Transient global amnesia (TGA) is a disorder characterized by a sudden attack of severe anterograde amnesia, where patients are unable to learn and recall novel information during the event. Although first described at least 60 years ago,1 the etiology and pathophysiology of TGA remain unclear and have been a matter of debate among clinicians and researchers. In this paper, we present a case of TGA with typical MRI findings and thereview of literature.
A 38-year-old, right-handed, Thai lady, without significant past medical history, presented to the Neuroscience Center of Bangkok Hospital Medical Center with a sudden onset of transient memory loss. Her symptoms occurred on the morning of the same day of the hospital visit. After sending her daughter to school and driving back home, the patient suddenly could not remember what was going on, and repeatedly asked the same questions. She was able to remember her name and her husband. Her language was not disturbed during the event. She denies headache, dizziness, or vertigo associated with this spell. There were no other focal neurological deficits. There were no witnessed abnormal movements of the face, lip smacking, or fidgeting of the hands and feet. The symptoms lasted for approximately two hours before her memory gradually came back. The patient could not remember the entire spell. She denies prior similar symptoms. She denies the history of recent head injury or any stressful events.
On examination, the patient was alert, awake, and oriented to time, place, and person. She appeared anxious and frustrated as she could not remember what happened during the event. Her concentration, memory, repetition, naming, reasoning and executive functions were all intact. There was otherwise no focal neurological deficit. Her vital signs were all within normal ranges.
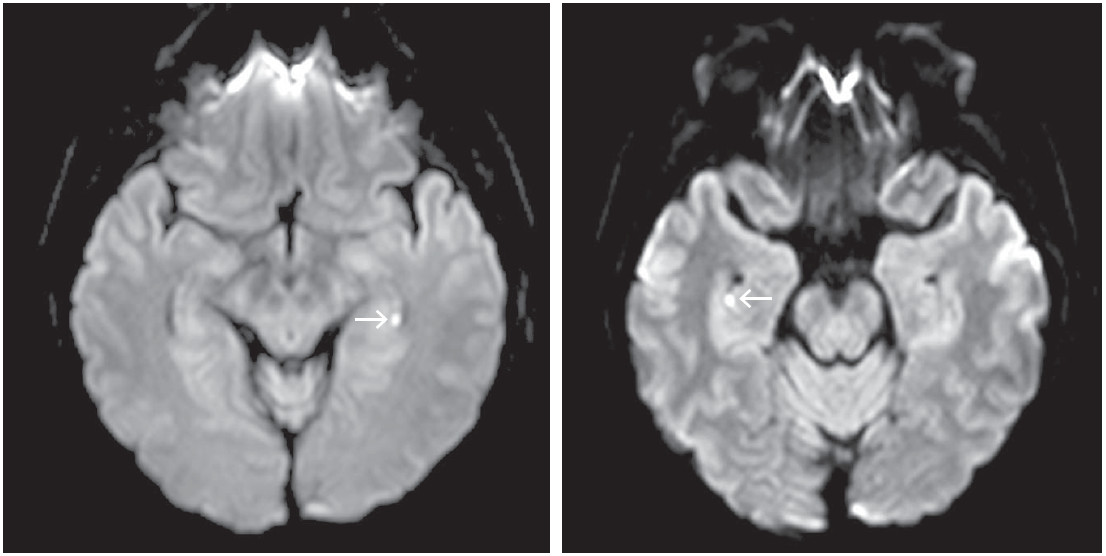 Figure 1: The MRI diffusion weighted imaging (DWI) showed small punctuate hyper-intense lesions in the CA1 area of the bilateral hippocampi. (b value = 1000 s/mm2, 2-mm slice through the hippocampus, performed at approximately 12 hours after symptom onset).
Figure 1: The MRI diffusion weighted imaging (DWI) showed small punctuate hyper-intense lesions in the CA1 area of the bilateral hippocampi. (b value = 1000 s/mm2, 2-mm slice through the hippocampus, performed at approximately 12 hours after symptom onset).
 Figure 2: The MRA of the brain was unremarkable.
Figure 2: The MRA of the brain was unremarkable.
 Figure 3: The MRV of the brain revealed hypoplasia of the left transverse and sigmoid sinuses, which could be a normal variation.
Figure 3: The MRV of the brain revealed hypoplasia of the left transverse and sigmoid sinuses, which could be a normal variation.
Blood chemistry revealed fasting blood glucose of 81 mg/dL, HbA1c of 4.9%, total cholesterol of 195 mg/ dL, triglyceride of 107 mg/dL, HDL-C of 90 mg/dL, and LDL-C of 96 mg/dL. 12-lead EKG showed a normal sinus rhythm of 67 beats per minute without other pathological findings.
The patient underwent electroencephalography (EEG) which was within normal limits. MRI, MRA, and MRV of the brain were obtained (Figures 1-3), which revealed two small foci of restricted diffusion at the bilateral hippocampal bodies; otherwise the studies were unremark- able.
The patient in our case meets the strict diagnostic criteria for transient global amnesia, which was proposed by Hodges and Warlow as follows:2
When the patient fulfills the definite diagnosis for TGA, the outcome is usually excellent. The rate of subse- quent major vascular event is less than 1% per year,2 and in most patients (more than 90% of cases), TGA occurs only once in their lifetime.3
Given the temporary nature of this disorder, TGA is often hypothesized to be caused by transient cerebral ischemia, epilepsy, migraine,4 as well as venous congestion due to retrograde venous cerebral blood flow.5 However, none of these pathophysiological theories is convincing as the relapse rate of such conditions are significantly higher than that of TGA.6 Additionally, most of the initial studies found no significant difference between the brain imaging of TGA patients and normal control.2,7
An MRI study in 1999 by Grass and colleague8 in patients with acute TGA (performed within 8 hours of symptoms resolution) found no evidence of hyperintensity on diffusion-weighted (DW) images or hypointensity on apparent diffusion coefficient (ADC) maps that would imply decreases of water mobility or acute T2 changes. However, when the study by the same group was modified in order to serially investigate TGA patients using DW images performed on the day of symptom onset through days 1 and 2, more than 80% of the patients developed a small, punctate, unilateral or bilateral DW MRI lesion in the lateral aspect of the hippocampal formation (pes and fimbria hippocampi).9 Such findings have been confirmed by several subsequent studies.10-12 Since lesions were rarely detected in the hyperacute phase, and most became noticeable within 48 hours, this may explain why many prior studies did not reveal significant abnormalities in neuroimaging of TGA patients.9 Follow up brain MRI is recommended several days later when no lesion is detected by DW images within 24 hours after onset.11
Although diffusion restriction is often associated with ischemic stroke representing a zone of irreversible damage, several studies showed that hippocampal lesions in TGA patients completely resolve without structural sequelae.10,12 In addition, there is no significant difference in long-term cognitive performance and psychological outcomes between patients with and without DW restriction as well as compared to healthy control.6 Moreover, the frequently delayed onset of the lesions is not consistent with the abrupt nature of cerebral ischemic events. There- fore, the DWI restriction in TGA may not result from similar pathophysiology to that of an acute cerebrovascular accident.
There are certain personality traits and psychological comorbidities that have been suggested to be more common in TGA. For example, Inzitari and colleagues found that TGA patients scored significantly higher than the control group on a scale that measured phobic attitude.13 According to an analysis by Quinette et al, TGA episodes in women are associated with an emotional precipitating event, a history of anxiety and pathological personality traits, suggesting that psychological factors are of particular importance in TGA.14 Griebe and colleagues showed that patients with prior TGA has a hypersensitivity of the hypothalamic–pituitary–adrenal (HPA) axis, which can result in a significant elevation of the glucocorticoid level during an acute stress event, affecting the function of the hippocampus on a cellular level.15 Thus, recent hypothesis suggests that TGA might result from a stress-related temporary inhibition of memory formation in the hippo- campus by means of a selective vulnerability of CA-1 neurons to metabolic stress.16
Transient global amnesia is a disorder characterized by an attack of temporary anterograde amnesia with no other focal neurological symptoms. Recent studies showed that the characteristic MRI findings of this disorder are small punctuate diffusion restricted lesions in the CA1 area of the hippocampal formation. The onset of such findings can be delayed up to 48 hours after the symptom onset: therefore, serial MRI may be helpful.