Klebsiella related liver abscesses can occur at a primary site and are most likely monomicrobial.1-3 The virulent strains of K.pneumoniae are able to invade a normal liver paren-chyma without underlying hepatobiliary diseases, intra-abdominal infections, surgery, trauma or colorectal diseases.4 Most cases have been reported from Asian countries.5 A polymicrobial liver abscess is usually secondary to other intra-abdominal infections.1,6 We report a case of a Klebsiella-associated liver abscess, presenting only with high fever.
A 51-year old Thai male presented to the emergency depart- ment with high fever and chills six hours prior to admission. His past medical history was significant for only hyperlipidemia and hypertension. Physical examination revealed mild scleral icterus and a temperature of 40oC. Other findings were unremarkable. Laboratory tests were pertinent for a leukocytosis (11,630 cells/ mm3), neutrophil predominance (86%), hyperbilirubinemia (2.2 mg/dL), aspartate transferase 121 U/L, and alanine transferase 176 U/L. Dengue NS-1 antigen and influenza screening test were negative. Presepsin levels were found to be elevated at 1,831.0 pg/ mL (< 300.0 pg/mL) and this aided in the differentiation between bacterial versus non-bacterial infection.
The patient was started on intravenous ceftriaxone. Hemoculture grew Klebsiella pneumonia (K. pneumonia) sensitive to all antibiotics except amoxicillin-clavulinate. Computed tomography (CT) of the whole abdomen was performed to evaluate the primary source of bacteremia. Localized hypoattenuation at the hepatic angle with no linear appearance was seen in the non-contrast study (Figure A), while contrast study revealed a localized hypoattenuation lesion 2x3 cm with rim enhancement associated with linear hypoattenuation appearance proximally (Figure B, C). This finding was suggestive of liver abscess. Percutaneous drainage was not performed due to the size of the lesion. His fever gradually subsided and the patient was clinically improved after the first few days of antibiotic treatment. Presepsin levels subsequently declined to 498.0 pg/mL. The antibiotic was later switched to oral levofloxacin after 14 days of IV ceftriaxone. At the 28 day-follow up, the presepsin level had further dropped to 235.0 pg/mL. The follow-up CT scan (Figure D) revealed complete resolution of the previously seen lesion. The disappearance of the linear attenuation observed on the initial CT study is due to hepatic venous thrombophlebitis, which is simulated as a small dilated intrahepatic duct.
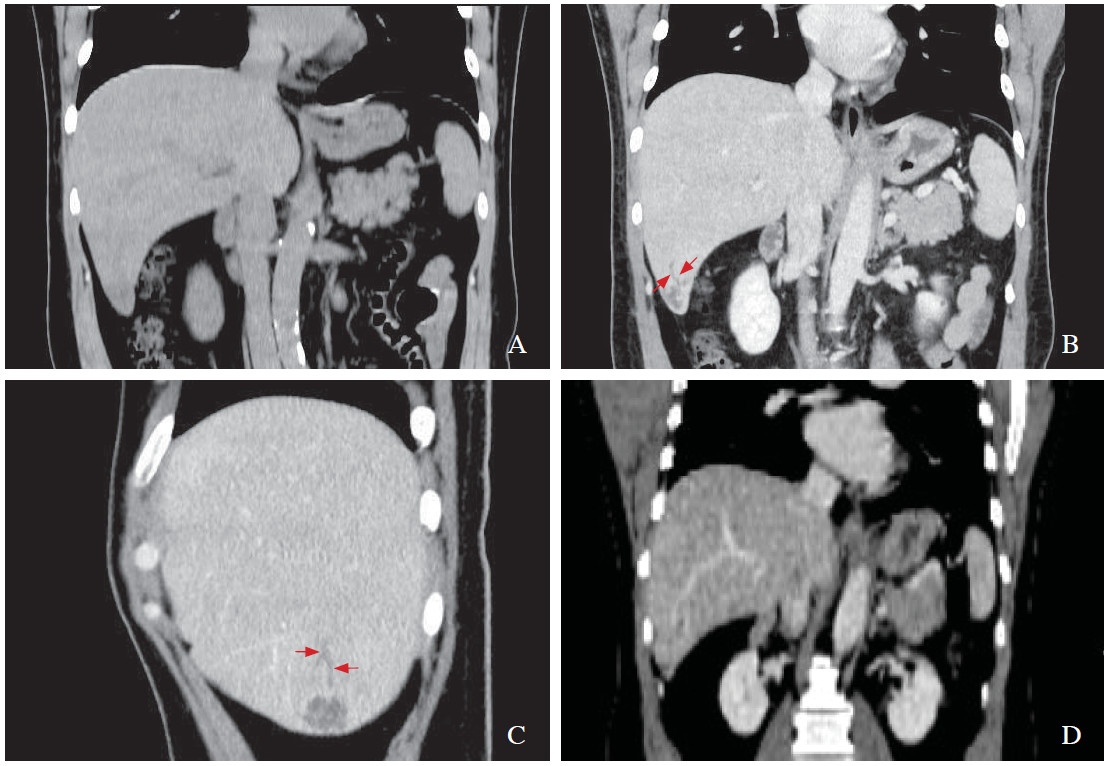
Figure A: CT coronal section without contrast enhancement reveals localized hypoattenuation near hepatics only.
Figure B-C: CT coronal and sagiital sections with contrast enhancement reveals rim contrast enhancement and linear hypoattenuation radiating towards medially on delay phase with is due to hepatic venous thrombophlebitis (see arrows).
Figure D: CT coronal section on delay phase 28 days after treatment reveals disappearance of all mass and linear hypoattenuation.
Monomicrobial pyogenic liver abscess caused by K.pneumoniae occurs in a patient without underlying hepatobiliary tract diseases, colorectal diseases or pre-existing intra-abdominal pathology. It has been found to be associated with Asian ethnicity, diabetes and middle- to-older-aged patients. The common presenting symptom is acute febrile illness, while only one-half of cases presents with more specific clinical clues such as right upper quadrant pain, jaundice and hepatomegaly.
The symptom of high fever may be due to bacterial or non-bacterial infection, which needs to be differentiated urgently. The novel sepsis biomarker that has recently been made available is presepsin. Soluble (sCD14) or presepsin is the free fragment of a glycoprotein expressed on monocytes and macrophages. As a receptor of the lipopolysaccharide-lipopolysaccharide binding protein (LPS-LBP) complex, CD14 can activate a series of signal transduction pathways and inflammatory cascades in the setting of bacterial infection (sepsis), and leads to systemic inflammatory response. If the level is higher than 300 pg/ mL, systemic bacterial infection (sepsis) should be consid- ered. In the range of 500-1000 pg/mL, moderate and severe sepsis is suggestive. For this patient, presepsin was 1,831.0 pg/mL on the first day of admission. Presepsin was superior to procalcitonin (PCT) in early diagnosis of bacterial sepsis. Compared with PCT, presepsin increased earlier and faster in patients with sepsis, at 2 hours after infec- tion in the cecal ligation and puncture (CLP) sepsis model, peaked at 3 hours, and declined at 4-8 hours.7,8 However, there was no difference between levels of presepsin and sepsis severity.
To identify the source of infection, it is important to perform an abdominal CT with contrast enhancement as this shows the hepatic mass with rim contrast enhancement and linear hypoattenuation radiating towards medially only on delay phase. This finding is likely to occur due to a liver abscess with hepatic venous thrombophlebitis. This finding is not a dilated intrahepatic duct because in non-contrast enhancement there was no demonstrable; hence cholan- giocarcinoma peripheral type is excluded.
K. pneumoniae causing pyogenic liver abscesses are now seen as an emerging pathogen with clinical significance. The risk factors are diabetes, cancer, impaired host defenses, and glucocorticoid therapy. This syndrome occurs almost exclusively in Asia, possibly due to a distinctive virulent strain. The chief complaints usually include high fever, nausea, vomiting, and right-sided upper abdominal pain. This report presents this case to increase awareness among physicians for accurate management and investigation of this condition. We suggest the use of presepsin to aid in early diagnosis of bacterial sepsis.