Diabetic Mellitus (DM) is a lifelong chronic disease that has a major impact on health care costs. Taking care of diabetic patients relies heavily on adequate and accurate informatics. In order for care providers to view a patient history and to be able to project the trend of future treatments, the health information system must be concise and include a function for easy access to patient records to efficiently locate all the related data. At the Bangkok Medical Center (BMC), the existing Hospital Information System (HIS) is mainly used to manage administrative functions, such as making appointments, registering patients, order entry, results reporting, and billing. The traditional paper clinical record from providers are still used and scanned as an image into the HIS. We found that the HIS is too generalized and broad, and does not meet the specific needs for diabetes management. The display of information is sub-optimal, not only because it’s incomplete and often contains scanned images of illegibly written notes, but also because it presents a cluttered user interface (UI) that includes myriad windows with laboratory results, radiology reports and medication lists, making viewing of summarized data quite difficult.
Additionally, The American Diabetes Association’s (ADA) standards of medical care in Diabetes 20141 suggested that optimal diabetes management requires an organized, systematic approach with the involvement of a coordinated team of dedicated health care professionals working in an environment where patient-centered high-quality care is a priority. Furthermore, the provision of care coordination as recommended by ADA and Joint Commission International (JCI), can only be achieved by leveraging information system technology.2,3 We looked for a tool to compliment and extend our HIS to deliver diabetes-specific care.
We ultimately decided to innovate and develop a new diseasespecific electronic medical record (EMR) system to support the management of diabetes patients. Hopefully, this project will encourage other specialists to use this disease-specific EMR instead of traditional clinical records stored on paper.
In summary, the expected goals of the project are as follows:
- To create a system of choice for endocrinologists and other physicians to use interactively, allowing them to focus on the medical history rather than resorting to paper for clinical notes and orders.
- To improve both function and workflow for effective manage- ment and care of DM Type 2 patients.
- To achieve and sustain the standard medical care recommended by JCI and ADA.
- To ensure effective communication between a multidisciplinary care team.
- To reduce the use of paper and enable a fully digital clinical record of care.
- To act as the source of reliable clinical data for data analysis for educational and medical research purposes.
- To be the first pilot project at BMC to study the utilization of disease-specific EMR.
The system called DM EMR was developed through a collaboration of in-house IT technicians who worked closely with endocrinologists and DM nurse specialists. The DM EMR was implemented in the Diabetes Center in 2011. The Diabetes Center latterly received a certification from JCI CCPC for DM Type 2 care management in the same year.
DM EMR project was proposed to the executive team and finally received approval to proceed in planned phases:
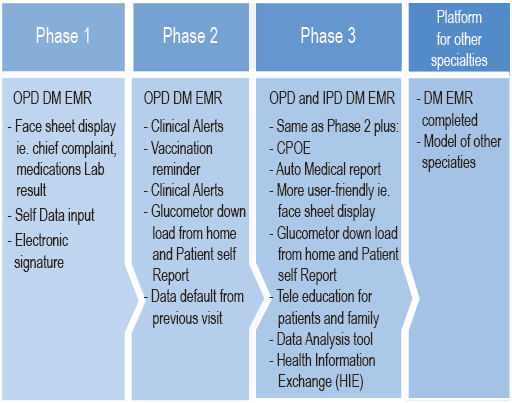
Figure 1: DM EMR Project Plan
In order to serve as an IT tool in facilitating best clinical practice, the software development teams needed to track the office workflow and support the DM Type 2 management care recommendations. The starting point in designing an efficient EMR work process was to assess the clinical needs. As shown in Figure 2 and 3, IT technicians and clinical team members worked together to determine the user requirement. After in depth discussions, the project team decided to leave orders and prescribing functions in the HIS and to leverage these capabilities in developing the DM EMR as an additional independent module.
Initially the DM EMR will be used only for patients aged 15 to 80 years old with DM type 2 diagnosed and HbA1C ≥ 7. A requirement of the clinical team was to have the DM EMR automatically look for these required criteria in the DM type 2 pathways. Once the patient is selected to participate in the pathway, the patient data is transferred and integrated with the information from the HIS, including ICD 10, prescriptions and all lab values. The face sheet of the DM EMR includes: Chief Complaint, Medication List, Diagnosis List, Laboratory Results List, Vital Signs List, Cumulative Creatinine, Next Appointment List, and all the pathways the patient has been on. In addition to retrieving the HIS, DM EMR allows providers to manually enter medication lists as well as lab results from other hospitals.
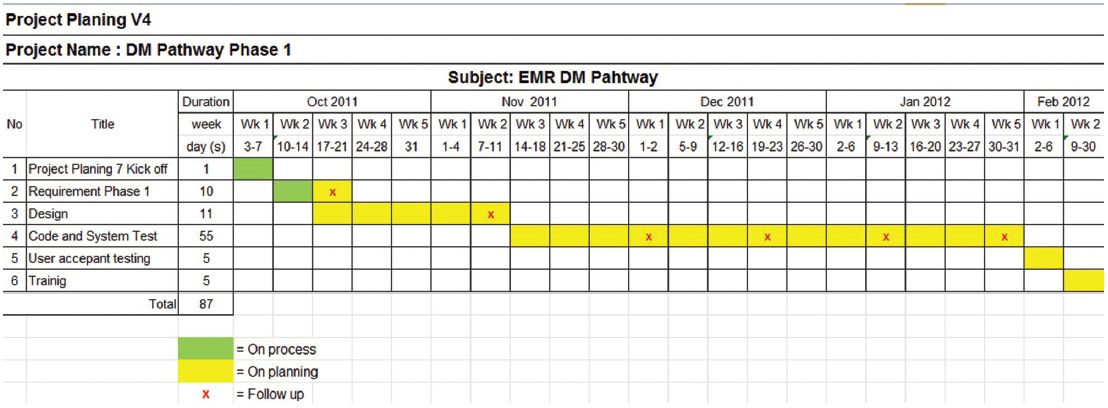
Figure 2: DM EMR Project Schedule
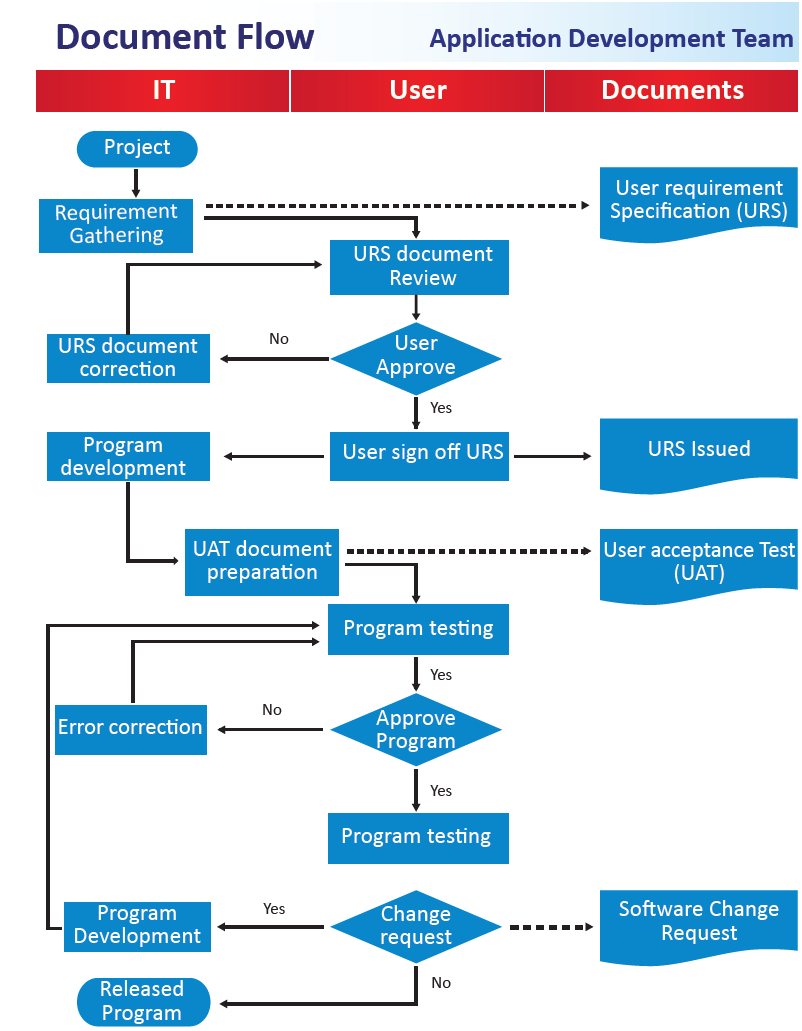
Figure 3: DM EMR designing process
One of the useful functions of EMR is automated alerts to improve the quality, safety, and consistency of the care process. The clinical team demanded automatic “Clinical alerts”, recommended by American Diabetes Association (ADA) and JCI standard care, as follows:
Clinical Alert Remark
- HbA1C Examination needed every 6 months
- LDL Cholesterol (direct) Examination needed every 1 year
- Microalbumin (Urine) Examination needed every 1 year
- Eye Examination needed every 1 year
- Influenza Vaccination every 1 year
- Foot examination needed every 1 year Low risk : every 1 year
Moderate risk: every 4-6 months
High risk: every 1-4 weeks
Reminders are required to assist the physicians in enabling evidence-based therapeutic decision-makingas well as increasing pathway compliance.
Condition Warning
- HbA1C ≥ 9% - Intensive therapy; 2 or more groups
of medication required
- LDL ≥ 100 mg/dl - Statin required
- Microalbumin urine - Angiotensin-converting-enzyme
> 30 mg/gm/ inhibitor(ACEI) and/or Angiotensin II
receptor blockers(ARB) required
(Twice repeatedly)
Design performance requirement
Acceptance Criteria:
- Able to search for all patients in HIS with all complete data
- Able to transport the complete data as scheduled from HIS
- Able to alert all clinical teams for necessary diagnostic and treatment interventions
- Able to record all data as identical as First Visit Form and Follow-Up Form
Performance Requirements:
- DM EMR transporting the information from HIS every 5 minutes
- Unlimited access for users
- Timely response
- Easy to use
- If HIS system is down, the DM EMR system can operate independently of the HIS.
Document Scanning
Originally, the medical record was scanned and saved as an image for viewing. For the DM EMR, after physicians complete the clinical record form, it is sent to the Doc Scan system and saved in the HIS as show in Figure 4
However, physicians cannot submit the clinical record to Doc Scan unless an ICD 10, diagnosis and all requirement sections and clinical alerts are completed. Unlike the existing HIS, the DM EMR record can be retrieved and edited later, with the time stamp and the signature of the person who modifies the record added to the saved record.
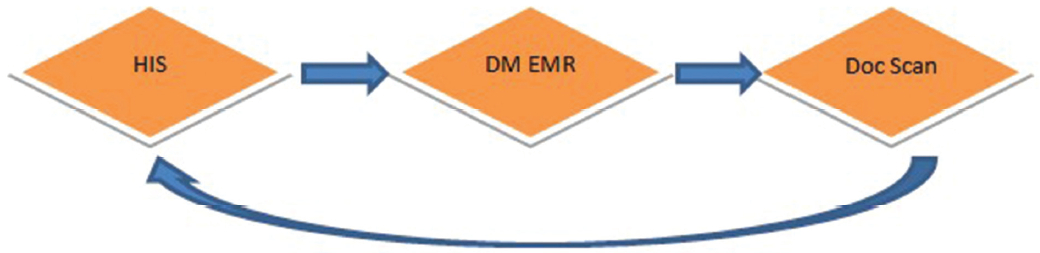
Figure 4: Documents flow
1. The benefits of the DM EMR
- Provides complete and comprehensive information: The patient face sheet gathers all relevant information in one place, i.e. lab results, which makes it easier to consider all aspects of a patient’s condition and this results in an improved quality of care. Also an ICD 10 coded diagnosis is included for comorbid diseases.
- DM EMR enhanced documentation: After implemen- tation, compared with the original paper clinical record and the statistics in completeness of clinical documents for DM Type 2 pathway first increased and eventually reached 100%. We have no more problems with being unable to read a physician’s handwriting in the out-patient department (OPD). A comparison example of the clinical records is shown in Figure 5 and 6.
- Improving patient education and satisfaction: Most patients reacted positively to the DM EMR; it enables access to graphing and trending features. The patients were satisfied with a more responsive exchange of information with their physicians.
2. DM EMR Glitches
1. Technical problem
- The physicians have to work on two screens, requiring two sign-ons and additional effort. - Data exchange problems: synchronization of data between two systems, the HIS and DM EMR is challenging and occasional glitches have resulted in laboratory missing values. Occasionally a laboratory value is missing in DM EMR.
2. IT technicians and Learning curve
- Over the period of the two years of the project, the high rate of IT staff turnover was a problem. It caused a lack of continuity in developing the software program and prolonged the development process. Hiring outsourced IT staff was a challenge.
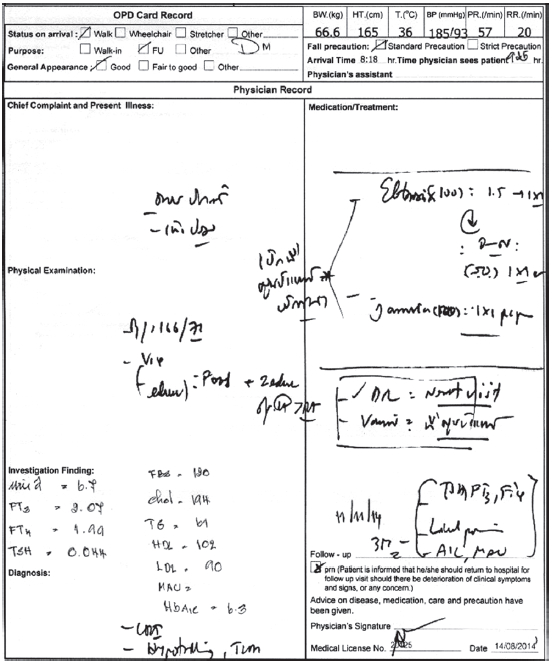
Figure 5: Original OPD Clinical Record
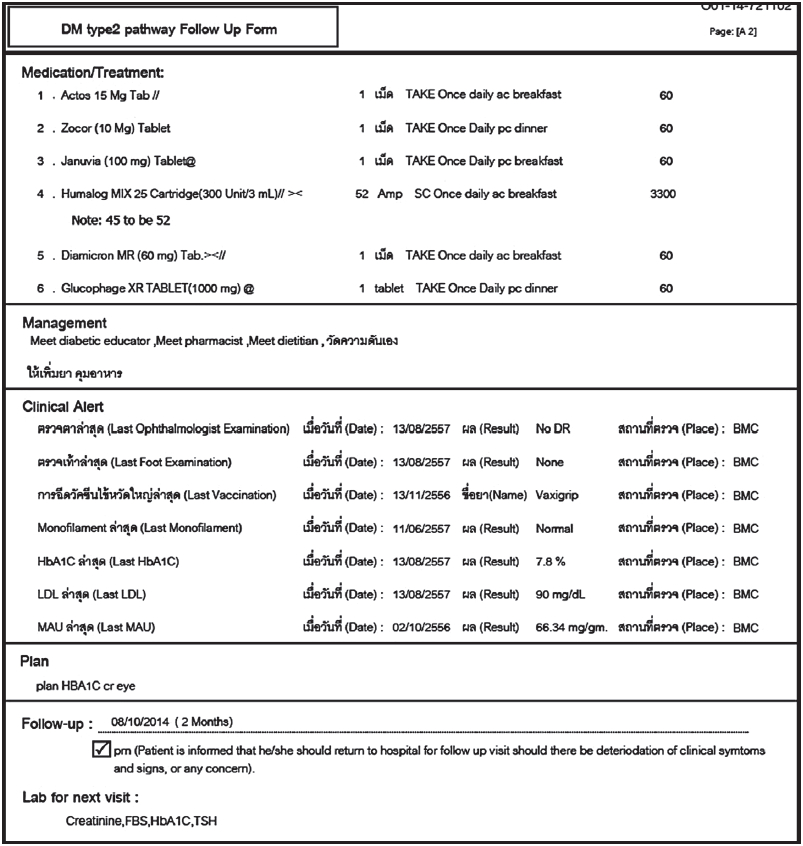
Figure 6: DM EMR OPD Clinical Record
3. Time consuming
- Entering structured data is more time-consuming than charting free-text on the paper. Moreover, it requires physicians to map concepts into the new clinical record templates. Eventually, efficiency improved, but the process still took longer than writing in the original clinical record paper. It is yet another task to encourage the physicians to use EMR in their practice. The main strategy for over- coming this problem involves separating the EMR use from time spent communicating with patients. Modifying the software for easy data access and viewing, fewer clicks, and providing more check boxes would help reduce the time spent. Computer mastery and enhanced physicians’ communication skills also helps.4
Being the first hospital to use an EMR specifically for diabetes management in Thailand, and after more than two years of implementation, we achieved most of our goals. Besides, we have learned several lessons from the DM EMR development and implementation. The difficulties found after implementing the DM EMR were solved eventually by the dedicated working team. The Plan Do Check Act model has been used in helping reduce working times, and the program has been modified many times to resolve technical problems and respond to user requirements.
Finally the system is a success as a disease registry, and in providing data for research and quality improvement in the future. DM EMR is diabetes’s oriented standard treatment; the physician can effectively deliver comprehensive and essential care to the patient. Recently, the JCI came for the re-certification of our hospital and they had very positive comments regarding our EMR project especially with regards to the safety part of patient care, and improvement in the legibility of records.
After we learned some hard lessons, our plans for a new DM EMR is make it more user-friendly, customizable, and for it to display information on one page to facilitate effective navigation, using fewer clicks. The provision of physician record templates would also help improving effectiveness.3 A good sign is that most of our endocrinologists are now getting used to and are keen to use our DM EMR. We are now planning for phase 3, building IPD DM EMR as a tool for better diabetes care management in the Inpatient Department (IPD). This IPD EMR will extend the requirements of the OPD DM EMR, adding new features such as progress notes and Computerized Physician Order Entry (CPOE).
In the next phase of development, we would like more patient involvement, which we think will improve care and increase patient satisfaction6. Engaging our patients in the process is required to enable more interactive patient- centered care, allowing them for example to download their home monitoring glucose from home to the EMR for physician review. Other benefits include sharing tele-education with patients and their families. We also want to improve nursing satisfaction with the EMR as a tool for patient education. Beyond that, our patients can get their own summary reports every visit with their medications, blood sugars, weight loss and HbA1c’s goals.
The leadership role as a project manager is to promote and to encourage the use of the EMR as a standard tool in hospital for better care for our patients. First, to create sufficient urgency, we are due for a recertifying survey of CCPC from the JCI at the end of this year. Also, we are seeking and applying for a new extension certification of the Inpatient Diabetes care for the next JCI’s survey. This is an opportunity to lead and orchestrate the development process of both function and workflow for the EMR on the IPD service. To this extent, a clear vision will be passed to all working team members emphasizing that the EMR helps to prevent illegible handwriting of notes and orders. Also, in order to leverage the lessons learned from the current DM EMR to the 3rd phrase of the EMR, the IPD EMR will be re-engineered. A more powerful coalition will be extended to others such as IPD head nurses, critical care physicians and surgeons to demonstrate the good benefits of the EMR.
In the near future, a health information exchange project called B-Exchange will transfer clinical information between hospitals in Bangkok Dusit Medical Services Network. We hope that DM EMR can be implemented in other hospitals in the network, providing continuity of care and via B-Exchange. We are not declaring victory too soon, but we are ready for the challenges to come.
I would like to give a special thanks to Dr. Mike McCoy, BMC chief medical information officer, for being a supportive consultant for the DM EMR project and for his thoughtful reading of this article and critical comments. Thanks to IT Information Management Committee (IM) for supporting the project. Lastly, I also would like to thank the IT technical team of BMC and all the staff at the Diabetes, Thyroid and Endocrine Center for their devoted work.