Plantar fasciitis is a common foot problem that occurs in 10% of the population.1,2 The most involved age group is 40-50 years old. Chronic inflammation and foot pain can be a result of calcification and is correlated with heel spur.3,4 Actually, symptoms of foot and heel pain can occur due to many different etiologies. Clinical history and physical examination are major keys to unlock the differential causes of heel pain. A knowledge of functional biomechanics of plantar fascia will help both physicians and patients to understand for prevention and rehabilitation techniques.
The treatment options are various and may not be limited to only one best treatment; a combination of therapies can be used. Furthermore, physicians should adjust the proper treatments of choice in accordance with the different circumstances of each person and treating hospital. Nowadays, physicians will use multi modal therapies, combining treatments of choice for a better and faster recovery.
Our review focuses on the practical management of degenerative plantar fasciitis. Mostly successful treatments are conservative, such as load absorbing insoles, stretching exercises and heat modalities.
Plantar fascia is the strong elastic tissue that gives primary static and dynamic stability during walking, running and jumping5 (Figure 1). It has a functional structure of medial arch support for absorption of ground loading activity.6-8 Due to daily activities over a lifetime, the plantar fascia tends to degenerate by overuse, patients being overweight and middle age extending over longer periods. Actually, etiologies cannot be concluded, but it can show in the associated multifactorial factors such as poor quality footwear, arthritic diseases and structural deformity.9
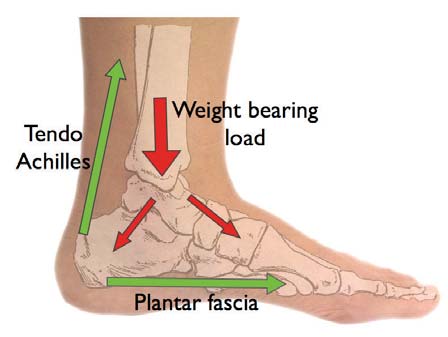
Figure 1: Weight bearing load.
Abnormal arch, low arch, flat feet and high arch have not been shown to be the true cause of plantar fasciitis although abnormal arch can be a cause of fatigue and cuff muscle myalgia.8,10 Abnormal arch can also be a cause of limited sport activities due to limited load absorption. Adequate loading supports such as orthotics, insoles and modified sport shoes are recommended for this group of patients.
Heel spur has not been a proven cause heel pain; chronic heel pain and inflammation may however, induce the calcific formation at plantar fascia origin.3,11,12 More- over, a large heel spur can be a cause of abnormal overload and lateral plantar nerve entrapment. Since this condition can be a secondary cause of heel pain later on, then surgical options may be beneficial.
The classic symptoms of plantar fasciitis are pain and tenderness at the medial heel area with the first steps in the morning or after long periods of rest. The clinical signs will improve after warming up with a few more steps and taking a warm bath. Physical examinations found the maximum tender point to be at the medial calcaneal origin of plantar fascia1,13-17 (Figure 2,3). Radiography may show a calcific formation at the calcaneus call heel spur (Figure 4).

Figure 2: Differential diagnosis landmarks.

Figure 3: Differential diagnosis pathology.
However, even if radiography shows evidence of chronic inflammation, it is not a pathognomonic sign nor does it indicate the surgical removal of calcification. Before using radiography, the author suggests discussion with patients and explaining the natural history of the condition and treatment plan.18,19 Usually, this author would not recommend taking routine radiography because patients get increasingly nervous about calcific spur formations.
Sever’s disease is a calcaneal apophysitis (an inflam- mation of the apophysis of the heel) in adolescents that in radiography appears slightly sclerotic or as a fragment of calcaneal apophysis (Figure 5). For differential diag- nosis,2,4,7,20-23 the locations of maximum pain in the initial examination are the guide to pathological problems: pain in the posterior part leads one to consider Achilles tendinitis and retrocalcaneal bursitis, medial pain suggests tarsal tunnel syndrome and lateral pain may indicate Peroneal tendinitis17,24–26 (Figure 3). For medial calcaneal heel pain, differential diagnoses include heel pad syndrome, calcaneal stress fracture and tarsal tunnel syndrome. Tarsal tunnel syndrome can induce pain referred to the medial calcaneal area and then a positive Tinel’s sign can indicate medial plantar nerve entrapment (Figure 6). MRI investigation can be helpful in cases where conservative evaluations have failed. MRI findings of plantar fasciitis can be thickened fascia, peritendinous edema and partial tears.16,21

Figure 4: Heel spur in radiography.

Figure 5: Sever’s disease in radiography.
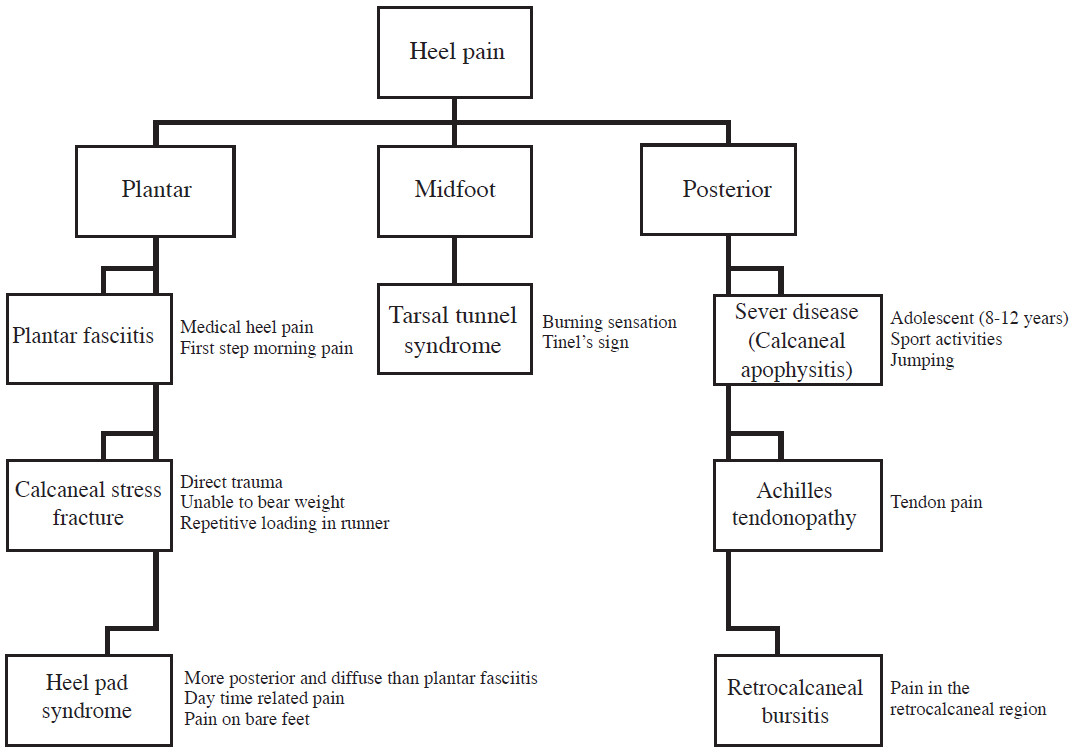
Figure 6: Heel pain diagnosis guideline.
Usually, the major treatments of heel pain with high success rates in good compliance patients are nonoperative. 7,14,20-23,27 These included the following: a short term use period of NSAIDs can be prescribed for active symptoms of inflammation and pain;28 steroid injections should be limited to cases of chronic and failure of first line treatment. First line treatment should be combined in multiple nonoperative treatments.29 With the important landmark injection, physicians should be trained and address the needle directed properly to avoid complication of heel fat pad atrophy and plantar fascia ruptures.29 The American College of Foot and Ankle Surgeons has issued good practice guidelines which be can adapted to be used in each hospital facility.23
The first line of treatment includes insoles, foot taping, foot padding and oral nonsteroidal anti-inflammatory drugs (NSAIDs)1,28,30-32 (Figure 7, 8). Cold and heat therapy should be applied at the appropriate time. Cold therapy (including ice or gel packs) is appropriate for the acute period of inflammation, usually in the first 24 hours, because the inflammatory process needs to be reduced. Usually, heat therapy is of more importance because of increasing tissue elasticity andincreasing blood circulation forthe healing process. Heat therapy includes soaking in warm water 10 to 15 minutes morning and evening, and heat treatment with paraffin but deep heat ultrasound shock waves may be used as a second line. However, the first line warm bath is of practical use. Reducing pressure loading is of importance to avoid repetitive mechanical trauma. Pressure reducing supports include heel cushions, heel cups, insoles, and running shoes. Patients should avoid using flat shoes, walking barefoot, and impact sport or load inducing activities.33 For the latter, regular Achilles and plantar fascia stretching is significant in long-term recovery and needs to take place after pain and inflammation have been well controlled. For the first line treatment, the author aims to educate patients for long-term success and self-help. Initially, continued treatments should be taken within 1 to 3 months with good patients’ compliance. The author advises use of insoles in all shoes (including house slippers), warm bath, short period of NSAIDs (less than 2 weeks) and then stretching exercises (after pain improvement).
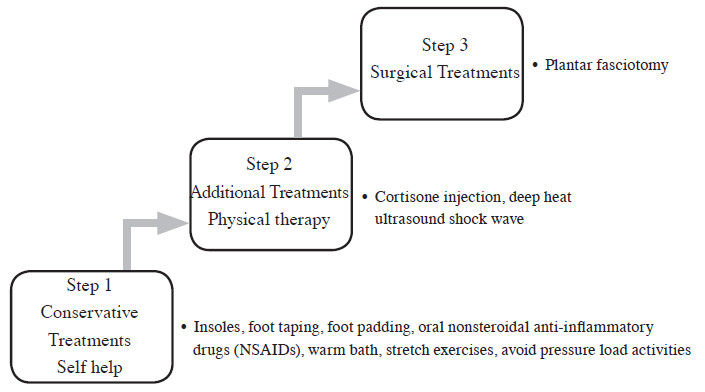
Figure 7: Plantar fasciitis treatment guideline
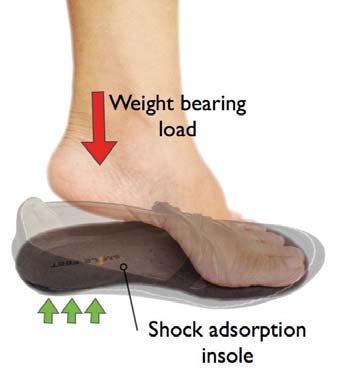
Figure 8: Insole absorbs weight bearing load.

Figure 9: Insole composite properties
Nowadays, insoles are widely accepted for reducing pain in plantar fasciitis.31,34 The author has developed a specially formulated composite insole, Smile feet™ (Images and information from: http://www.smile-feet. com/) (Figure 9) for reducing foot pain and fatigue. Our preliminary research shows its effectiveness in reducing pressure and pain.
The second line of treatment includes continuation of the first line of treatment, cortisone injection,21,29,35 extracorporeal shock wave and night splints.14,36-40 These treatments should be started if first line treatments show no response in one month or little response within three months. Usually, second line treatments will show improvement within 2 months but patients need to understand that treatment should continue until resolution of all symptoms. However, unresponsive patients need to seek reevaluation of cause, diagnosis, associated conditions and their own compliance.
If 6 months have passed and all previous treatments have failed, surgery should be considered as the third line of treatment. However, since almost all plantar fasciitis patients have success with conservative treatment, surgery is the last consideration. Surgical techniques depend on surgeons’ experience and may include endoscopic plantar fasciotomy, in-step fasciotomy, or minimally invasive surgical techniques.21,41,42
Plantar fasciitis is a common condition of heel pain. Clinical symptoms show pain in the morning with the first steps taken and tenderness at the medial heel area of plantar fascia origin. Multi modality treatments are the key to success and include use of insoles, warm baths, short period of oral nonsteroidal anti-inflammatory drugs (NSAIDs) and then stretching exercises. After three months, patients less responsive to treatment should be given cortisone injections and deep heat ultrasound shock wave. The last treatment option for unresponsive cases is plantar fasciotomy surgery.41,42