Kawasaki disease (KD) is an acute febrile vasculitic syndrome of unknown etiology that occurs predominantly in infants and young children. The disease has also been called mucocutaneous lymph node syndrome or infantile periarteritis nodosa. Affected children present with high fever, rash, conjunctival injection, inflammation of the lips or oral cavity, cervical lymphadenitis, erythema and edema of the hands and feet. Cardiac sequelae, the most potentially life-threatening complications include coronary artery aneurysms or ectasia which can occur in up to 15-25% of untreated patients and may lead to myocardial infarction, sudden death, or ischemic heart disease.1
A 2 years 8 month-old Thai boy who previously had been in a healthy state, presented with a high fever of 40 °C, red eyes, rash on both palms, both lower extremities and soles swollen. No evidence of oral mucosa change or cervical lymphadenopathy detected. He was admitted to another hospital on day 3 of fever for investigation and symptomatic treatment. Empirical antibiotics were administered and results for dengue, influenza and mycoplasma were pending. Since admission, patient remained highly febrile and did not respond to antibiotics. On day 5 of fever, he became hypotensive with a blood pressure of 70/40 mmHg, poor perfusion and was transferred to intensive care unit (ICU) to receive intravenous fluid resuscitation and inotropic drug support under clinical impression of septic shock. His transfer to Bangkok hospital was arranged by the pediatric intensivist team for further investigation and treatment.
Physical examination
Vital signs showed BP 80/50 mmHg, pulse 140/min, temperature 38.5 °C and respiratory rate 30/min. Patient appeared cranky but consolable. The body weight was 14 kilograms, body surface area 0.58 m2. There were positive findings for bilateral nonexudative conjuntival injection, dry cracked lips, erythematous macular rash on both lower extremities and marked swollen erythema over the feet. Otherwise unremarkable.
Investigations
Complete blood count (CBC) revealed anemia and thrombocytopenia. Hb 9.2 g/dL, WBC 13,950 cell/mm3 with 70% of neutrophil and 21% of lymphocyte, no band form, platelet 170,000 cell/mm3. Elevation of inflammatory markers with erythrocyte sedimentation rate (ESR) 57 mm/hr and C-reactive protein (CRP) 158 mg/L. Liver function test revealed hypoalbuminemia 2.8 g/dL with normal SGOT and SGPT. Urinalysis showed evidence of pyuria with WBC 10-20/HPF. Normal serum lactate level 1.5 mmol/L. Abnormal coagulogram showed PTT 33 second (sec), PT 14.1 sec, TT 14 sec and elevated FDP D-dimer 3,118 microgram/L FEU (Fibrinogen equipment unit). Blood and urine culture were negative, as well as tests for dengue virus, influenza virus and mycoplasma.
Electrocardiogram (Figure 1) revealed sinus tachycardia at 156/min. There was flattening of T wave in all precordial leads. No abnormal Q wave. Initial echocardiogram revealed normal coronary artery dimension with left main coronary artery (LMCA) 3 mm, left circumflex artery (LCX) 2 mm and right coronary artery (RCA) 2 mm. Left ventricular (LV) systolic function was mildly decreased with ejection fraction (EF) 50-55%. There was mild mitral regurgitation and small pericardial effusion. Small right and left pleural effusion was also noted.
Hospital course
A diagnosis of Kawasaki disease shock syndrome (KDSS) was given to this patient after the reviewing all clinical findings and investigations. While the patient was being given dobutamine for inotropic support, intravenous immunoglobulin (IVIG) 2 grams/ kilogram was commenced on day 6 of fever. Fresh frozen plasma was given due to abnormal coagulogram. Patient’s hemodynamic status had improved and he finally came off dobutamine. High dose aspirin was introduced after patient started oral intake. His temperature returned to normal after finishing IVIG and remained normal for another 48 hours. On day 3 of admission, he was discharged home with a high dose aspirin. Twenty-four hours after discharge, he became febrile again with temperature of 38.7 °C. The repeated physical examination revealed bilateral non-exudative conjunctival injection. Others were unremarkable. Repeated CRP 72 mg/L, ESR 70 mm/hr. Repeated echocardiogram revealed ectasia of LMCA 3.7 mm (Figure 2) , LCX 2.2 mm and RCA 2.3 mm. LV systolic function was normal with EF 65%. There was a small pericardial effusion, which was unchanged from previous study.
A second dose of IVIG at 2 grams/kilogram wasadministered due to recrudescent fever > 36 hours after completion of the initial IVIG infusion. Patient had no reaction to the second dose of IVIG and was observed closely and his fever initially abated. However at 48 hours after second dose of IVIG, he had recrudescent fever at 38.7 °C. Repeated physical examinations neither revealed any evidence of occult infection nor evidence of systemic inflammatory disease. Screening tests for autoimmune disease were also negative. Due to failure of response of 2 doses of IVIG, Infliximab 70 mg was administered intravenously according to the drug protocol. There was no reaction from Infliximab and patient’s temperature remained normal for the next 72 hours. Patient was again discharged home with a high dose aspirin. Repeated echocardiogram 6 months (Figure 3) after onset of disease revealed resolution of LMCA ectasia 2.5 mm with normal left ventricular systolic function.
Kawasaki disease (KD) is now the leading cause of acquired heart disease in children both in developing and developed countries.1 Diagnosis of KD can be straightforward if patient’s clinical findings have been matched to clinical criteria or can be delayed if patient’s clinical findings have not been presented accordingly (incomplete KD). The most common clinical features of KD are high, intermittent fever of at least 5 days and the presence of at least 4 of the 5 following clinical features namely;
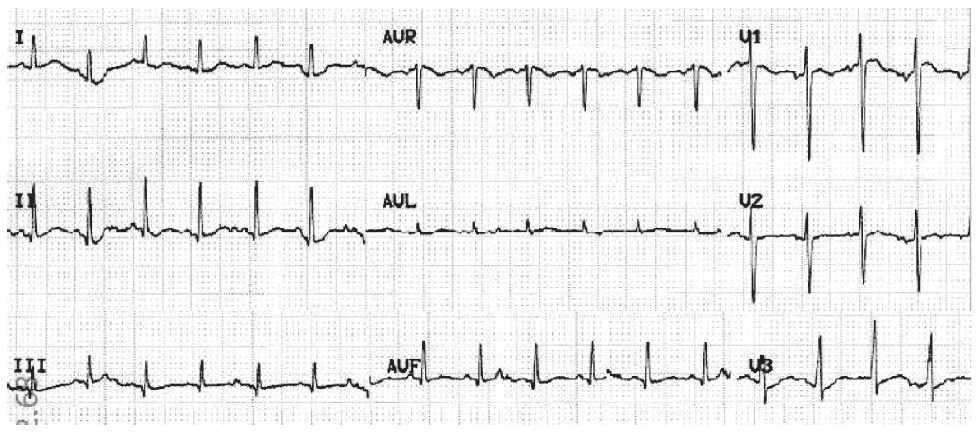
Figure 1: Pediatric Electrocardiogram showed sinus tachycardia rate 156/min., abnormal ST-T changes and no abnormal Q wave.
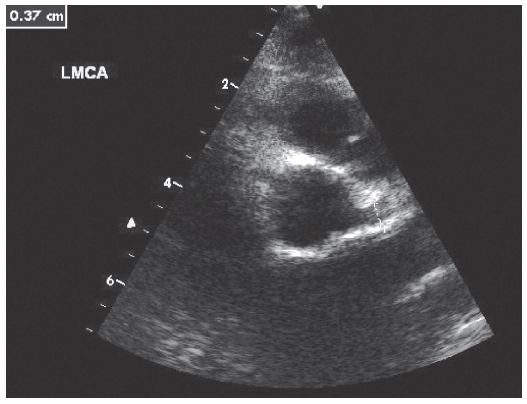
Figure 2: Before treatment: ectasia of left main coronary artery, measured 3.7 mm in diameter
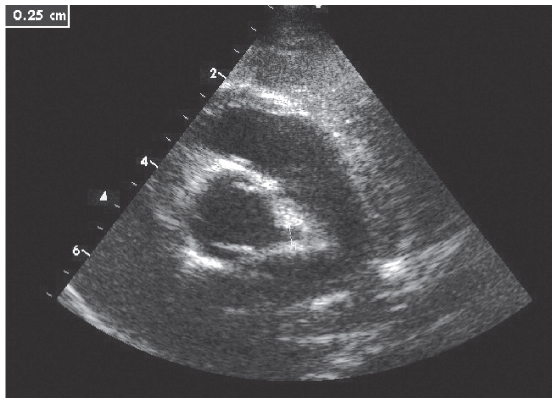
Figure 3: Repeated echocardiogram 6 months after onset of disease revealed ectasia of left main coronary artery, measured 2.5 mm in diameter
Our patient had fever for 6 days including eyes, lips, extremities changes and rash. Supporting laboratory findings included elevated ESR and CRP, anemia, hypoalbuminemia and sterile pyuria. One of the striking features presented in this patient is shock with evidence of vascular leakage. Hemodynamic instability has been reported during IVIG infusion due to allergic reaction, which did not present in our case because he had hypotension before infusion of IVIG. The occurrence of hemodynamic instability unrelated to IVIG adverse affects during the acute phase KD is uncommon unless the patient has significant cardiovascular involvement for KD, such as severe myocarditis or cardiac tamponade from rapidly developing pericardial effusion, which was also not the case for our patient.
Kanegaye et al2 has described “Kawasaki disease shock syndrome” (KDSS) as an unrecognized complication of KD. Interestingly, 13/187 (7%) patients with diagnosis of KD developed hypotension (as defined by pediatric advanced life support guidelines) or had clinical signs of poor perfusion that required fluid resuscitation and inotropic support. Compared with KD patients without shock, patients with KDSS were more often female and had larger proportions of bands, higher CRP concentrations and lower hemoglobin concentrations and platelet counts. Evidence of consumptive coagulopathy was also common in the KDSS group. Additional findings in KDSS group are impaired left ventricular systolic function, mitral regurgitation, coronary abnormalities and IVIG resistance.
Our patient had significantly elevated CRP, thrombocytopenia, prolonged coagulogram, elevated D-dimer with supporting evidence of left ventricular systolic dysfunction, mitral regurgitation, coronary abnormalities. More important than the initial clinical and laboratory findings, our patient showed a resistance to IVIG treatment as has been reported in the Kanegaye study.
KDSS is a newly recognized complication of KD. The causes and factors contributing to the development of KDSS are still undiscovered. Some laboratory tests suggested greater underlying inflammation and more intense vasculitis in KDSS. To the best of the author’s knowledge, there has to date been no report of KDSS in Thailand. This first case report emphasizes the presence of this new complication, and thus the need for pediatricians, pediatric cardiologists and pediatric intensivists to be aware of, and recognize the highly varied clinical manifestations of the most common acquired heart disease in children, namely Kawasaki disease.