The Hypertension Clinic is a part of the Internal Medicine Outpatient department (OPD) at the Bangkok Hospital Medical Center. Hypertension patients account for 15% of all Internal Medicine OPD visits. It is now widely accepted that hypertension management is also a concern to other cardiovascular risk factors. Besides the process of measuring blood pressure and prescribing medications, better management can help prevent more cardiovascular vascular complications.1-4
The primary goals of the Hypertension Registry are:
1)to create data as a tool for quality control (QC) to help improve the quality of future services and planning
2)to create awareness of other associated medical conditions that are risk factors beyond blood pressure levels in both patients and service providers to increase public awareness
3)to make use of electronic medical records (EMR) to benefit both patients and service providers
4)to improve service efficiency and continuous education of clinical staff and physicians by periodically creating feedback data reports
During the first seven months of the Hypertension Registry, 647 patients with hypertension enrolled in the programme. The objective of the study is to highlight the main data of patients who registered in the programme compared to a group enrolled in one physician’s hyperten- sion registry.
The Hypertension Registry was established in June 2012. Patients’ demographic and clinical information of is retrieved from two data sources: the electronic medical records (EMR) and collating information by hand. The process to create a registry entry is as follows:
The staff
1)Coordinator Nurses (who also play a role as educators) open each case entry by inputting the initial information (a new case entry is partly picked up from ICD-10 diagnosis in the department and some cases are opened by physicians themselves or through physician assistants who inform the nurse coordinators). An icon is created in the EMR for each case and flagged as a hypertension registry member case. A review and data input for antihypertensive medications prescribed is inputted, plus information is audited to check the entries are correct. A summary is generated periodically (every 3-6 months) with assistance from Information Technology staff to create reports for the Hypertension Clinic and as a feedback information mechanism for the physicians involved.
2)Physician Assistants coordinate physicians and coordinators.
3)Physicians who attend the patient and act as team consultants.
4)Information Technology (IT) staff help the team from an early stage in the process and create appropriate software for the electronic medical records, create additional input questionnaires for specific data, and create programmes for the data summary system.
The Process
1) The demographic information of each registrant is linked to the EMR once the patient is entered into the hypertension registry and a HT icon is created on each individual EMR to flag the patient as a member of the registry. The patient’s past history and any associated illnesses are reviewed from the EMR and the patient record files and also available including interviewing the patient during an education session conducted by a nurse coordinator.
2) Laboratory investigations identify any organ damage i.e. EKG, echocardiography, chest x-ray, urine for microalbumin (MAU) and Ankle Brachial Index (ABI) by using a vascular screening machine “VaSera” (this machine measures both ABI x CAVI) which also measures a Cardio-Ankle Vascular Index (CAVI).5-8 The results of each investigation are retrieved from the EMR and input into the registry by directly linking the information to the date the investigations were performed. At present, only the linked information can be accessed in bulk but the results from various measurements still need to be input manually.
3) Medication use was reviewed from the EMR and the medical records file. Antihypertensive medication was classified into 9 groups; 1) Diuretics, 2) Dihydropyridine calcium channel blockers (DHP CCB), 3) Non dihydropyridine (non DHP CCB),
4) Angiotensin-converting enzyme inhibitors (ACEI),
5) Angiotensin II receptor blockers (ARB),
6) Direct renin inhibitors (DRI), 7) Alpha blockers,
8) Beta blockers, and 9) Others. The combination antihypertensive tablet was counted as 2 or 3 isolated medications that are the components of the pill prescribed at the same time. The medication is entered by trade name and is automatically allocated to the group they belong to in accordance with the preset lists of the antihypertensive medication database. 4) At each visit the registrant’s height (cm), and body weight (kg) is reviewed and this data is added to the individual’s database by the physician assistants. Blood pressure values (both systolic and diastolic) are collected after visits to the physician. The data inputs are corrected and audited by nurse coordinators and the team every 2-4 weeks. 5) The summary is preset for future periodic reports. It was set to be searchable by period of time from one to several months to years and searchable by service providers, and by name, by group or by individual physician.
A whole staff team meeting, including IT staff, reviews the process and reports back every 2-3 months.
Since June 2012, when the Hypertension Registry was created, the number of registrants has gradually increased through a better understanding of the team members (Figure 1). A total of 647 cases were registered during the first 7 months.
Sex
About 57% of cases were female. The outnumbering of men by women was also true for the total of hypertension cases at the Bangkok Hospital Medical Center as well as the cases of one physician (Figure 2).
Age
Most registrants (74.5%) were aged between 51 and 80 years old compared to patients who registered in one physician’s registry (Figure 3).
Body Mass Index
Of those, half of all patients had a BMI of more than 24.99 and were categorized as overweight (Figure 4).
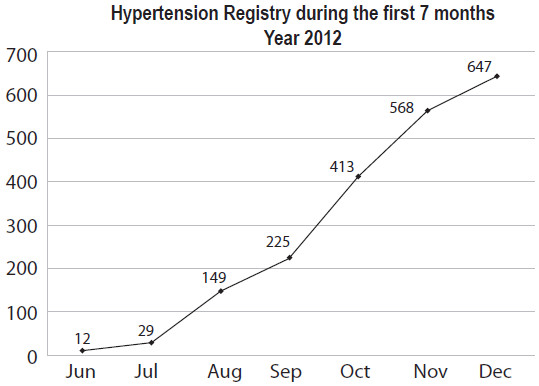
Figure 1: Demonstrates the progression of the number of enrolled cases in the Hypertension Registry during the fi rst 7 months
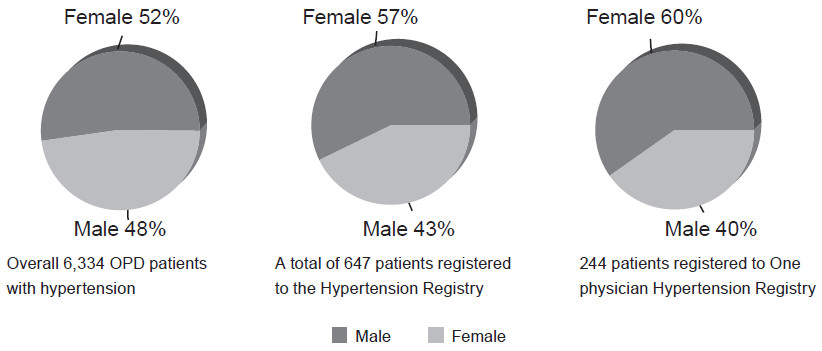
Figure 2: Sex distribution of 6,334 hypertension patients from the whole medical center (the left is compared with 647 cases from The Hypertension Registry (middle) and 244 cases from one physician hypertension registry (right) during the same period.
History of risk factors
According to an initial interview of 84 cases, 51.9% had dyslipidaemia and 34.8% had diabetes mellitus (DM). Heart disease was found in 4.4%, kidney disease in 3.7%, stroke in 3.2%, and 0.7% of cases interviewed had peripheral vascular disorder as in Figure 5.
Laboratory investigations: EKG was the most frequently ordered investigation (34.4%) followed by chest x-ray, ABI, and MAU in 27.9%, 19.5% and 18.1% respectively while ABI was the second most frequent investigation required in one physician’s registry group (Figure 6).
Antihypertensive medication: 3.9% of all registry cases did not need any antihypertensive agents to control blood pressure. Most cases (53.5%) took only one item of antihypertensive medication. Of the remaining 32%, 8.5%, and 2.2 % used 2, 3, and 4 antihypertensive medications respectively (Figure 7). ARB was the most common group prescribed for the treatment of hypertension (35.6%). The second most common drug was DHP CCB (32.7%) and if combined with non DHP CCB (2.9%) then the percentage of the use of CCB would be equal to the ARB group. Beta blockers were used in 14.5% of cases and were more common than Diuretics (9.9%), ACEI (3.0%), alpha blockers (1.0%) and DRI (0.3%). Among 647 cases from the Hypertension Registry, there were no patients who used any antihypertensive medication marked as ‘others’ (Figure 8).
Achievement of blood pressure goal: approximately 90% of registrants had well controlled blood pressure by achieving SBP < 140 and DBP < 90 mmHg (Figure 9).
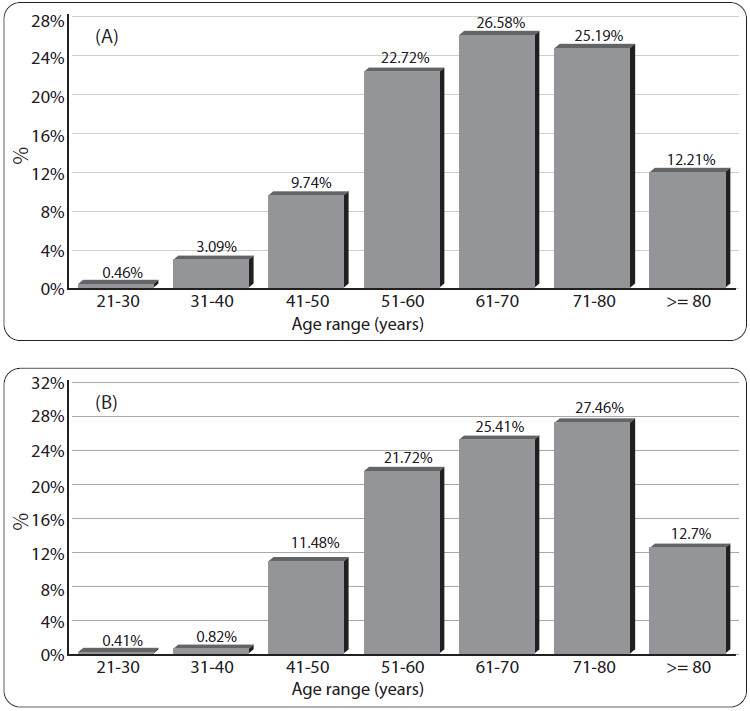
Figure 3: Age distribution amongst 647 patients who participated in the Hypertension Registry (A) compared to 244 patients from one physician’s registry (B).
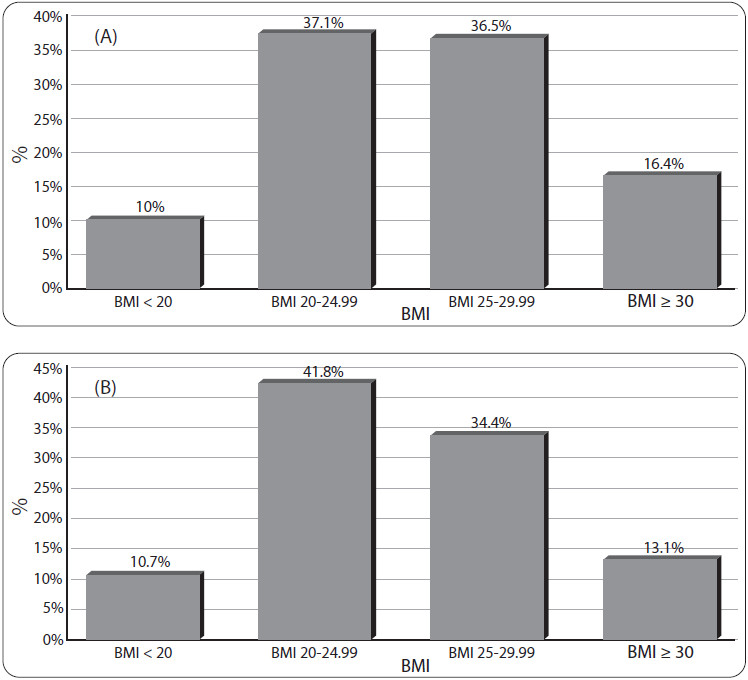
Figure 4: The Body Mass Index (BMI) distribution of 647 registrants who participated in the Hypertension Registry (A) compared to 244 cases from one physician’s registry (B).
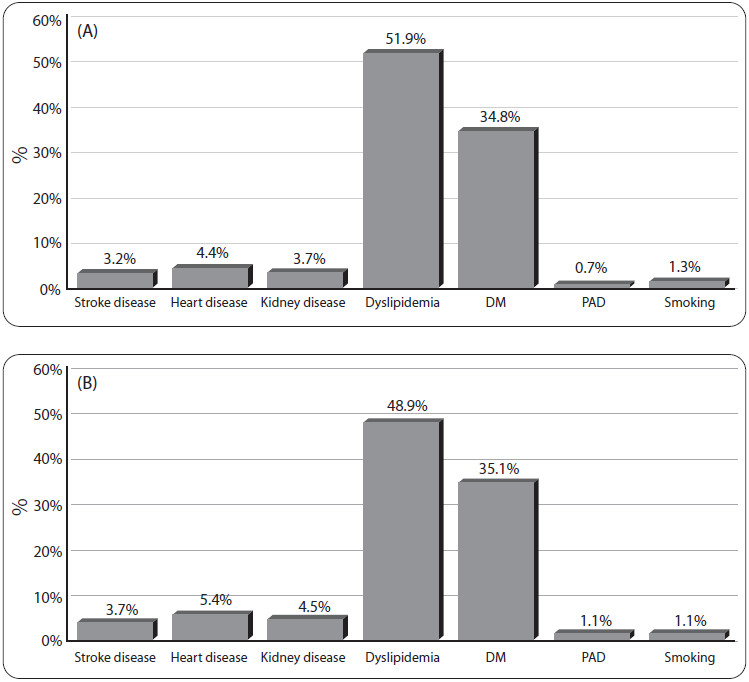
Figure 5: Associated risk conditions from the history of 84 patients from the Hypertension Registry interviewed (A) compared to 44 patients from one physician’s registry (B).
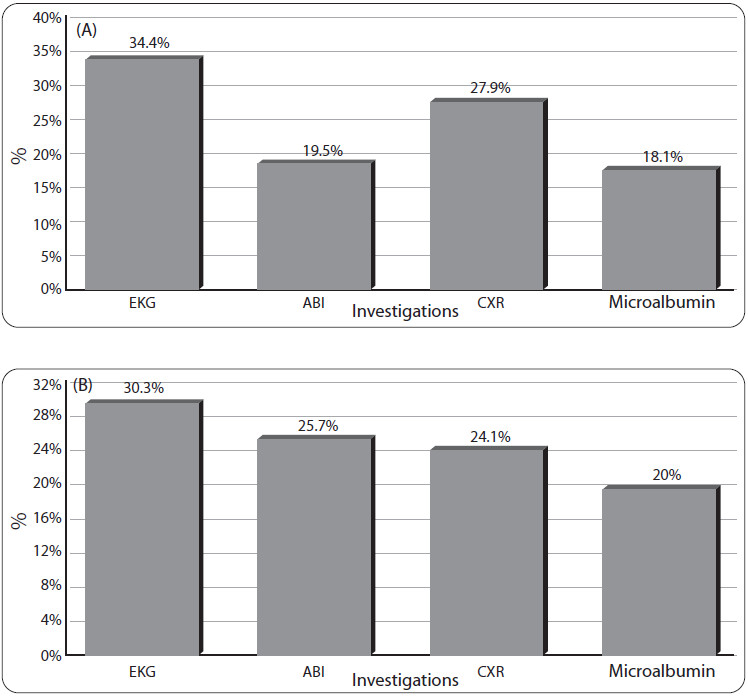
Figure 6: Percentage of investigations done in 647 cases from the Hypertension Registry (A) compared to 244 cases from one physician’s registry (B).
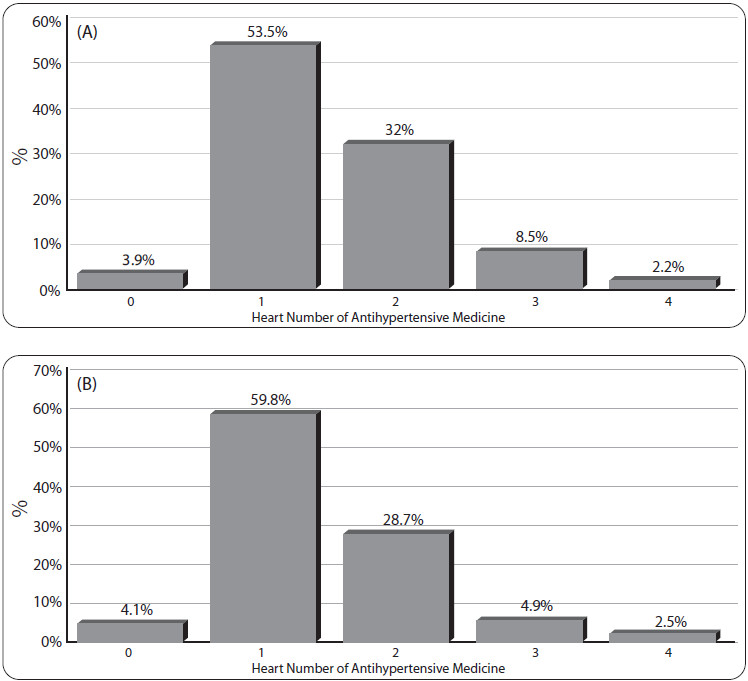
Figure 7: Distribution of registrants using 0 to 4 items of antihypertensive medications amongst 647 cases from the Hypertension Registry (A) and 244 cases from one physician’s registry (B).
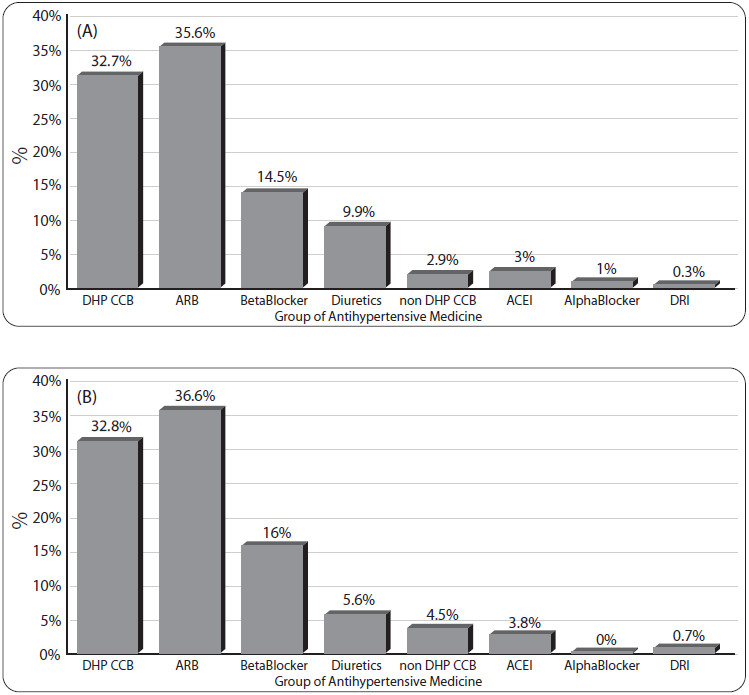
Figure 8: Group of antihypertensive medications amongst 647 cases from the Hypertension Registry (A) compared to 244 cases from one physician’s registry (B).
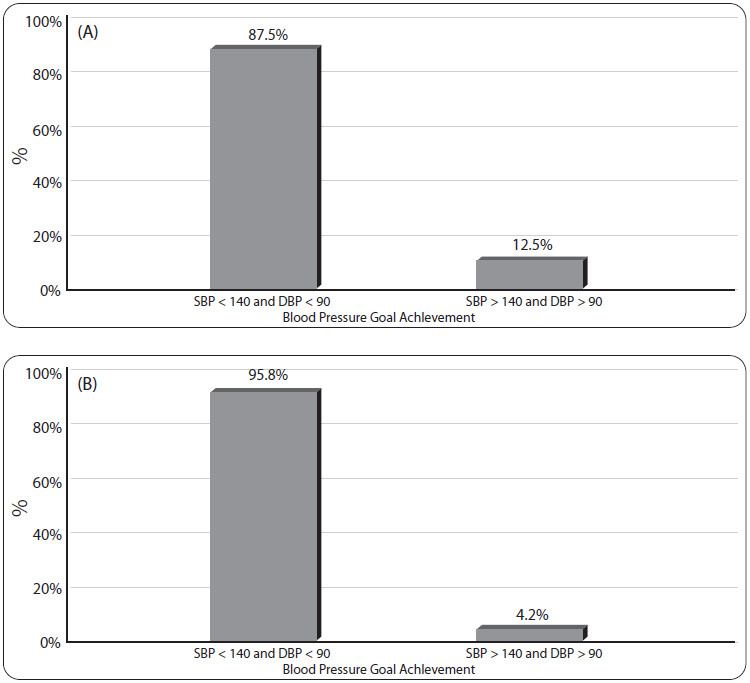
Figure 9: Percentage of cases achieving goal of treatment, SBP < 140 and DBP < 90 in 337 cases from the Hypertension Registry (A) and 120 cases from one physician’s registry (B).
During the initial 7 months of the Hypertension Registry, we can see many broad ideas that can be used to improve hypertension clinical services. About half of all cases were overweight (BMI > 24.99 kg/m2), and an EKG was taken assess any left ventricular hypertrophy evidence (only about a third of participants), urine micro- albumin was tested in less than a fifth of the cases despite much evidence to suggest that this simple test can warn us of the cardiovascular risk in hypertensive patients etc. All this information is critical for hospital staff to be able to plan for better services. Furthermore, the registry data can also be a good tool for patient education. It was surprising to discover that more than half of all patients only need one antihypertensive medication and about 90% of cases achieved the BP goal. These initial registry cases, however, will slowly and continuously accumulate, so it may be too soon to extrapolate, as this sample may not represent the reality. Time is needed for the registry system to develop and for staff to improve their skills and increase their experience. Also, larger numbers are required in the registry to help build a better picture of the current situation. This Hypertension Registry is a dynamic tool, able to accommodate frequent updates and to be adapted in the future if required. We hope to learn more from our information with a larger number of participants in the hypertension registry numbers, accompanied by a growth in global medical knowledge and guidelines.
The Hypertension Registry provides multiple benefits and valuable information. It is progressing well, and may yield firmer conclusions when the registry grows in numbers.
Acknowledgements
The authors and the Hypertensive Registry team would like to thank the CEO, the Bangkok Hospital Directors, the Medicine Patient Care Group Manager, and the President of the Medical Staff Organization of The Bangkok Hospital Medical Center for all their support towards this project’s development.