Hip dislocation after total hip arthroplasty can be classified into anterior and posterior dislocation, and immediate post-op and late dislocation. The most common dislocation is posterior dislocation which depends on a primary surgical approach because the resection of the posterior capsule takes part in the direction of hip dislocation. However, surgical technique, components orientation and soft tissue tension have a major role in hip stability. We report a case of a 52-year-old man who suffered from an unstable hip after having a normal hip functional score for 13 years without any traumatic events. Radiographic findings did not show any sign of loosening or radiolucency. The causes of late hip dislocation and treatment are also described.
A 52-year-old man who worked as a flight attendant developed chronic right hip pain for 13 years with a diagnosis of avascular necrosis of the right femoral head. After the efforts of many conser- vative treatments for 6 months, the pain was in progression. The first surgeon decided to do a femoral head decompression. After the surgery, he could not walk well, and had slipped and fallen down many times. Then a derotation proximal femoral osteotomy was further performed. However, the patient developed uneven pain occasionally and later progressed to constant pain on his right hip. He decided to seek a second opinion. The x-ray showed segmental collapse of the right femoral head with a normal left hip. Total hip replacement (THA) was performed with Sportono acetabular cup and stem with 28mm Metal-on-Metal (MoM) articulation. After the successful operation, the patient could go back to work on board. He could sit low into a squat position and stand upright normally. He had a very active normal life with full functional score for 13 years after the right THA.
One and a half years later, he felt a clunk inside his right groin with minimal pain. He could do hip reduction by himself. There were about 8-9 times in a year that he had hip subluxation and spon- taneous reduction. The most common position when he sensed the clunk was sitting with the right hip crossing the leg with the knee in flexion and a fully external rotation. He did self reduction by standing up and turning his foot in internal rotation.
One month ago, when standing up from a chair, he immediately felt severe pain in his right hip. Without any traumatic event, at that time he could not do self reduction. Then he was brought to the hospital. The x-ray confirmed that he had right hip prosthesis dislocation. Closed reduction under general anesthesia was successfully done without difficulty and it was stable at 75-80 degrees of flexion without any dislocation. The pre-operative x-ray showed hip dislocation and the post-operative x-ray after reduction at 75-80 degrees of flexion demonstrated normal position of the right femoral head dislocation (Figure 1). Despite successful hip reduction with some degree of stable hip, the patient still felt very unconfident with his right hip, he was afraid that if his hip dislocated again while he was working on board, it would be very painful and no one could do hip reduction for him.

Figure 1A: Nontraumatic anterior hip dislocation fully exposed lesser trochanter in external rotation. Femoral stem and cup shell were still well fi xed without any sign of osteolysis.

Figure 1B: After close reduction head was well seated into metal liner, both leg lengths were equal. Soft tissue tension was proper after telescoping test.
Approaching and Pre-operative Planning
According to the history of subluxation and the inci- dence of dislocation after having normal function after 12 years post THA, a critical analysis of the post reduction x-ray was done. There was no sign of component loosening in both acetabulum and femoral stem components. Femoral component position was normal without any sub- sidence. Acetabular cup had about 65 degrees abduction angle with no excessive abnormal rotation. No positional change was detected. Considering that hip dislocation was not immediately post-operative event, but happened 13 years later, the high abduction cup angle should not be the major cause of this late hip dislocation. From the x-ray, both legs were equal in length so we could expect that soft tissue tension was normal and should not be the cause of hip dislocation in this patient.
After a meticulous study of the x-ray, we could detect a small change on the x-ray and this was a very important point that led to the definitive treatment. In Figure 2, the arrow sign shows the evidence of migration of metal liner over polyethylene liner. However, we could not evaluate the status of the locking mechanism between polyethylene and metal back shell. It might be broken already and this was not known until we were in the operative field. The positional change in metal liner that changed the degree of anteversion can explain why he had late hip dislocation.

Figure 2: From a careful analysis on the post reduction x-ray, elevated metal liner was seen at the inferior junction of metalpolyethylene liner interface.
During the pre-operative preparation, Metasul liner had stopped marketing and there had been no more implant stock in Thailand for 8 years, so the order for these liners from Switzerland had to be done. From the x-ray, the metal shell was a Spotorno cup and the distributor still had the equipment available.
Duringthe operation, the patient wasplacedinthelateral decubitus position. A lateral curvilinear over greater trochanter incision was done. Tensor fascia lata and previous fibrous tissue were split. Short external rotators were cut step by step then a posterior capsulotomy was performed. The femoral component was well fixed. Soft tissue and granulation tissue with very little metallosis around the acetabular cup were removed as shown in Figure 3. Then the liner was removed from the metal shell by using a special removal instrument twisting in an anti-clockwise direction, as shown in Figure 4 and 5. The spiral lock mechanism was checked and found that the locking system was still in good condition. New polyethylene was inserted into the spiral lock by a clockwise twist. The femoral head was then reduced and hip stability was tested. Closure of the wound was per- formed layer by layer with a vacuum drain inserted. The next day after surgery, the patient was allowed to have a full weight bearing walk with axillary crutches. He was discharged after 4 days of hospital admission and con- tinued receiving physical therapy. After 1 month, he went back to work for the airline.

Figure 3: Shows a small amount of necrotic tissue around the impingement area. Very little metallosis is detected.

Figure 4A: Spotorno metal shell cup and liner.
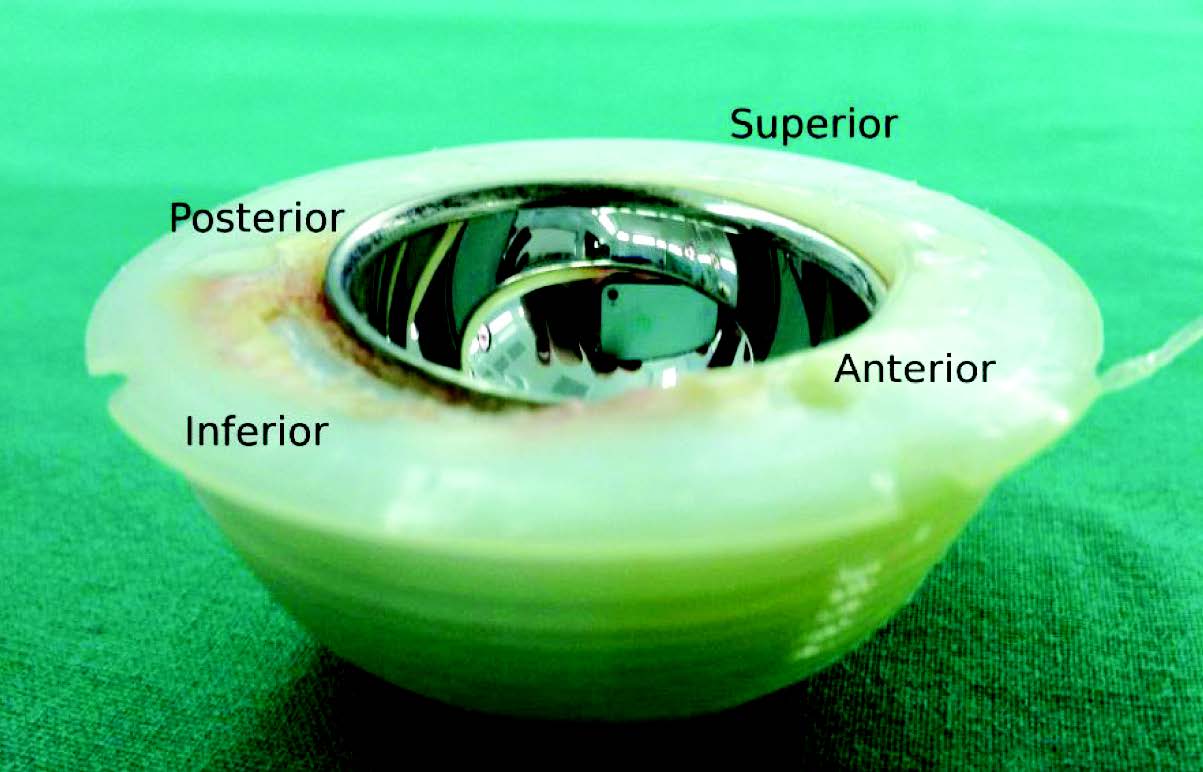
Figure 4B: Extracted Metasul liner shows inferior polyethylene surface with laminated wear. The change of metal liner position means polyethylene and metal liner disintegrated; however, they are well fi xed together. The metal liner at anterosuperior is sunk. In the opposite direction, the posteroinferior border of metal liner is elevated.

Figure 5: The back of the liner does not show wear out of locking mechanism. A small piece on the right of the liner comes from the extraction procedure.
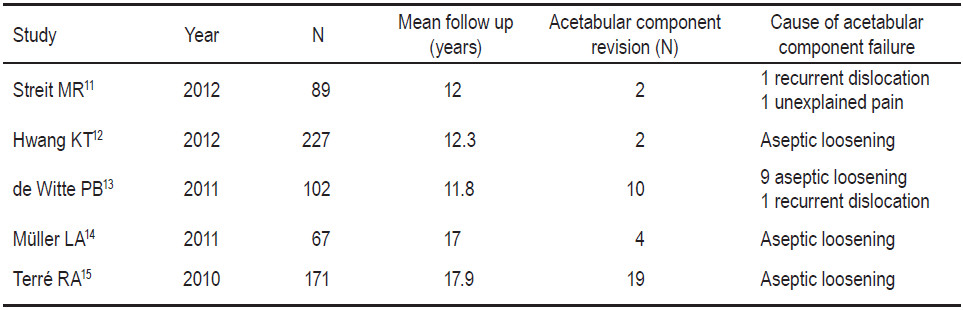
Table 1: Report of the number and causes of acetabular component revision
Metal-on-metal (MoM) bearings in hips is not a new concept. Many long-lasting, successful cases more than 20 years with MoM were reported in several studies such as McKee-Farrar’s prosthesis1,2 and Peter Ring’s prosthesis.3 However, MoM was not popular because of the higher failure rate when compared to metal-on-polyethylene bearing (MoP). The major causes were big head and big neck designs that follow the design concept of Austin Moore prosthesis, so these designs could easily make impingement with the metal cup. One of the other causes was that metallurgy technology and quality control during that time were not as good as those at present. MoM hip with Metasul liner is the only 28mm head articulate with composite metal-polyethylene liner on the market that had a very successful track record,4,5 especially when used with cementless acetabular and stem.6 Spotorno cup is a cementless cup that was introduced and implanted in 1985. This special design features the basic conical shape and the large surface area of the self-tapping thread lamellae that give the cup excellent properties in terms of primary stability, biomechanics and secondary stability without press-fit or screw fixation.7
The cup placement in this case was 65 degrees abduction (Figure 2). Surgical technical limitation was a major cause in this vertical alignment. These constraints included the inadequate medial reaming and the cup placement which relied on the superolateral rim of the acetabulum. Retrospectively, if the surgeon just did more medial reaming, the abduction angle would be 40-45 degrees. In the case that abduction angle is more than 55 degrees, wear rate would increase up to 10 times within 5 years of implantation when compared to abduction angle at 45 degrees.8 However, this patient used metalsul liner that was 28mm head MoM. The intra-op- eration findings showed very little metalosis (Figure 3). This evidence was correlated with the x-ray findings at 13 years postoperation, where there was no radiolucency or loosening signs in both femoral and cup shell components.
If this case used nearly anatomical head size such as hip resurfacing or big head MoM THA, worse results would be expected from high metal wear because in the high abduction angle cup, the fluid lubrication phenom- enon would not occur but the boundary contact would happen instead.9 The high level of metal ion production would have subsequent results of pseudo-tumor, early osteolysis and finally component loosening. A small- er head, like a 28mm head even in a normal abduction angle will not show the fluid lubrication phenomenon because it will perform much better when the diameter of a metal cup is more than 50mm (metal head size more than 44mm).10 The evidence from these findings also supports that the smaller 28mm head MoM like Metasul tolerates volumetric wear better in a high abduction cup angle when compared to a big head MoM. On the other hand, metalsul does not rely on the fluid lubrication phenomenon and the boundary contact wear is lower in the small head metalsul than in the big head hip resurfacing.
There are studies reporting the failure of the acetabular cup in the Spotorno system. Most of them are aseptic loos- ening (Table 1). To our current knowledge, there is no report of the mode of failure like this case. The major cause of failure in this case was the impingement that resulted in hip dislocation. Even the cup abduction angle was too high but the anteversion was also low which provided stability of the artificial hip along 12 years of usage.16 However, the high cup abduction angle also produced impingement at the an- teroinferior sector of the cup especially when this patient worked in a squatting position on an airplane. This impinge- ment force was not strong enough to make the metal cup shell immediately change its position because of the very strong initial bonding developed from the conical thread design of Spotorno and also the good bonding between the liner thread and inside the metal cup shell (Figure 5). When repetitive impingement happened again and again from routine airline work with a squatting position, the weaker de facto bonding between the inside metal liner and the outer polyethylene liner was dissociated. The anteroinferior sector of the inside metal liner changed its position and sunk beneath the polyethylene liner. The repetitive impingement still happened; however, it impinged on the anteroinferior polyethylene liner instead of the metal liner because the metal liner had already sunk. This was why the laminated polyethylene wear was found at the anteroinferior sector in the same direction as the sinking metal liner. This anteroinferior defect was the cause of an unstable anterior hip dislocation in this patient. Fortunately, changing the inside metal liner was detected at the x-ray as in Figure 2. The appropriate pre-operative planning was prepared from this little change in the x-ray findings.
In conclusion, the major cause of the 13-year-later dislocation in well fixed cementless Spotorno total hip arthroplasty system in this case, was the anteroinferior impingement that later made an anterior defect. Despite the very high vertical cup placement (rim loading), there was no sign of massive metal wear in the standard head (28 mm) MoM bearing surface. This indicates the successful MoM articulation in a young active patient. A spiral thread design at the back of the Spotorno and at the polyethylene liner to the metal shell interface provide very high stable bonding both initially and subsequently.
Conflict of interest statement
The authors claim no conflict of interest associated with the manuscript.