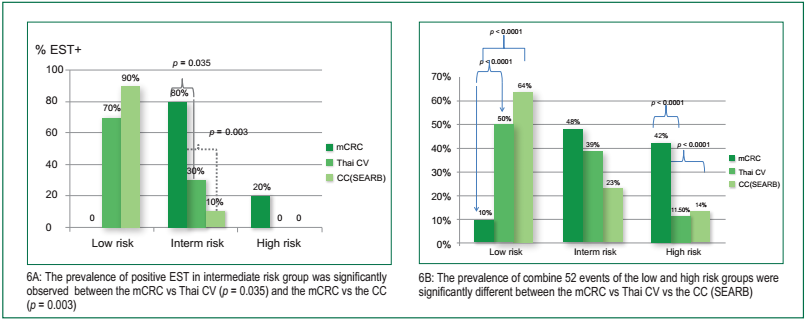
Figure 6: From table 5, the prevalence (%) of positive exercise stress test (performed only in intermediate and high risk groups) and their combine 52 events (ACS+ stroke+ death) by each risk score were illustrated in a histogram 6A and 6B respectively.
Studied population
By comparing our asymptomatic population with the victims of the pre-existing ACS registries; the AMI-AF (n=336),8 the Thai ACS registries (n = 9,373),21 the Thai Cardiac Network ACS Registry (n = 8,843),23 we found some common findings. First, the male gender was prominent in all Thai ACS victims, ranging from 59.8-72.6%, and so did our study group, 85.4%, see Table 4. Second, all ACS victims and our studied population shared common risk profiles, hypercholesterolemia, hypertension, cigarette smoking and impaired fasting glucose or diabetes mellitus. Third, the mean age of our group, 50.9 years, was ten years younger than those of ACS registries.8,21,23 Thus, it seemed reasonable to screen and prevent them from developing cardiovascular events in the next decade.
Reliability of the modified Coronary risk Chart (mCRC)
We compared the predictive results (ACS, stroke, ischemic EST, death) of the mCRC with other two available scores, the Thai CV (updated version of EGAT-RAMA) which was derived from the original study13 and the Color chart (CC) that was recommended by the World Health Organization (WHO) in 2007.24 For the latter one, we used the chart of Southeast Asian region B (SEARB) that included Indonesian, Sri Lanka and Thailand. As shown in table-5, 87.7% and 70.7% of the original 410 cases would be classified as the low risk population by the CC, and Thai CV respectively, in contrast with 21.5% of the mCRC. Of eight documented ACS cases, 50% of them would be assigned as the low risk candidates by the Thai CV and the CC, see Table 5. Although it was statistically indifferent, the mCRC classified only one ACS case (14.3%) as an initial low risk member. Of ten occult CAD (ischemic EST) cases, 70% and 90% would be viewed as the low risk candidates (risk<10%) by the Thai CV and the CC so the EST would not be performed to make their CAD diagnosis. For these +EST “intermediate” risk group, statistically different was observed between those of the mCRC vs Thai CV, p =0.035 and the mCRC vs CC (SEARB), p =0.003. Similar observation was noted in the eleven stroke cases, Thai CV and CC (SEARB) would view 45.5% and 90.9% of them as the initial low risk candidate but the significant different was only noted between the “low risk” group of the mCRC vs those of the CC (SEARB), p < 0.0001. Interestingly, the death and combine 52 events were also statistically different among the low and high risk group of these three risk score, see figure 6 and discussion below. All of these findings supported that the mCRC should be a more reliable tool for preventive screening of our study population.
ACS occurrence was lower than predicted rate
Assuming that the mCRC had the lowest limit of prediction of the, so 5% of 88 low risk members or at least 4 cases would have ACS but there was only one ACS events noted in this group. Among the 322 presumptive target members, 10% or 32 cases would have ACS instead of 7 cases. This low ACS occurrence could be explained by at least three causes: the effectiveness of risk reduction, the screening test and overestimation. First, unlike the CRC recommendation, to start medication only in high risk candidates,10 we provided education for all groups and started medication for both intermediate and high risk candidates. While there were no persistent low risk cases at all developing ACS or stroke, all documented ACS and most stroke cases became high risk candidates within three years of the index events. Therefore, failure to reduce the risk would lead to catastrophic events. Reduction of cardiovascular events by effectively control CVD risk factors had been documented in many western countries.25,26 Second, by screening EST, ten cases (3.1%) had ischemic exercise responses and all of them had explainable causes of ischemia. Severe CAD was noted in 4 cases (40%) which all of them required revascularization, see Figure 4. The other six cases also had definable causes of myocardial ischemia, ACS or even sudden death which included non-obstructive CAD,22 coronary slow flow,27-30 vasospasm 31-34 and myocardial bridging.35,36 Although EST was not done in the low risk group, the combined total CAD (ACS, ischemic EST) and stroke were significantly higher when compared to those between the low versus intermediate risk group: relative risk of 4.5 (95% CI: 1.0-20.0), p = 0.03, see Table 2. Thus, early detection and pre-treatment could prevent them from future catastrophic events. Lastly, it was still possible that the mCRC might overestimate the risk of ACS in Thai officers like other scores had in Asian populations.16 Ideally, the suitable screening tool should allow no false negative prediction otherwise the candidates at risk would not be identified. By the same token, this type of tool could cause over prediction as well.
Risk progression can lead to a worse outcome
Regardless of the initial risk categorized, risk progression could lead to a worse outcome as demonstrated by the only one low-risk lady who later had STE-ACS. At age 41, she had a low predicted risk, below 10%, and it was sustainable during 2006-2010. Owing to poor medical compliance, her risk further escalated to over 10% in 2011 and far beyond 20% in 2013 when she had an acute LAD artery occlusion. Angiogram of subtotal proximal left anterior descending (LAD) coronary stenosis before and after stent implantation was illustrated in Figure 3E-F. Persistent high risk status, at least three years, as other two cases in figure 3G-I, was consistently noted in all ACS cases and most of stroke victims. As the CVD risk rose along the advancing age, we should update the risk for at least every three years. Since none of persistent low risk cases developed either ACS or stroke, any attempts to lowering the risk should be encouraged. Lastly, like these cases in Figure 3, poor medical compliance needed to be improved among those asymptomatic high-risk cases.
The young ACS victims
During 2014-15, cardiovascular disease killed 25-29% of the in-service Thai military officers and outranked death from cancer and accident.7 While the average age of Thai ACS cases ranged from 60.3-65.2 years,8,21,23 our mean age was younger, 55.1 years. The youngest case was a 37 year old man who was excluded by the age of 34 in 2006. This over-weight officer (BMI of 28.3) was a high risk candidate as he also smoked cigarettes presented with hypertension, impaired fasting glucose (112 mg/dl) and hypercholesterolemia (serum cholesterol of 348, triglyceride of 267, HDL-C of 44 mg/dl). Although medications were prescribed, he stopped taking them for three months and had STE-ACS in 2009. Post thrombolysis angiogram (Figure 3A-C) showed severe two-vessel CAD, composing of an old occluded right coronary artery (3A) and the thrombus containing lesion in the proximal LAD artery required stent implantation (3B-C). In general, the young ACS cases (age < 45 years) was quite uncommon.37,38 In Queensland, in a study of 4,549 ACS cases, its prevalence was only 6.1% and the mean age was, close to our case, 38.5 years.37Like the Australian data, the prevalence of young ACS cases from the Thai ACS registry (9,373 ACS cases) was only 5.8%.38 In addition, both Australian and Thai ACS data shared similar risk factors with our case which included a patient who was overweight, a cigarette smoker, presenting with hypertension, dyslipidemia and diabetes mellitus. However, our case did not have a family history of coronary disease which was common in those reports.37,38 The relative young ACS victim like this one and others raised our concern of the primary prevention. Until the suitable screening age becomes justified by more epidemiologic studies, we should not delay stratifying the risk of any young men who shared those aforementioned risk factors.
Ischemic stroke presented later but also at younger age
Stroke cases occurred later than ACS did, at 7.1 years, and their mean age was also quite young, 61.1 years. Similar to our cases, most stroke victims in Thailand were also ischemic type and the most common one was lacunar infarction.39 Although they shared common risk factors to ours, their mean age was much older, 65 years.39 During 1994-6, the prevalence of stroke in 3,036 Thai elderly was only 1.22%.40 Ten years later (2004-6), stroke prevalence from the TES (Thai Epidemiologic Stroke) increased to 1.88% among 19,997 subjects, aged 45-80 years.41 These studies and our data suggested that stroke prevalence was increasing in Thai people and occurred at a younger age. Although most stroke cases (72.7%) came from intermediate risk group, most of them (73%) became the high risk candidates within three years before their events. Again, reassessing the risk in any case who shared the above risk profiles and reducing the risk status should be strongly encouraged.
Predict the excess non-CVD mortality by the mCRC
While the ACS events were lower than we expected, the non-CVD mortality i.e. cancer (36.4%), cirrhosis (18%), accident (9%) were prevalent in the high risk group, see Table 3. This result raised the question, whether or not the mCRC could predict the non-CVD death as well. Some answers already existed in the previous studies that showed the non-CVD mortality was also reduced after controlling those coronary risk factors. In an analysis of data of the five cohorts, involving 366,559 cases, the low risk men and women (defined as serum cholesterol below 200 mg/dl, non-smoker, BP120/80 mmHg or lower, non-DM and had no ECG abnormalities) had 5.8-9.5 years longer life-expectancy than those of the non-low risk group.42 The all cause mortality of these low risk candidates was consistently and markedly lower than the others, 50-58% for men and 40% for women.42 Currently, the Coronary calcium score (CAS), an index of coronary calcified plaque burden, has been proven to be a reliable predictor of future CAD events and was independent to age, sex, ethnicity and conventional risk factors.43,44 In the MESA, Multi-Ethnic Study of Atherosclerosis, coronary calcium scores (CAS) was measured in 6,814 participants. After the mean follow-up of 10.2 years, participants who had high CAS, > 400 Agaston, were also at an increased risk of non-cardiovascular events including hip fracture, chronic obstructive pulmonary disease, pneumonia, chronic kidney disease and cancer, with the hazard ratio of 4.29, 2.7, 1.97, 1.70 and 1.53 respectively.45 Although the clear explanation remained unknown, these studies supported the positive association between coronary risk reduction and non-CVD mortality. By these means, controlling all possible risk factors would not only reduce ischemic events but also the non-CVD mortality as well.
Several limitations existed in our study. First, this is a single center prospective study with a relative small number of 410 cases. Second, according to government policy, we excluded subjects who were aged below 35 years and above 60 years, thus, the result could not be applied beyond this range. Third, as the cohort of the study came from a military based population, the majority (85%) of them were men in the middle age group, so it cannot represent the whole Thailand population. In fact, it did represent the experienced officers in the Force. Lastly, we did not perform EST in low risk members due to a lack of indication and evidence of any benefit so we did not know the prevalence of occult CAD in this group.
Despite the above limitations, from the best of our knowledge, this study was the first 10-yr cohort study that showed the feasibility of predicting and preventing cardiovascular events in asymptomatic officers. The observed CVD events were > 50% lower than expected rates and the mCRC could be used as a reliable screening tool to identify the population at risk which was the high risk members. Progression to ACS or stroke was also observed in non-high risk cases therefore we recommend re-assessing CV risk every 3-year. Although documented CAD cases were found in only 3% among individuals who had the risk above 10%, but almost half of them required revascularization and the rest still had definable causes of future ischemic events. Thus EST could be an additional tool for early detection in this group. While the ACS and stroke rates were lower than expected, we observed the high rate of non-CVD death which was significantly increased in the high-risk group. This group of individuals should be targeted for further preventive measures related e.g. smoking and alcohol consumption. Finally, we hope that this study would bring more research attention in preventive medicine to our Thai colleagues, not only for lowering the CVD events but also all causes of mortality.