Desmoid tumors (extra-abdominal), also known as aggressive fibromatosis, are benign locally aggressive slow-growing lesions, which arise from deep musculo-aponeurotic tissue. These rare tumors account for 0.03% of all tumors and 3% of all soft-tissue lesions1 and they are broadly divided into Intra- and extra-abdominal lesions. Their clinical presentation is quite variable and depends on their location and their potential to expand, compress and invade surrounding neuro-vascular structures. While some may present as a painless swelling, others may be also associated with pain and contractures.2 Surgery with wide-margin resection has been the mainstay of treatment for symptomatic lesions.2-6 However this approach has been challenged because of the associated risk of surgical injury to adjacent neuro-vascular structures and the relatively high recurrence rate (23-77%) of these tumors.3 The latest consensus guidelines from the National Comprehensive Cancer Network (NCCN) recommends observation as a primary treatment option for surgically unresectable tumors or resectable tumors that are not symptomatic, life threatening, or causing significant impairment.7 A recent review8 suggested other conservative, non-surgical treatment options, including radiation therapy, systemic NSAIDs, anti-estrogens, Tyrosine-kinase inhibitors, Interferon and cytotoxic chemotherapy. Given the rarity of this tumor, there were no randomized and prospective trials for different treatment available making it difficult to find the best way of treatment.4
We report a case of symptomatic (extra-abdominal) desmoid tumor which responded favorably to another conservative management of intra-lesional injections of Cox-2 inhibitors.
A 38-year-old female, married with one son, presented to the Internal Medicine out-patient clinic in July 2011, complaining of a painful mass, which had appeared about 2 months before, on her left forearm, close to the elbow joint. She has been known to suffer for the last 20 years from SLE and had been on long-term treatment of SLE, hypertension, osteoporosis, dyslipidemia, and chronic disease anemia with: 25 milligrams of prednisolone, 100 milligrams of azathioprine, 5 milligrams of amlodipine, vitamin-D and calcium supplement and a weekly dose of 70 mg of bisphosphonate. Physical examination by the attending rheumatologist revealed a 3x3 cm, round and firm mass in the left cubital fossa, which was close to but did not involve the joint. She was sent for further work-up and was advised to use diclofenac and cold compressions.
An ultrasound exam (December 2011) revealed a well-defined heterogeneous echogenic mass, located in the inter-muscular space of the flexor compartment of the left forearm, which measured 2.7x1.5x4.5 cm. It was noted to be located near the brachial vessels, without evidence of vascular encasement. When her symptoms worsened and also paraesthesias appeared, she was referred to the orthopedic out-patient clinic (March 2012).
An MRI examination performed immediately thereafter, revealed a 2.1x2.6x4.6 cm. fibrous tumor, probably a fibromatosis, surrounding biceps tendon insertion at the radial tuberosity. The mass touches the median nerve, located close to the radial nerve, but with no definitive evidence of neurovascular encasement. Two weeks later an incisional biopsy was performed under local anaesthesia. An experienced pathologist reported a spindle cell lesion with pale nuclei which have low cellularity and abundant collagen. There was no definite malignancy seen in the specimen which suggested a desmoid tumor (Figure. 1). The diagnosis of desmoid tumor was made from MRI imaging and pathological finding of the biopsy.
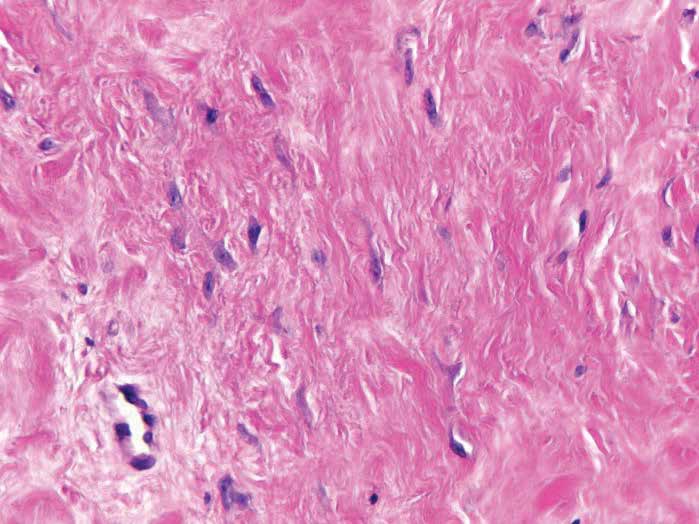
Figure 1: High magnification of the tumor specimen reveals a spindle cell lesion with pale nuclei which have low cellularity and abundant collagen. There was no definite malignancy seen in the specimen which suggested a desmoid tumor.
In view of the histologic diagnosis and the proximity to major nerve and vascular trunks of the forearm, it was decided to attempt conservative treatment, rather than surgical extirpation of the tumor. Since some reports8,10,11 suggested a positive response of desmoid tumors to oral Cox-2 inhibitors and the patient was already receiving a fair amount of oral drugs, we thought it justifiable to use intra-lesional injection of the drug. After appropriate informed consent was obtained and the protocol was approved by the institutional review board of our institution, we injected (May 2012) 2 ml of Parecoxib solution (40 mg) into the tumor on the patient’s forearm under ultrasound guidance and a second dose followed 2 months later (July 2012). On a follow-up visit (August 2012) the patient reported that the pain had significantly subsided and the physical exam suggested some reduction in tumor size. A third dose was injected (October 2012), after which a follow-up MRI showed no significant changes in either size or local invasion. On further follow-up visits (November 2012, February 2013, May 2013) the patient reported that both her pain and paraesthesias had disappeared completely and the tumor seemed not to have increased in size. In view of this apparent positive response, the patient received 3 more intra-lesional injections of the same doses of the drug, with 2 month intervals between the injections (May 2013, July 2013, and September 2013). On follow-up visits (November 2013, February 2014) the patient remained symptom-free and the tumor was noted to decrease in size. A third MRI (February 2014) confirmed a slight reduction in tumor dimensions (2.0x2.3x4.1 cm) and a reduction in tumor volume from 13.81 ml to 8.67 ml (37.22%) see Figure 2. Lastly (December 2015) when she was contacted she confirmed to have remained symptom-free and her impression is that the tumor has remained the same size.
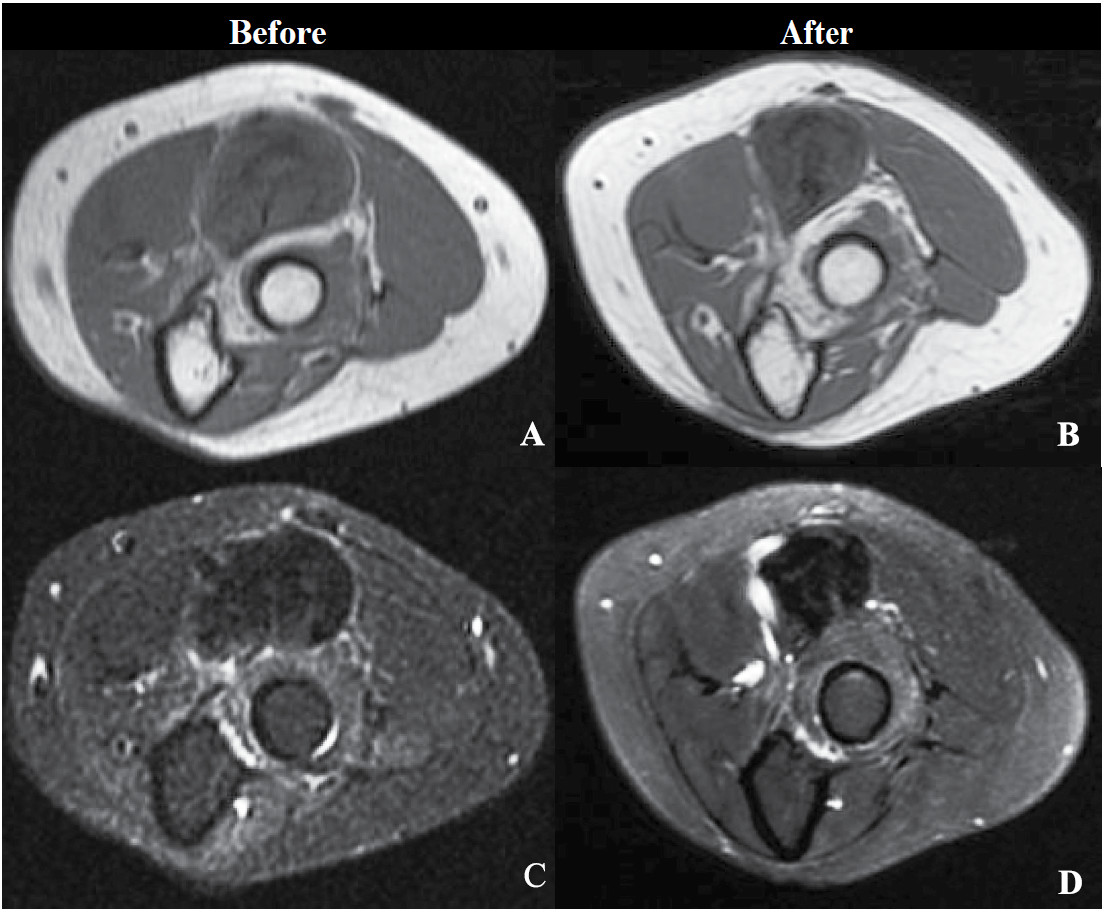
Figure 2: Axial view of the tumor in T1 and T2 (pulse sequences) from MRI study prior to and after 6 doses of treatment showing a decrease of tumor dimensions. A and C are images prior to the treatment. B and D are images after 6 doses of treatment.
This case report describes a symptomatic (extra- abdominal) desmoid tumor in the cubital fossa of the forearm of approximately 4 years duration, which responded favorably to intra-lesional injections of a Cox-2 inhibitor. Although we entertained surgical resection in our case as she showed increasing symptomatology, the tumor surrounded the biceps tendon and was closely adjacent to the median and radial nerves. Wide-margin resection in our case carried a significant risk of damage to these structures and we opted for conservative treatment.
Over the last 3 decades systemic NSAIDs have emerged as a conservative treatment options for extra- abdominal desmoids tumors. Typically, desmoid tumor cells show accumulation of beta-catenin, which appears to play a major role in their pathogenesis, and over-expres- sion of cyclooxygenase, specifically COX-2. NSAIDs are believed to interfere with both beta-catenin function,12 as well as cyclooxygenase activity.11 In the mouse model COX-2 blockade resulted in reduction of desmoid tumor size13 and there is anecdotal report of beneficial effects of NSAIDs in humans.12 Similarly, there is case series (22 patients with desmoid tumors) demonstrated complete/ partial response or stabilization of tumor growth14 in response to systemic NSAIDs, alone or in combination with other agents.11 Our patient was already on many medications and we were concerned with the risk of side effects and or drug interactions. The option of intra-lesional injection of a drug for desmoid tumor treatment has been previously described with collagenase, as tumor cells usually contain large amounts of collagen.15,16 Compared with surgery, intra-lesional collagenase injections were associated with faster recovery time, lower cost and less physician required follow-up time.
Desmoid tumors’ behavior, somehow, is unpredictable. In a series of patients with desmoids and familial adenomatous polyposis noted that 10% of desmoid tumors will resolve spontaneously, 30% will undergo cycles of progression and resolution, 50% will remain stable after diagnosis and 10% will progress rapidly.17 Desmoid tumors, in a case series with 106 cases, also have been reported to stabilize after evolving actively over a median period of three years.18 Fiore also reported in his study of 142 cases that 50% of his patients have a stable disease after 5 years of wait and see strategy, but for patients who progressed, the median time to prog ression (TTP) was 14 months.19 Chew suggested that the natural progression of desmoids is erratic at best with some studies demonstrating 89% of cases progressing within the first 2 years of referral, but not to greater than twice their size.20 Few cases also reported a spontaneous regres- sion.21,22 Our patient reported a progression of the tumor size and her symptoms around one year before the treatment began. MRI study after three and six doses of COX-2 inhibitors injection showed tumor growth arrest and improvement which were about 17 and 29 months respec- tively from first becoming aware of the disease.
From suggestions of the tumors’ behavior from previous studies, our treatment can stop the tumor growth during its progression period. The treatment then reduces the tumor size in the time that many studies suggest the moment of progression or stable disease.
Although in our case we have witnessed a positive response to intra-lesional injections of a COX-2 inhibitor, one should be cautious before making any conclusions. The natural history of desmoid tumors is very unpredictable and spontaneous regressions have been reported as mentioned above.
We would like to report this case to inform that this rare tumor had shown improvement with our new method of treatment. Further research and clinical experience with intralesional injection of COX-2 inhibitors in extra- abdominal desmoids tumors may provide better evidence for this therapeutic option. We hope that our report could be useful in giving ideas in managing desmoid tumors. Hopefully, we may find another good choice of treatment for desmoid tumor patients in the future.
Desmoid tumors are rare and the true behaviour of the tumor is still unknown. The gold standard of the treat- ment is surgery. In some cases where surgical interven- tion is contraindicated, conservative treatment may have its role. NSAIDs is one of desmoid tumors’ conservative treatments. From our case report, this is the only single case presentation. It is not statistically applicable. This article is only a contributor for clinical trial for future collection of more data. Of course we do not have similar conditions such as keloid hypertronic scar or keloid in difficult area for surgery to apply this method. This method may arrest a progression of disease during its active period. Further study is required before approval for clinical application. It showed that desmoid tumors can respond to intra-lesional NSAIDs. This new method of therapeutic option had shown to arrest a progression of disease during its active period. All things considered, further study of this method is required.
We thank Prof. Dan J. Sherman, MD, for helping us in writing this manuscript.