The incidence of venous thromboembolism (VTE, i.e., deep venous thrombosis (DVT) and/or pulmonary embolism (PE)) is now increasing in Thailand because of the recognition of the disease’s burden and greater accessibility to diagnostic tools even in rural areas. The delay in the diagnosis of diseases will bring about many complications, such as post-thrombotic syndrome, and that means more morbidities and mortalities. There is literature to indicate that the incidence of VTE in Thailand or Asian countries is no less than in Western countries.1-8 Many studies on VTE in multiple countries (including Asian populations) have shown that the benefits of VTE prevention far outweigh the treatment of diseases in every aspect, e.g. less suffering and premature mortality, more quality of life and fewer costs overall.9-13 VTE will occur more often if patients already have risk factors, both modifiable and unmodifiable. According to guidelines from National Institute for Health and Clinical Excellence (NICE) if patients, either medical or surgical, have at least one risk factor or have significant reduction in mobility they are considered to be at an increased risk of VTE and they require further evaluation of risk of bleeding before they are administered preventive inter- ventions. If the patient has at least one risk factor for bleeding, NICE guidelines suggest not giving any pharma- cological prophylaxis, unless the risk of VTE outweighs risk of bleeding.13
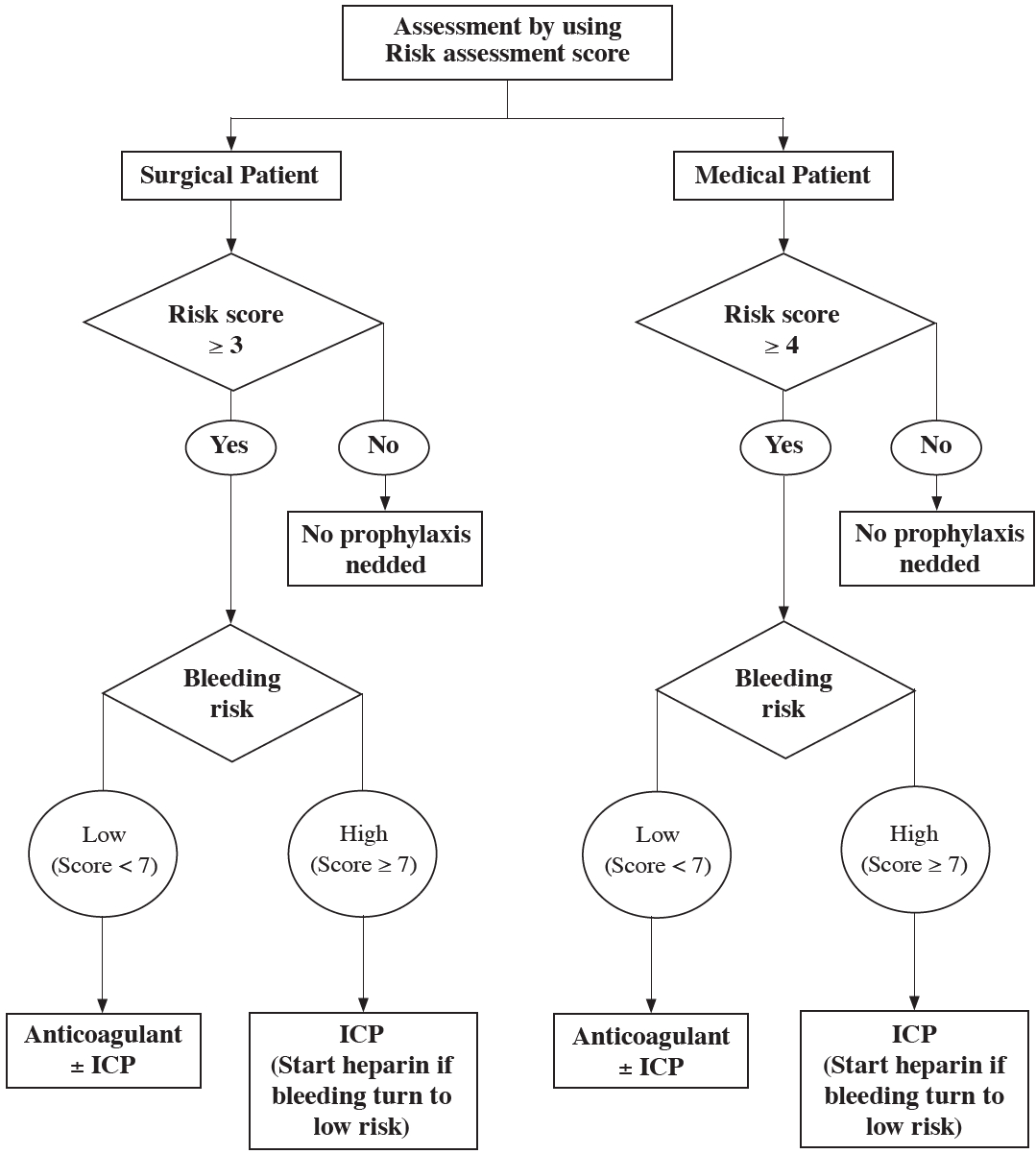
At the Bangkok Medical Hospital Center (BMC) we adapted the NICE guidelines to make a protocol (Appendix 1) to assess the risk of thrombosis and risk of bleeding in our patients, and to guide the prophylaxis interventions. We already knew that some patients are at high risk for VTE without any additional risk factor such as cancer patients, critically ill patients in the Intensive Care Unit (ICU), known cases of thrombophilia and post-operative ortho- pedic surgery patients, so we used this protocol first in this group of patients, starting from 1 Jan 2013.
The study was a retrospective study; we collected data from January 1, 2012 to December 31, 2013 by electronic medical records. The populations are the patients who were admitted to the cancer unit, ICU or orthopedic unit which are the units that apply the VTE risk assessment protocol. Both medical and surgical patients were included. In these groups we selected the patients who met all of our inclusion criteria, those who had been diagnosed with VTE at the BMC, who were 15 years old or older, and have official radiologist reports diagnosis of VTE. Our exclusion criteria are patients aged below 15 years old or with no official radiologist reports.
Once the exclusion criteria were applied, the remaining patients were divided into 2 groups. The first group of patients attended BMC in 2012 and the second group attended in 2013. We applied the protocol only to patients who were hospitalized; therefore we selected IPD patients only. We categorized IPD patients into either high or low thrombosis risk groups using the risk assessment screening for the BMC VTE protocol. We define high thrombosis risk as patients with a thrombosis score ≥ 4 (in medical patients) or score ≥ 3 (in surgical patients). We then used the SPSS program for data analysis. We compared populations from both years to see if there were any differences in baseline characteristics. We evaluated the outcomes when using the preventive protocol by comparing high thrombosis risk patients to low thrombosis risk patients from each year to see if there were any differences in the number of patients before applying the protocol, (in 2012), and after applying the protocol, (in 2013). Then we calculated the odd ratio, relative risk, relative risk reduction and the number needed to treat (NNT).
The total population hospitalized in the cancer unit, ICU or orthopedic unit is 50,027 patients, of whom 26,036 were patients in 2012 and 23,991 were patients in 2013. There were 225 patients with VTE (in 2012 n = 125 (55.56%) and in 2013 n = 100 (44.46%)). Of these patients, 25 patients were excluded (10 patients with no official radiologist reports and 15 patients with missing demographic and clinical data). Of the remaining total of 190 patients, 104 patients were seen in 2012 (54.73%) and 86 patients were seen in 2013 (45.27%). Of these 190 patients, 95 were men and 95 were women. Their mean age was 63.52 ± 17.70 years. Ninety two patients (48.42%) are Thai nationals, while 98 patients (52.58%) are non-Thai nationals. The top three nationalities are British (13 patients), Qatar (11 patients) and Kuwait (11 patients). Details are shown in Figure 1. There were 76 IPD patients (40%) and 114 OPD patients (60%). Of the IPD patients, 71 patients (93.42%) have high thrombosis risk, 39 patients (37.50%) in 2012 and 32 patients (37.21%) in 2013. A summary of patients’ characteristics are shown below in Table 1.
One hundred and fifty patients (78.95%) have underlying diseases. The most common underlying disease that increases the risk of VTE is cancer, found in 56 patients (29.47%). Of these, 19 patients (33.99%) have advanced stage cancer with metastasis. The primary cancers are lung cancer (9 patients (16.07%)), breast cancer (6 patients (10.71%)), colon cancer (6 patient (10.71%)), and rectal cancer (5 patients (8.93%)). Details of primary cancer sites are shown below in Figure 2.
Table 1: Summary of clinical characteristics of enrolled patients (n=190).
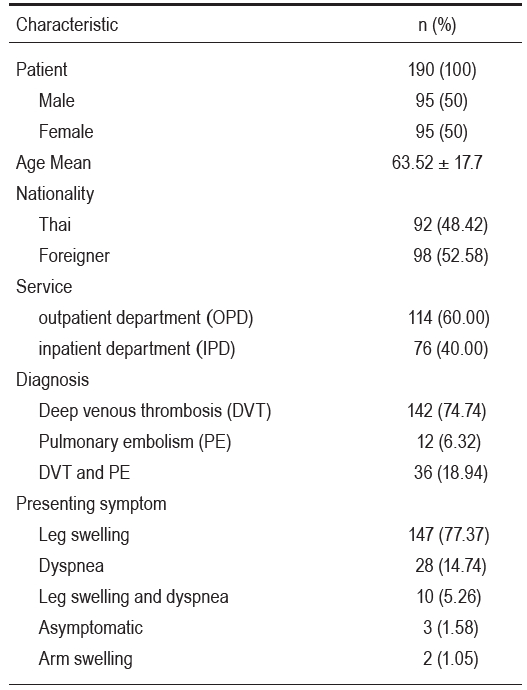
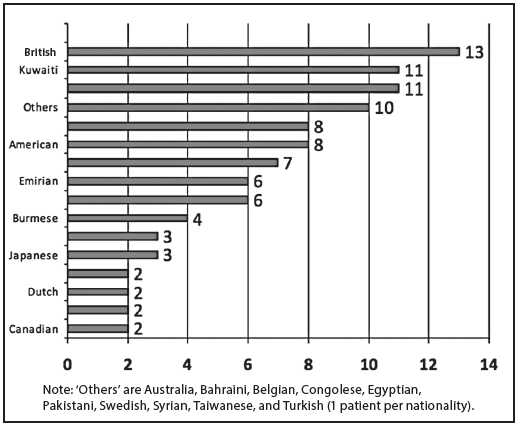
Figure 1: Nationalities of non-Thai population.
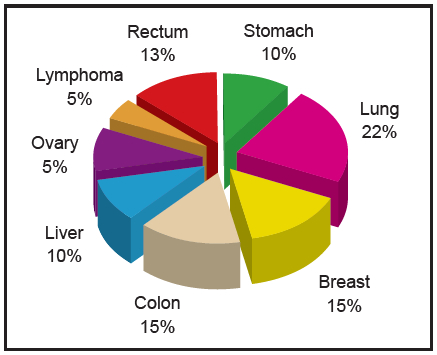
Figure 2: Primary cancer location.
Other underlying conditions that increase the risk of VTE are stroke (after more than 1 month) 18 patients (9.47%), of whom 13 have been immobilized (72.22%). For each of the following diseases, protein C deficiency and protein S deficiency, there are 6 patients with deficiency (3.16%), 3 patients with antithrombin III deficiency (1.58%) and 1 patient with hyperhomo-cysteinemia (0.53%). A summary of details about underlying diseases is listed below in Table 2.
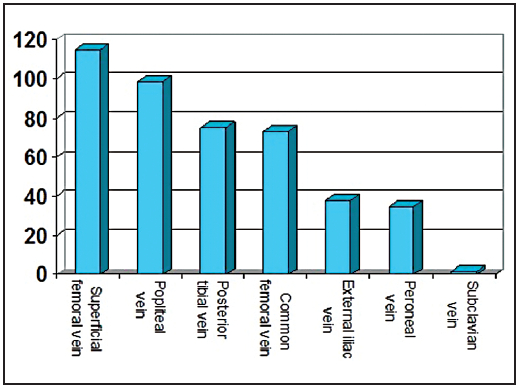
Their most common presenting symptoms are leg swelling (147 patients, 77.37%). The other symptoms are dyspnea (28 patients, 14.74%), leg swelling with dyspnea (10 patients, 5.26%) and arm swelling (2 patients, 1.05%). There are 3 asymptomatic patients (1.58%) with problems resulting from their cancer, and VTE was revealed in the imaging to define the cancer stage. There were 11 patients (5.79%) who died during our study, and every one of these patients had cancer as comorbidity. The causes of death are cancer (6 patients), massive pulmonary embolism (4 patients) and septic shock (1 patient). In 2012, 10 patients (9.61%) died and in 2013, 1 patient (1.16%) died. All of the deceased patients had a high thrombosis risk score. The VTE sites in our study include superficial femoral vein (115 patients (60.52%)), popliteal vein (99 patients (52.11%)), posterior tibial vein (75 patients (39.47%)), common femoral vein (73 patients (38.42%)), external iliac vein (38 patients (20.00%)), peroneal vein (35 patients (18.42%)) and subclavian vein (2 patients (1.05%)). Of the 2 patients with subclavian vein thrombosis, 1 patient has breast cancer, the other is a Kuwaiti female who has been taking oral contraceptive pills for a long time (> 5 years) without any other risk for thrombosis. The data on thrombosis sites are shown below in Figure 3.
For the statistical SPSS analysis, we used the independent t-test analysis and chi-square to find differences in characteristics between both years. The results found that there are two statistically significant differences in the populations between both years. The first is the mean thrombosis risk score, and the mean difference is -0.918 (-1.589 - -0.248, p = 0.008), (mean in 2013 > mean in 2012), the median score in 2012 is 5 and in 2013 it is 6. The second is the number of deceased patients, with more in 2012 than in 2013 (p = 0.013). The other non-significant values and summary details are listed below in Table 3. Patients who have a high thrombosis risk score in 2012 are 37.50% and in 2013 are 37.21%. The odd ratio is 1.013 (0.561 - 1.828), the relative risk is 1.008 (0.696 - 1.459), the relative risk reduction is 0.77 and number needed to treat is 344.82.
Table 2: Underlying diseases of enrolled patients.
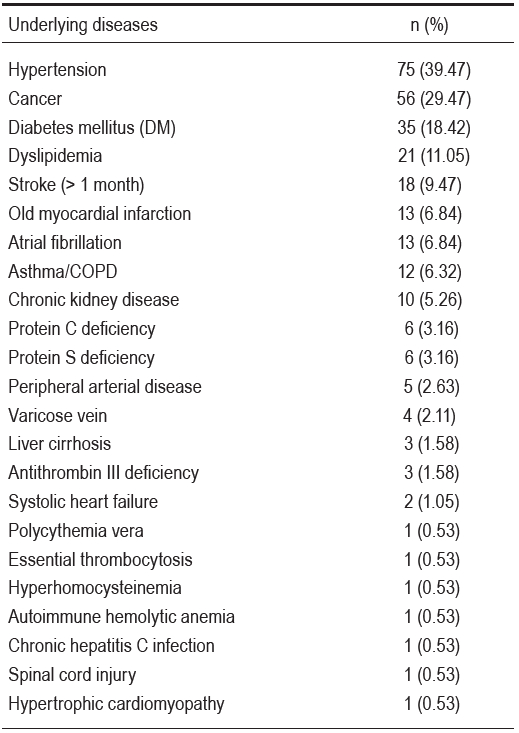
Table 3: Clinical characteristics compared between 2012 and 2013.
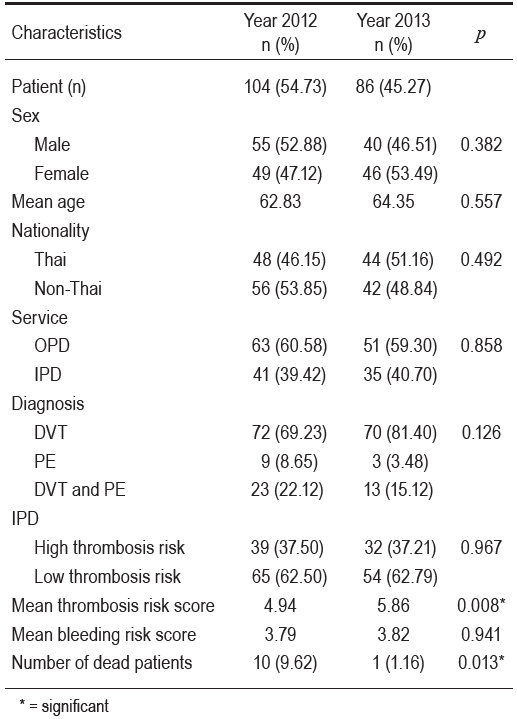
Figure 3: Site of thrombosis
According to the Agency for Health Care Research and Quality, the prevention of VTE is the number one strategy to improve patients’ safety in hospitals.22 There is strong evidence from multiple randomized trials and analyses of appropriately employed prophylaxis of VTE that show it is cost effective and has a desirable benefit-to-risk ratio. In Thailand, however, due to many reasons, the VTE prevention strategy is not applied consistently or regularly. Our study of 190 VTE patients showed a trend in reducing the occurrence of VTE in patients, especially in high risk patients; although it’s not statistically significant due to many limitations.
In our study the rate of occurrence of VTE was the same across men and women. With regards to nationality we found the rate of occurrence in Thai nationals is roughly the same as in non-Thai nationals. This concurs with the findings of previous studies that the incidence of VTE in Thailand is no less than in Western countries.1-8 We used data, however, from a population with VTE, and not from a normal population, so we need to keep in mind that our findings are not necessarily a true rate occurrence of VTE across both Thai and non-Thai nationals. So this data shows that there is a tendency towards an incidence of VTE in Thai nationals that is not low after all, contrary to the old understanding we previously held.
About 60% of patients received OPD services, and the most common presenting symptom was leg swelling (78.5%). There are 3 patients (1.58%) with no symptoms but who do have radiological evidence of VTE. These asymptomatic patients (all cancer patients) incidentally found evidence of VTE from an examination to determine the staging of the cancer with computer tomography (CT). These symptomatic patients were treated for the incidental VTE with a standard treatment if there is no contraindication. Compared to the previous study1 that found asymptomatic VTE to be about 80%, our study has less asymptomatic patients. This is due to differences in population characteristics, study methods and diagnostic tools for diagnosis.
Hypertension is the underlying disease we found most often in our populations, cancer being the second. We know, however, that hypertension, diabetes mellitus, and dyslipidemia all increase the risk for VTE a little, about 1.1-1.3 times14-17, so if we look into disease that significantly increases the risk of VTE the first is cancer, which increases the risk 2-3 times.18-20 The most common primary site of cancer is the lung, followed by breast and colon, and 33.99% of cancer patients have advanced stage cancer. A review of previous literature shows that advanced cancer increases the risk of VTE more than early stage cancer.18 The second most common significant disease that increases the risk of VTE is stroke (after more than 1 month) that confines about 72% of patients to bed. This correlates to previous analysis21 that found VTE more often in paralyzed limbs of stroke patients compared to non-paralyzed limbs (60% and 7%). Inherited cases of thrombophilia in our study included antithrombin III deficiency, protein C deficiency, and protein S deficiency (15 cases (7.89%)). This is found in Thai (4 cases), French (1 case), American (3 cases), Swedish (1 case), Bangladesh (3 cases), Kuwaiti (2 cases), and Bahraini (1 case) patients. It can be inferred that most causes of VTE in Thai nationals are acquired, and not so many cases are due to inherited causes. Therefore, the key to preventing VTE is to reduce modifiable risks as much as possible.
From the analysis, we compared the number of high risk thrombosis patients in 2012 to patients in 2013 and we found the odd ratio for high thrombosis risk patients to low thrombosis risk patients is 1.013 and the relative risk is 1.008 with no statistical significance. But from the comparative characteristics data, between both years we found that patients seen in 2013 have a higher mean thrombosis risk score than patients seen in 2012 with statistical significance (p < 0.05). It’s reflected that although patients in 2013 have a higher mean thrombosis risk score for VTE the occurrence is still lower in 2013. This is interesting data, as we infer that the protocol probably can reduce the number of VTE patients who have a high risk of thrombosis.
There are five limitations to our study. First, our study populations are patients who already have VTE, and are not drawn from the normal population, so there are some limitations to applying our data to real life practices. Second, the number of patients who have VTE is very low compared to the overall population, so when we use statistical analysis it hardly makes the results significant. We think the reason for this is that most patients are not yet aware of VTE, because most symptoms are not painful. Some patients may feel that VTE is not the main issue when they compare this to their underlying disease (for those who already have one, e.g. cancer.) The other reason may come from a lack of awareness of VTE in physicians because most of them just pay attention to the main diseases their patients have. Third, some patients were hospitalized first in other hospitals with no VTE prevention protocols. Then the patients are referred to BMC when their condition gets worse. Prevention in these cases may be too late, because patients may already have had VTE without symptoms and when the main diseases progress more, the symptoms of VTE appeared later. Fourth, this is a retrospective study; there were no randomization in the population and it cannot have a control confounding factor. Due to ethical considerations, it is not right to randomize patients to either use or not use preventive methods because there are many guidelines that recommend VTE prophylaxis in high risk patients.13, 23-28 Fifth, the evidence of VTE using doppler ultrasound has its own limitations, such as in cases of major soft tissue swelling.
These days VTE is a disease that is occurring more frequently than in the past, due in part because today we are more aware of diseases and the technology for diagnosis is more easily accessible. VTE prevention has many benefits, and it is preferable to prevent the disease altogether than cure the disease after it occurs. From our study, we showed a relative reduction in VTE 0.77 when using risk assessment protocol and number needed to treat is 344.82. Although this number may not be statistically significant, due to our study’s limitations, nonetheless we saw a trend towards a drop in the number of high thrombosis risk VTE patients when the prevention protocol was applied.
Appendix 1: Risk assessment for VTE and Flow chart
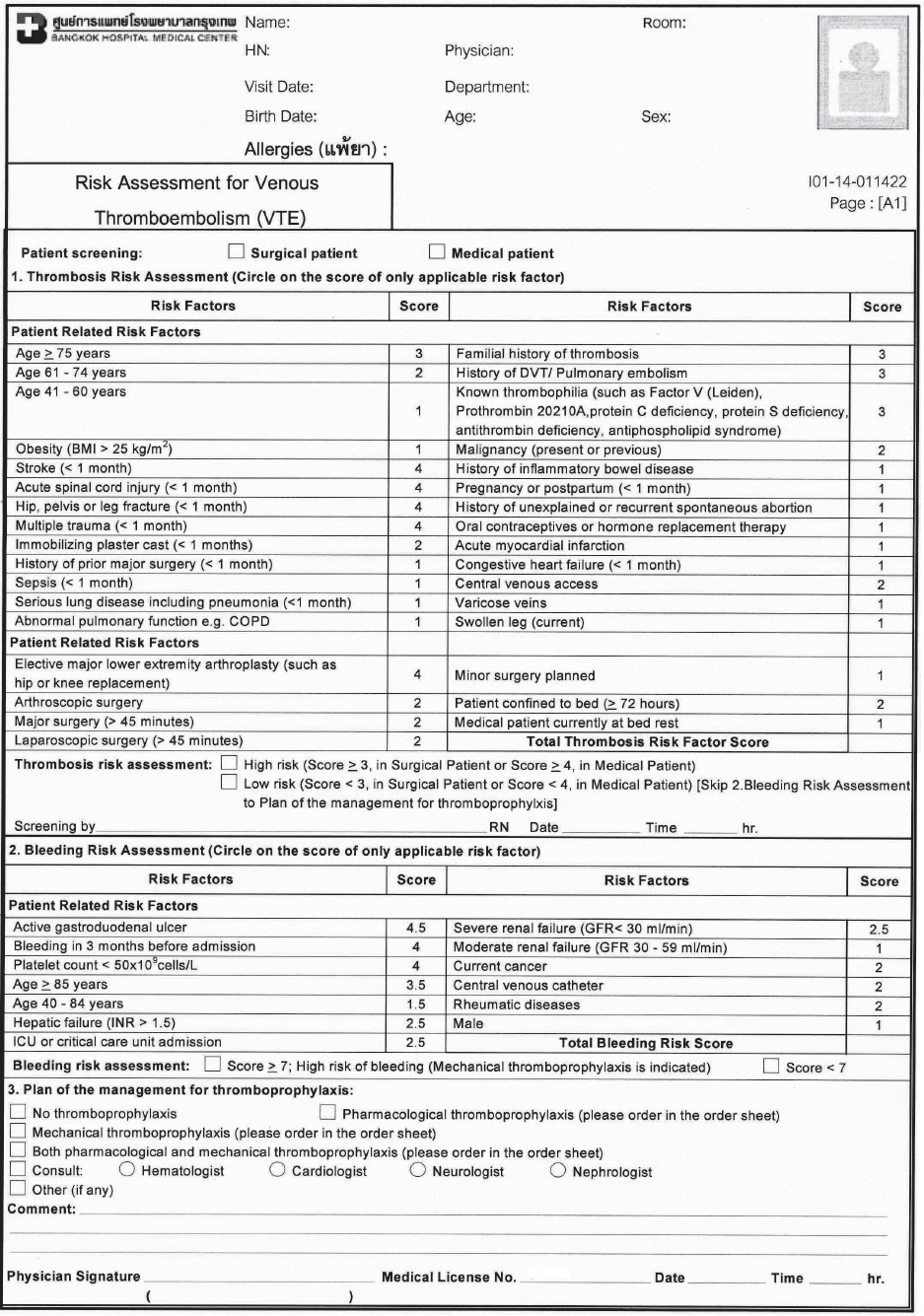
Appendix 2: Flow Chart