Neuromyelitis optica (NMO), or Devic’s disease, is a rare inflammatory and demyelinating autoimmune disorder of the central nervous system (CNS) characterized by recurrent attacks of optic neuritis (ON) and longitudinally extensive transverse myelitis (LETM) which is distinct from multiple sclerosis (Table 1).1 The first case was reported by Eugene Devic in 1894, but the discovery of a highly specific serum autoantibody (NMO-IgG) was only recently found in 2004, with a high specificity of 91% and sensitivity of 73%.1,2 This antibody is known to target aquaporin-4 (AQP4), an astrocyte water channel that is widely distributed, and this antibody is known as a pathogenesis of this disease. Patients often have relapses, which leads to severe disability and blindness.3 Magnetic resonance imaging (MRI) of the brain and spine can show typical findings of this disease. Early diagnosis is key to successful management for prevention of disability. The most appropriate treatment approach in NMO is immuno-suppression: this is effective against antibody-mediated diseases such as azathioprine, and mycophenolate mofetil.
This is a report of a middle-aged Thai female, presenting as a classic case of NMO.
A 48-year-old woman presented with a rapidly progressive left hemiparesis and numbness at left chest wall, back and left arm. There were no ocular symptoms or bowel and bladder symptoms. She had not experienced an accident or other preceding illness, including no rash and no arthritis.
Neurological examination showed grade IV/V left hemiparesis and loss of sensation at the left C2-6 dermatome distribution. She has generalized hyperreflexia with the presence of finger reflexes on both sides, but with a normal jaw jerk reflex. The tone was increased in both legs and Barbinski’s sign was present on both sides. Her cranial nerve, including optic nerve and visual function, bowel and bladder were normal.
Magnetic resonance imaging (MRI) of the brain was normal (Figure 1). MRI of cervical spine showed heterogeneous patchy enhancement and swelling of the cervical spinal cord at C2-C6 levels, with a suspected long segment of cervical transverse myelitis (Figure 2).
Table 1: Definition and characteristic of Multiple Sclerosis (MS) and Neuromyelitis Optica (NMO).1
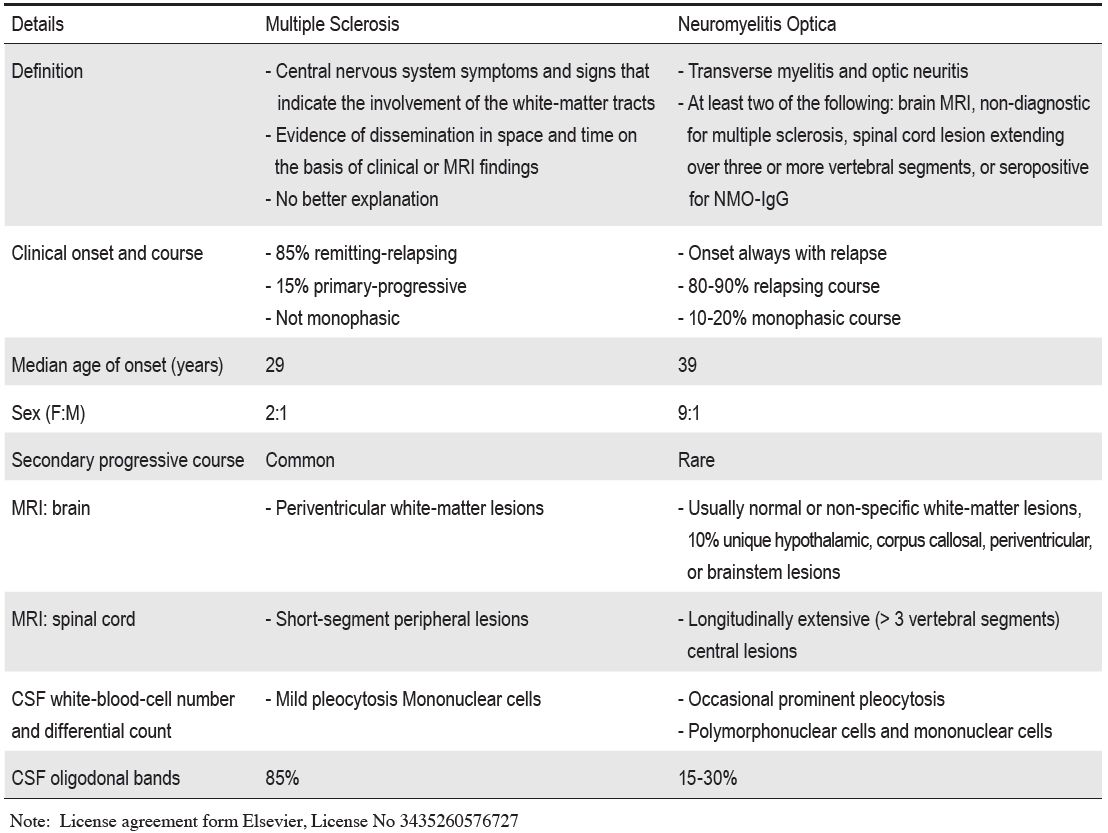
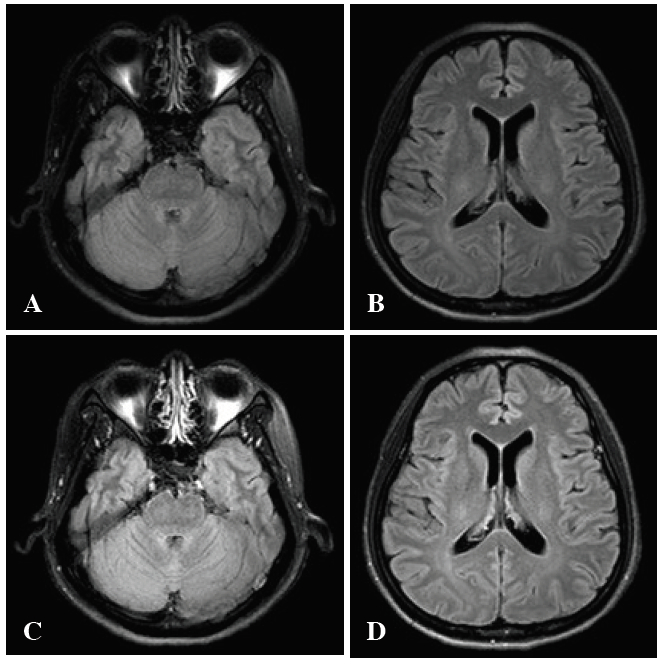
Figure 1: MRI brain T2 flair technique shows normal brain parenchyma (A,B) and post gadolinium injection reveals no enhancement (C,D).
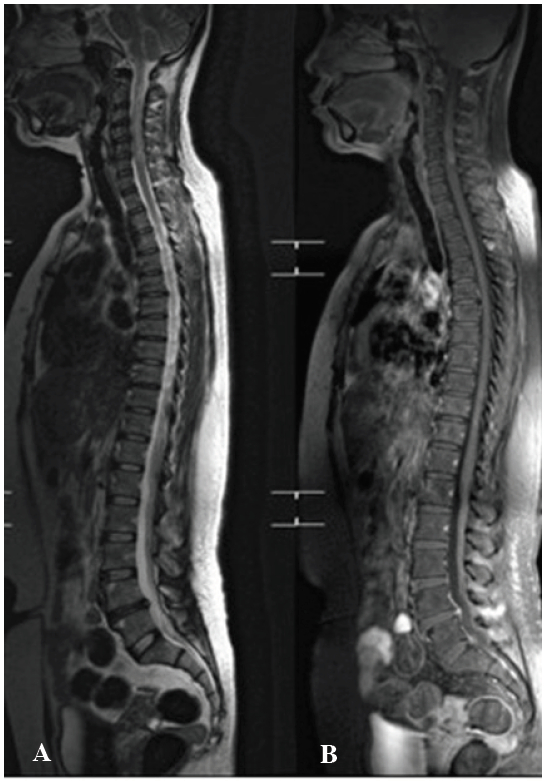
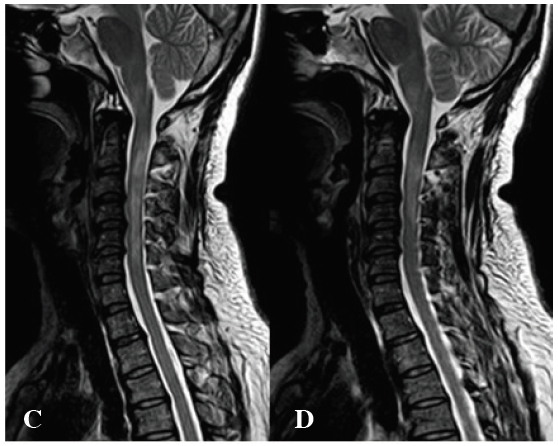
Figure 2: A, B: MRI whole spine neutral position: the sagittal T2-weight MR image shows a long segment of hyperintensity at cervical cord at level 2-6 with cord swelling.
C, D: MR image saggital T2-weight with gadolinium injection: Heterogeneous patchy enhancement and swelling of the cervical spinal cord at C2-C 6 levels, suspected transverse myelitis.
The complete blood count (CBC) results were as follows: Hemoglobin (Hb) 13.8 g/dL, white blood cell (WBC) 8,130 cell/mm3 (neurotrophil 63.9%, lymphocyte 26.8%, mono- cytes 3.9%), platelet 314,000 /mm3. Anti-nuclear factor (ANF) was 1:80, ESR was 14 mm/hr, and Anti-Ro and Anti-La were negative. A CSF oligoclonal band was negative. NMO-IgG antibody was positive.
This case demonstrated a typical clinical finding and MRI specific example of NMO. Her clinical symptoms are typical of acute cervical myelitis that rapidly progresses like a natural history of NMO. Her MRI showed a long segment of intra-axial hyper intensity on T2W with heterogeneous patchy enhancement and swelling of the affected spinal cord, which is also a typical finding of NMO. The positive NMO IgG result confirms the diagnosis. NMO affects young adults with a median onset age of 39 years. Woman are much more commonly affected. NMO is more common in Asian populations than western populations (Japanese 20-30%, Hong Kong 36% of all demyelination diseases, similar to Thailand levels, according to a study by Siriraj Hospital, Bangkok).4 The difference between MS and NMO is summarized in Table 1.1
Clinical presentation of NMO
- Optic neuritis: severe unilateral more commonly that bilateral.
- Myetitis: severe symmetrical paraplegia, and sensory loss below the lesion.
- Other: chronic vertigo, chronic hiccups, nausea, vomiting.
Patients with NMO tend to have a high chance of relapse 60% and 90% at 1 year and 3 years respectively. A criterion for diagnosis of NMO is shown in Table 2.5,6
Table 2: Revised neuromyelitis optica diagnosis criteria (2006).4,5
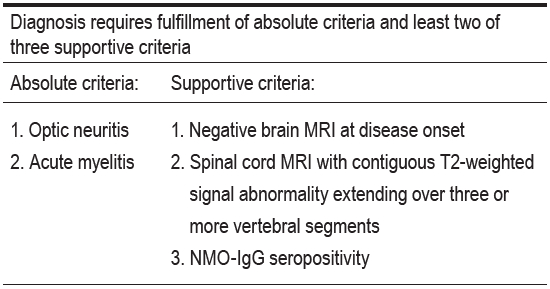

Figure 3: Spinal cord MRI in multiple sclerosis and neuromyelitis optica.
A: Sagittal T2-weighted MRI of the cervical spinal cord shows typical dorsal, short-segment signal abnormalities (arrows) characteristic of multiple sclerosis.
B: Sagittal T2-weighted cervical spinal cord MRI from a patient with acute myelitis and neuromyelitis optica shows a typical longitudinally extensive, expansile, centrally located cord lesion that extends into the brainstem (arrows).
C: On T1-weighted sagittal MRI sequences, such acute lesions might be hypointense (arrows), which might indicate necrosis and cavitation, while showing enhancement with intravenous gadolinium administration (arrowheads), indicative of active inflammation.
Note:License agreement form Elsevier, License No 3435260576727
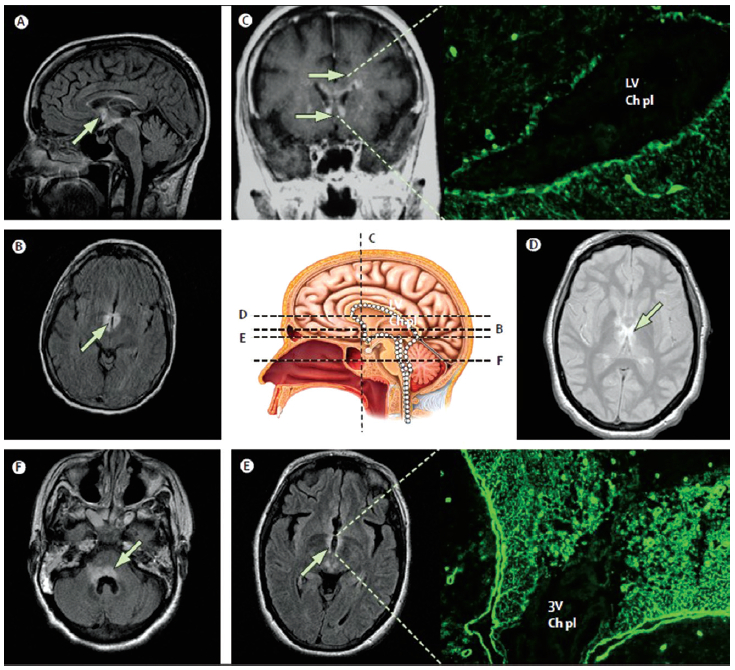
Figure 4: Brain lesions typical of neuromyelitis optica localised at the sites where aquaporin 4 expressions are normally highest. Representative MRI of three patients who are seropositive for NMO-IgG. The images show lesions in the periependymal regions of the brain; these sites are enriched with aquaporin 4 (white dots on centre picture of midline sagittal section). In the centre picture the dashed black lines show the anatomical level of MRI in the diagram; arrows show abnormality on fluid-attenuated inversion recovery (FLAIR), T2-weighted signal or after being given gadolinium. Patient 2 (image C; coronal, post-contrast T1-weighted image) has subependymal enhancement along the frontal horns bilaterally and in the adjacent white matter. The immunofluorescence photomicrograph linked to image C shows the binding pattern of the serum IgG from a patient with neuromyelitis optica in a mouse brain (400x). Intense immunoreactivity of basolateral ependymal cell membranes lining the lateral ventricle (LV) and extending into the subependymal astrocytic mesh coincides with aquaporin 4 immunoreactivity; the choroid plexus (Ch pl) is unstained. Patient 3 has contiguous signal abnormality throughout the periventricular tissues; diencephalon (image D; axial T2-weighted), third ventricle (image E; axial, FLAIR), and 4th ventricle (image F; axial FLAIR). Immunofluorescence photomicrograph linked to image E shows the binding pattern of the serum IgG from a patient with neuromyelitis optica in a mouse brain (400x), with intense staining of periventricular tissues (3rd ventricle, 3V); choroid plexus (Ch pl) is unstained image C is courtesy of Allen Aksamit, Mayo Clinic College of Medicine.
Note: License agreement form Elsevier, License No 3435260576727
Typical presentations of spinal cord MRI abnormalities in NMO include a longitudinally extensive intra-axial lesion, characteristically spanning over 3 or more contiguous vertebral segments, as shown in Figure 3.1 In contrast to MS, the brain MRI of patients with NMO is usually normal or shows non-specific white matter lesions. Nevertheless, in some NMO cases, typical abnormalities of the brain at the hypothalamus, corpus callosum, periventricular area (area postrema), or brainstem can be seen (Figure 4).1
CSF analysis
Prominent CSF pleocytosis with a high proportion of neutrophil can be seen. CSF oligoclonal band is present in only 15% of cases, which is much lower than in MS (80% of cases). ANA can be detected in 53% and antibodies to extractable nuclear antigen (primarily anti- Ro, anti-La) in 17%.7
Treatment
Intravenous corticosteroid therapy is commonly used as an initial treatment. Patients who do not respond may undergo plasmapheresis. Maintenance immunosuppressive therapy is generally used to reduce the relapse of NMO, of which, azathioprine (2.5-3mg/kg/day), mycophenolate mofetil, rituximab ,mitoxantrone and prednisolone may be used.8
NMO is a severe, disability disease that primarily affects middle-aged working females. Early and correct diagnosis is of the highest importance. The NMO-IgG test is very specific and useful in diagnosis and is now available in Thailand. Early immunosuppressive therapy is recommended.