Dementia is a common disease in the elderly with a rising incidence with increasing age. Diagnosis is crucial for determining patient care and directing the lines of treatment to decrease the rate of dementia progression.1,2
There are number of degenerative diseases that cause dementia including Alzheimer’s disease (AD), dementia with Lewy bodies (DLB), and frontotemporal lobar degeneration (FTLD). There are also number of other neurodegenerative diseases that sometimes present with dementia such as Parkinson’s disease (PD), other Parkinsonian disorders, and Creutzfeldt-Jakob disease (CJD). Dementia can also present in patients with other primary causes such as vascular dementia and AIDS dementia.3 Diagnosis of AD has been based on clinical phenotypes together with pathological changes in the brain.4 Since pathological diagnosis is difficult to obtain from a living patient, diagnosis of AD is predominantly a clinical entity with probabilistic diagnosis (probable or possible AD).5 Since the criteria for AD diagnosis in 1984, there has been evidence that many in vivo biological markers can also accurately diagnose AD during the patient’s lifetime. Thus, in 2007 a new research criterion was proposed, which permits diagnosis of AD with high accuracy.6 Among the in vivo biomarkers, Positron Emission Tomography (PET) is one of the imaging methods that can be used. It is different from anatomical imaging (CT and MRI) which are mainly used to exclude other potential curative diseases that can cause cognitive impairment.2,7 PET is an imaging that uses positron emitting isotopes labeled with human physiologic chemicals or analogues to qualitatively or quantitatively trace cerebral blood flow, metabolism, receptors, transporters, and enzymes within the patient’s body. It is a sensitive tool for diagnosis of diseases even when there is no demonstrable anatomical change. It can also be used to follow disease progression.
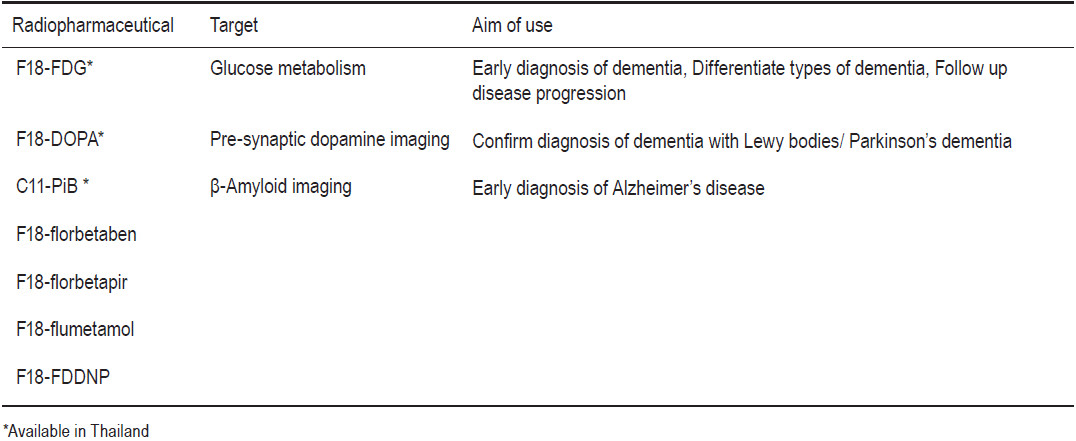
Several radiopharmaceuticals can be used in PET imaging for dementia with different purposes, for example, for early diagnosis or diagnosis confirmation, disease differentiation, or follow up of disease progression. (Table 1)
Table 1: PET radiopharmaceuticals and aims of use.
1. Diagnosis of AD in preclinical or presymptomatic stage
The National Institute on Aging-Alzheimer’s Association in the United States has suggested that Alzheimer’s disease would be optimally treated before significant cognitive impairment, defined as a ‘presymptomatic’ or ‘preclinical’ stage. For this purpose, the use of PET agents which detect amyloid aggregates are of advantage.8 The most widely used agent is C11-PiB (Pittsburgh compound-B) which has a high affinity to amyloid-β peptide aggregates9 and is available in Thailand.
In mild cognitive impairment (MCI) patients who subsequently converted to AD had a high C11-PiB uptake and the level of PiB uptake was comparable to those with AD. In a longitudinal study,10 MCI patients showed serially increased PiB uptake while FDG uptake was serially decreased. In symptomatic AD, PiB uptake was stably high while FDG uptake was decreased in relation to cognitive decline. Thus, abnormal PiB and FDG-PET are detected early in MCI patients who will progress to AD and are predictive of those who will progress to AD.10, 11
In the preclinical stage, which is difficult to identify, F18-FDDNP was studied in those who are at high risk for developing AD.12 Patients recruited were those with impaired cognitive status, older age, and APOE-4 genetic risk for AD, family history of dementia and less education. Impaired cognitive status, older age, and APOE-4 carrier status are associated with increased brain FDDNP-PET binding in persons without dementia, consistent with previous clinical and postmortem studies associating these risk factors with amyloid plaque and tau tangle accumulation.
2. Confirm clinical diagnosis of AD
From a meta-analysis, which analyzed studies which compared various biomarkers and imaging from 1990 to 2010,13 it was demonstrated that FDG-PET was the best way to differentiate patients with AD from normal controls with an area under the ROC curve of 0.96, sensitivity of 90% and specificity of 89%.
In a multicenter study of patients that had patho- logically verified dementia, FDG-PET showing typical parieto-temporal hypometabolism patterns improved the accuracy of “Probable AD” by clinical diagnosis from 73% to 82%.14 Thus, FDG-PET is recommended for use in a patient with difficult-to-clinically-characterize dementia. C11-PiB can also be used to confirm AD pathology in patients with atypical presentations of dementia.15
3. Differentiate other dementia causes from AD
Other than confirming clinical AD diagnosis, PET can also differentiate other types of dementia causes because of the metabolic patterns typical in each abnormality. In the aforementioned meta-analysis, FDG-PET provided the best diagnostic accuracy in differentiating AD from other dementing diseases compared to other biomarkers or imaging methods with a sensitivity of 92% and a specificity of 78%.13
FDG-PET patterns in various dementing diseases are: hypometabolism at parietal, superior/posterior temporal, posterior cingulate and precuneus areas in AD16,17 (Figure 1); hypometabolism at the frontal lobe and ante- rior temporal lobe in FTLD; hypometabolism in the same areas as AD with additional occipital lobe involvement in DLB; scattered hypometabolism in cortical and subcortical areas in vascular dementia.3
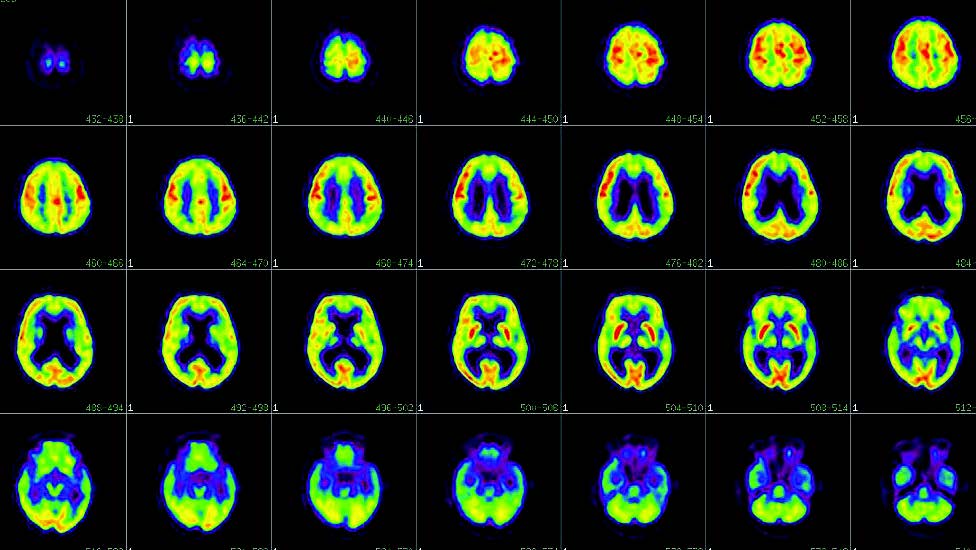
Figure 1: Findings of hypometabolism seen on FDG-PET scan in AD: hypometabolism at bilateral parietal and temporal lobes posterior cingulate cortex and precuneus without abnormalities at primary sensorimotor area, occipital lobe, basal ganglia, thalami, and cerebellum. In advanced disease, hypometabolism at frontal lobes may be seen.
To differentiate DLB or Parkinson’s disease from dementia (PDD) from AD, a radiopharmaceutical that is taken up in the presynaptic site such as F18-DOPA can be used, in which DLB and PDD will show decreased uptake at striatum while AD shows no abnormality.18 This can be applied in patients with suspected visual variant AD because there will be hypometabolism of FDG at occipital lobes confusing differentiation with DLB by using FDG-PET.19
4. Predict response to medications
Currently there are many promising treatment candidates which either slow down cognitive deterioration or even reverse the process of neurodegeneration. Biomarkers which can evaluate the effect of treatment are essential. FDG-PET has proven to be a sensitive biomarker to track these changes.20-22 It can differentiate patients who will respond to particular treatment from those who will not.
The PET/CT scanner was installed in Bangkok in November 2005 at Wattanosoth Hospital. Until now (July 2012), there are 6 hospitals in Thailand (Chulabhorn Hospital, King Chulalongkorn Memorial Hospital, Siriraj Hospital, Bumrungrad Hospital, and Ramathibodi Hospital) that have PET/CT scanners. Currently F18-FDG, F18-DOPA, and C11-PiB are available in Thailand for brain dementia PET scan.
At Wattanosoth Hospital, to date we have performed 128 cases of brain PET, with 93 cases being performed for dementia indications. Others were for epilepsy, brain function in vegetative state, and other indications.
In King Chulalongkorn Memorial Hospital, brain PET scans are performed mainly for epilepsy and dementia.
PET has many roles in dementia diagnosis and management from early diagnosis of AD, confirming diagnosis of AD, differentiating dementia type and predicting responses to therapy. For diagnostic purposes, it should be used in high risk patients and difficult- to-diagnose cases. It can also potentially reduce the costs of long-term treatment in patients already diagnosed as AD.