Priapism is a relatively rare condition characterized by the persistent erection in the absence of sexual arousal. There are two main subtypes.1 The more common ischemic or low-flow, is characterized by the impaired outflow from the corpora cavernosae, and non-ischemic, or high-flow is most often caused by trauma, characterized by the formation of an arteriovenous fistula, with increased flow of blood to the corpora cavernosae. With high-flow priapism, typically, the penis is neither fully rigid nor painful. Treatment of high-flow priapism in not an emergency case, as oxygen supply to the corpora cavernosae is maintained; hence, patients are at a low risk of permanent complications. The pathophysiology resembles that of compartment syndrome, with blood bypassing the capillary system completely and flowing directly into the lacunar spaces leading to persistent penile tumescence.1,2 Conservative therapy, such as penile cooling, compression of the penile artery and application of vasoconstriction, is almost always without long-term benefits. Surgical intervention in high-flow priapism usually consists of the ligation of a cavernous artery or its branch and is reported to have the highest permanent erectile dysfunction rate, thus it is usually the last treatment option.1-,3 Transarterial embolization using a small caliber coaxial catheter offers the ability to selectively occlude the fistula without damage to adjacent healthy tissue.3-8
We report a case of a post-traumatic high-flow priapism that underwent successful gelfoam embolization.
A 41-year-old patient was referred to us from another hospital. He presented with priapism caused by previous perineal trauma. An urologist from the previous hospital consulted us for arterio- graphy. The cavernous blood gas analysis was in keeping with arterial blood. The initial management involved pressure dressing for one week, but release of pressure caused immediate recurrence of priapism, typical of high-flow category.
Prior to the angiogram, a Foley catheter is placed. The patient was subsequently subjected to angiography under local anesthesia, the right femoral artery was punctured, and a 4 Fr. Cobra catheter was introduced through a 5 Fr. sheath. (The 5 Fr. Cobra catheter was out of stock at the time of the procedure).
The pelvic angiogram was performed in the antero- posterior projection and both obliques are obtained with the catheter at the aortic bifurcation to exclude correctable inflow disease of the common and internal iliac arteries. Selective internal pudendal arteriography is performed. The left internal pudendal artery angiogram showed no abnormality (Figure 1).
A Waltman loop is used to select the ipsilateral internal pudendal artery. The right internal pudendal angiogram shows extremely dense bulbar stain with shunting into the corpora. (Figure 2-3.)
A Curved-tip Microcatheter was advanced coaxially proximal to the fistula over a 0.014 flexible guide wire, but this was not successful. Several attempts were not successful. This was caused by the dislodgement of the Waltman loop: possibly due to the very sharp angle of the aortic bifurcation and the small size of the coaxial catheter. (4 Fr. Cobra) So, a new schedule for the angiogram was set, and the approach via the left femoral artery was undertaken.

Figure 1: Selective angiogram of the left internal pudendal artery in right anterior oblique view appears unremarkable.
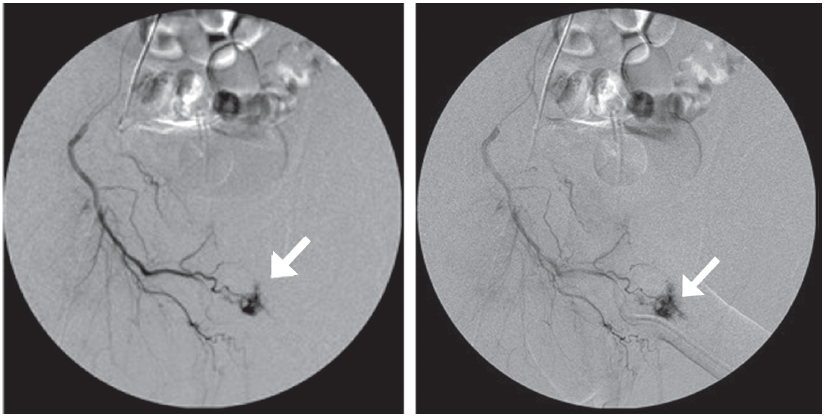
Figure 2-3: Selective angiogram of the right internal pudendal artery in left anterior oblique view shows blood pooling in the cavernosum secondary to arterio-corporal fistula. (see arrow).
Two days later, the patient still had priapism, so an angiogram was performed via the left femoral artery approach. A 5 Fr. Cobra catheter was used for the right internal pudendal angiogram. A Curved-tip Microcatheter was used for super selective examination. The defect was occluded using gelfoam. Improvement was reached with the closure of the fistula at the angiography check showed significant detumescence. He was kept in the hospital for 48 hours under observation after the procedure, and no complication occurred (Figure 4, Figure 5-6).
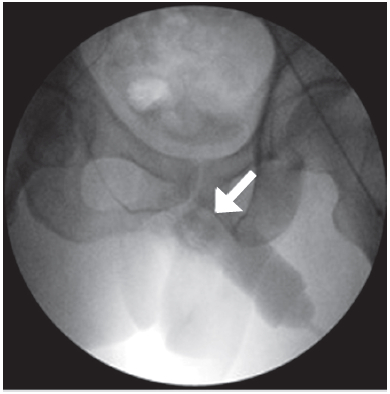
Figure 4: During gelatin sponge embolization. The gelatin sponge is impacted in the corpus cavernosum (see arrow).
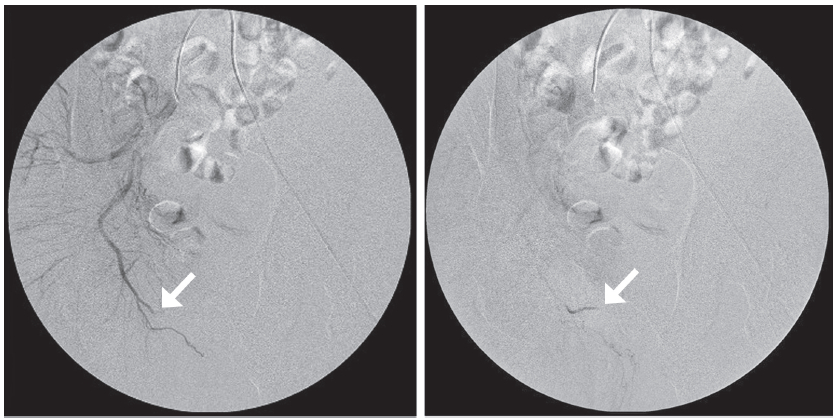
Figure 5-6: The selective angiogram of the right internal pudendal artery shows a complete occlusion of the arteriocorporal fistula (see arrow).
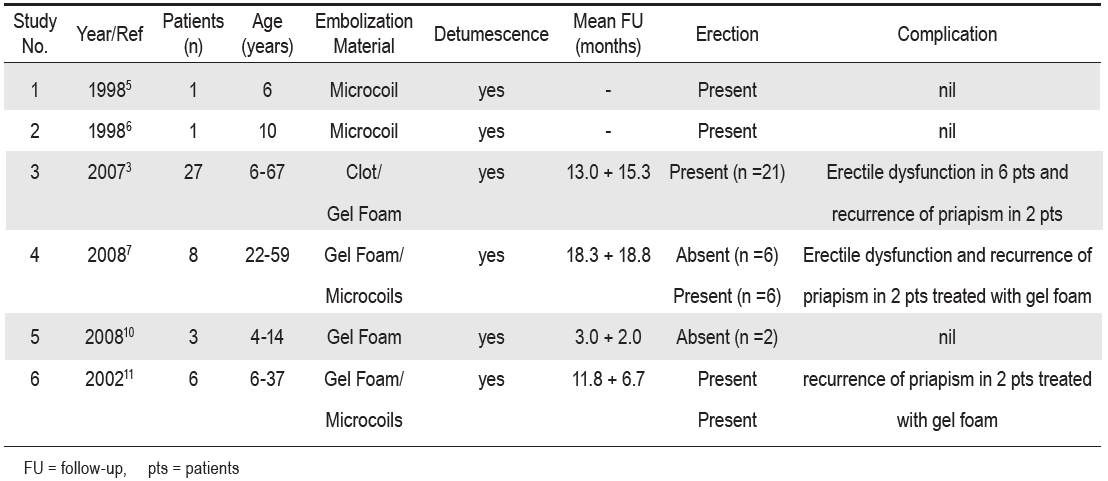
Priapism is a prolonged unwanted erection in the absence of sexual stimulation, and is classified as either low-flow or high-flow. The most common low-flow priapism is due to veno-occlusion: these are painful rigid erections and need emergency treatment with penile drainage to prevent permanent damage. High-flow priapism is less common, and is usually caused by blunt trauma, resulting in a traumatic fistula into the corpus cavernosum. As this is a painless erection,1 management of high-flow priapism includes conservative methods, selective embolization and surgery. Conservative methods include observation, mechanical compression, penile cooling, puncture of corpora cavernosa with blood aspiration, and intracarvernosal pharmacotherapy. However both conservative treatment and surgery are associated with a high risk of erectile dysfunction.1-3,9,14 Selective arterial embolization is firmly established as the treatment of choice in high-flow priapism. The gold standard of super selective arterial embolization therapy is to temporarily interrupt the arterial blood flow feeding the fistula for enough time to allow the injury site to heal without permanently jeopardizing penile erectile function. Embolization can be done using either resorbable (blood clot and gelfoam) or non-resorbable (coil or microballoons) materials.3,5,9,10,13,14 The majority of priapism cases reported in medical literature have been done using resorbable material.3 Overall success rates with embolization are high, with very few complications. (Table 1)
Table 1: Review of high-flow priapism treated with percutaneous embolization.
Selective arterial embolization is a minimally invasive procedure; fistulae can be sealed without damage to surrounding healthy tissue or nerves, there is less morbidity, shorter hospitalization times and the recovery period is much faster.3,4,6-8