Oral verruciform xanthoma (VX) is an uncommon oral mucosal lesion that was first described by Shafer in 1971.1 It is a benign mucosal lesion, characterized histologically by papillary or verrucous proliferation of squamous epithelium with the presence of numerous foam cells or xanthoma cells filling the lamina propria papillae. It occurs most commonly between the ages of 30 and 60 years old with a slightly higher incidence in males.2,3 On clinical presentation, it mostly presents with a verrucous appearance.2 The lesion is usually present in the intraoral regions especially on the gingival.4 The purpose of this article is to describe a rare case diagnosed as oral VX based on clinical and histopathological findings, and present a brief review of the literature.
A 37-year-old Thai female presented with an asymptomatic, slightly raised white verrucous lesion, measuring 4x8 mm. in size at the buccal attached and free gingiva of the left second lower premolar region (Figure 1). Interdental gingiva between the left second lower premolar tooth and the left first lower molar tooth was involved by the lesion. It was found during a routine oral examination and the medical history was not remarkable. The patient denied any history of smoking and alcohol consumption. The clinical impression was verrucous hyperplasia and squamous papilloma. An incisional biopsy was taken from this verrucopapillary lesion to rule out dysplasia and carcinoma.
Figure 1: Intraoral examination showed a rough verrucous surface at buccal attached gingiva and free gingiva of the left second lower premolar region.
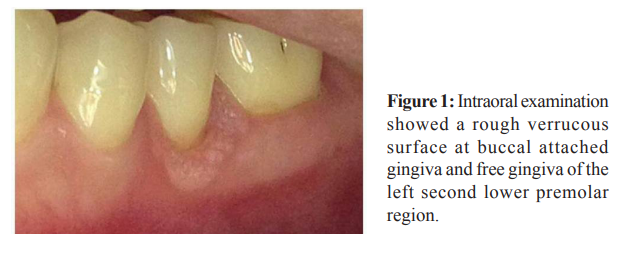
Figure 2: Histopathology
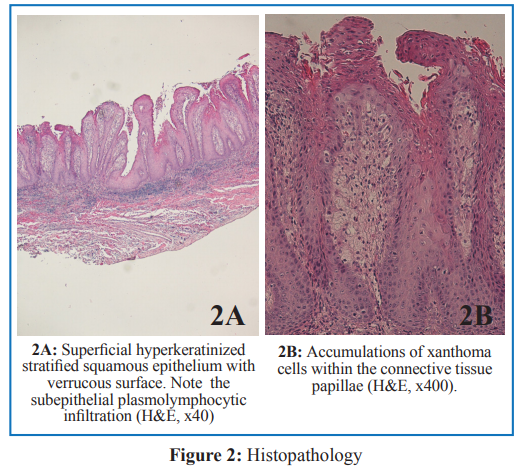
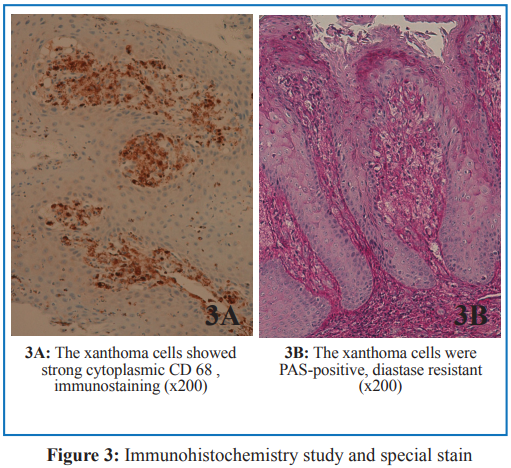
Figure 3: Immunohistochemistry study and special stain
Microscopically, the section revealed a hyperkeratinized stratified squamous epithelium with a verrucous surface and relatively uniform elongated rete peg (Figure 2A). Numerous xanthoma cells of various sizes, with small round eccentrically placed nuclei with granular or foamy cytoplasm, were located in the connective tissue papillae between the rete ridges (Figure 2B). Mild plasmolymphocytic infiltration was seen within the underlying connective tissue. The xanthoma cells were positive for CD68 and PAS-positive, diastase resistant (Figure 3). The diagnosis of oral VX was made. Excisional biopsy follow by mucogingival surgery with free gingival graft was planned but the patient denied the treatment and loss to follow up.
In 1971, Shafer1 reported 15 cases of a heretofore undescribed lesion of the oral mucosa under the term VX. Later, a few cases of extraoral VX were reported, including vulva, penis and skin of the scrotum.4
Oral VX occurs more often in middle-aged patients with a mean age of 51 years.5,6 In the largest series of 282 cases of oral VX reported by Philipsen et al.,4 the most commonly affected site was the gingiva (57.4%), followed by tongue, hard palate, buccal or vestibular mucosa, floor of the mouth, and soft palate, respectively. 4
Clinically, oral VX appears as a small, asymptomatic, verrucous, papillary, or flat lesion with a white, yellow-white, or red color depending on the degree of surface keratinization and the number of lipid-laden macrophages in the connective tissue papillae. 7 The papillary or verrucous outer appearance of the lesion with a broad or pedunculated base often leads to a clinical misdiagnosis of papilloma, verrucous hyperplasia, verrucous carcinoma, or squamous cell carcinoma (SCC).8 The size of oral VX is usually between 2 and 20 mm 9 with the exception of the largest reported lesion, at the lower mucosal fold, measuring 15×40 mm documented by Graff et al. 10
Several previous studies reported an association of a previously occurring or a concomitant oral mucosal lesion with oral VX. These lesions include lichen planus (LP),7,11-13 pemphigus vulgaris (PV),4 oral submucous fibrosis,7 carcinoma in situ,10 SCC,7,15 warty dyskeratoma 16 and graft versus host disease.17 In addition, a case of multifocal VX involving the upper aerodigestive tract in a 2.5-year-old child suffering from a systemic lipid storage disorder was published.18
The characteristic microscopic criteria for a diagnosis of oral VX includes parakeratotic, acanthotic epithelium with verrucous, papillary, or flat outer surface, uniformly elongated epithelial ridges, and the accumulation of a large number of lipid-laden macrophages (xanthoma cells, foamy cells, and foamy histiocytes) in the connective tissue papillae.19 Chronic inflammatory cell infiltrate composed mainly of lymphocytes and plasma cells has been noted in the lesions. In addition, Nowparast et al classified oral VX into 3 types (verrucous, papillary, and flat) according to the microscopic surface architecture of the lesions. The verrucous type is the most common, while the flat type is the least common. 5
Previous studies have shown that these foam cells contain both lipid 7,20,21 and PAS-positive, diastase-resistant granules in their cytoplasm.7,15 The origin of foam cells was found to be macrophages, because these foam cells are CD-68- positive7,22,23 and contain cathepsin B in their cytoplasm.6 Scharlach R and Sudan III stains reveal an abundance of cytoplasmic lipid.24,25 All xanthoma cells were negative for S-100 protein.26,27
Histopathologically, VX can be misdiagnosed as a granular cell tumor, verrucous hyperplasia and verrucous carcinoma.4 Granular cell tumor shows deeper extension of granular cells and does not have uniform rete pattern as seen in VX. 28 In addition, the granular cells in granular cell tumors are positive for S-100 protein.19 Differentiating verrucous hyperplasia and verrucous carcinoma from a VX is important, especially in small and superficial biopsy, xanthoma cells may be scanty and misdiagnose. In verrucous hyperplasia and verrucous carcinoma, the characteristic xanthoma cells are absent; furthermore, verrucous carcinoma shows the epidermal down-growth exhibiting bulbous form rather than relatively narrow ridges.4
The etiology and pathogenesis of VX remains unclear,7 while many factors have been suggested. Zegarelli et al.24 proposed that a ‘local irritant’ might be the initiator of this process because given that 70% or more of all VX are located at the masticatory oral mucosa where localized trauma is very common. The presence of inflammatory cells and colonies of microorganism in the lesion pointed toward ‘a local inflammatory response’.24 It has been found that the oral VX can occur associated with underlying inflammatory disorders of oral mucosa, such as LP and PV, as well as dermatoses. This further, supports the explanation that the lesion is a reactive process initiated by an inflammatory reaction rather than a true neoplasm. 21,24
On the base of condyloma-like growth pattern of these lesions, Santa Cruze and Martin 29 suggested a possible ‘viral aetiology’ for the VX. However, viral particles have never been demonstrated by electron microscopic, immunohistochemical, and in situ hybridization studies while bacterial and fungal organisms have been identified in some oral VX.7 Oliveira et al. 22 suggested that the pathologic process of VX may be based on ‘an immunologic response’ similar to that of LP because both lesions show inflammatory cell infiltration beneath the epithelium. In addition, some authors14,30 have reported VX occurring in patients using snuff or indulging in the habit of chewing tobacco, which points to possible etiological factors.
Zegarelli et al.31 introduced the concept that lipid -containing macrophages accumulate due to epithelial degeneration. The products of epithelial breakdown elicit an inflammatory response and a subsequent release of lipid material through epithelial degeneration, which is finally scavenged by macrophages. On the other hand, Travis et al.18 suggested that xanthoma cells are macrophages responsible for removing lipids that accumulate in the submucosal tissues, and that the epithelial hyperplasia is a secondary event.
The treatment for oral VX is surgical excision and the prognosis is excellent.4 Recurrence of oral VX is extremely rare, and only 3 cases have been reported, 5,6,32 all three cases were localized at the palate. There have been no reports of malignant occurring in VX.
In this report we have presented a case of oral VX at the buccal gingiva of the left second lower premolar tooth, whichDiscussion In this report we have presented a case of oral VX at the buccal gingiva of the left second lower premolar tooth, which clinical appearance, histopathological, immunohistochemical and special stains finding are accordance.
In the present case, the patient was a 37-year-old Thai female with an asymptomatic, slightly raised white verrucous lesion at the buccal attached and marginal gingiva of the left second lower premolar area. The left second lower premolar tooth was normal. The clinical feature and site of the lesion led the clinician suspected for verrucous papillary lesions, which were more consistent with benign lesion than reactive and malignant lesions. The examples of benign verrucous papillary lesions of oral mucosa were squamous papilloma, verruca vulgaris, focal epithelial hyperplasia, condyloma and VX. The first clinical differential diagnosis was squamous papilloma, which was the most common found in oral cavity. The reactive papillary lesions as papillary hyperplasia or inflammatory papillary hyperplasia of the palate, was excluded from our case because this lesion located at the buccal gingiva, rather verrucous surface in clinical feature and the patient did not used denture. One of the clinical differential diagnosis in this case was verrucous hyperplasia, which is a premalignant lesion that may transform into dysplasia and verrucous carcinoma. Furthermore, an incisional biopsy was taken to exclude epithelial dysplasia and carcinoma.
The general histopathologic appearance of this case shows xanthoma cells which ultimately replace the connective tissue between the epithelial ridges. The diagnosis of VX can be made solely on H&E sections. Special stains for xanthoma cells are for academic purpose. PAS-positive, diastase-resistant and CD-68-positive of the xanthoma cells in the section are noted, therefore it is confirmed with oral VX. In our case, the lesion is the verrucous type of Nowparast Classification.
The treatment of choice for our case, in which the lesion is located at the buccal attached gingiva and involved the free gingiva, was total excision followed by free gingival graft. The results of the procedure prevent an insufficient amount of keratinized tissue and prevent gingival recession.
The VX of the oral cavity is a harmless, usually single mucosal lesion with non-diagnostic clinical appearance. The clinical differential diagnosis may be challenging; however the histopathological features are diagnostic and well defined. It is noteworthy that in a small and superficial biopsy, xanthoma cells may be scanty and their presence can be missed. Treatment of VX consists of a simple surgical excision and the prognosis is excellent.