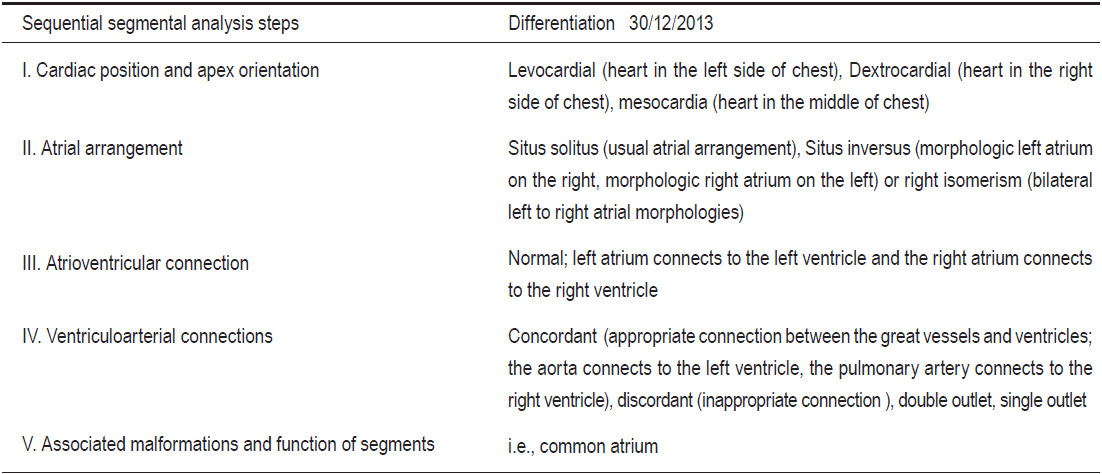
The snowman sign is a sign on a chest x-ray image that indicates a supra-cardiac type total anomalous pulmonary venous return (TAPVR).1 TAPVR is a serious congenital heart disease which occurs due to an abnormal development of the fetal heart. This leads to an inappropriate connection of all four pulmonary veins.1 TAPVR is a congenital left to right shunt disease where all four pulmonary veins are gathered into a vertical vein behind the left atrium. The vertical vein plays a role as a reservoir of oxygenated blood that drains into the right side system directly or via the left innominate vein. TAPVR causes neonatal death if there is no oxygenated blood shunting from the pulmonary venous circulation system to the systemic circulation system. Thus TAPVR is considered a critical congenital heart disease because an infant with TAPVR needs surgical correction early after birth to survive.2 The incidence of TAPVR accounts for 1-5% of all cardiovascular congenital heart disease.3,4 TAPVR is classified into four types according to the location (level) of the target organ of blood drainage from the vertical vein. The four types of TAPVR are: 1) supra-cardiac type, 2) cardiac type, 3) infra-cardiac type and 4) mixed type.1
The target organ of blood drainage in the supra-cardiac type is the right superior vena cava (SVC) which is at the supra-cardiac level. The head of the snowman sign is composed of a dilated vertical vein on the left, a dilated right SVC on the right and, in addition, there is sometimes a left innominate vein on the top. The body of the snowman is the dilated right atrium.1 The target organs of pulmonary venous drainage of the other types of TAPVR are shown in Table 1. The essential factor in keeping TAPVR patients alive is a right to left shunt pathway to facilitate oxygenated blood flow through systemic circulation. The most common right to left shunt pathway in TAPVR is a patent foramen ovale (PFO) and an atrial septal defect (ASD) and the least common is a patent ductus arteriosus (PDA).4 The specific treatment for TVPVR is the reconnection of all four pulmonary veins to the left atrium and the closing of cardiovascular defects. However, as a TAPVR infant grows up, the reconnection sites of pulmonary veins to the left atrium may be in stenosis which generally accounts for 40% of cases; therefore, a stent placement may be needed to permanently re-dilate the narrow venous port.5
A 15-month-old boy with TAPVR, heterotaxy syndrome and with status post bilateral Blalock Taussig (BT) shunts implantation in 2009 (with a status post stenting for PDA correction in the neonatal period) was admitted for a Fontan operation. During the admission process, the patient still had cyanosis with no worsening progression. A Pre-Fontan operation evaluation was ordered by the pediatrician.
Table 1: Type of total anomalous pulmonary venous return (TAPVR).
A twelve leads electrocardiogram (ECG) and an echocardiography was performed. The twelve leads ECG showed tachycardia (heart rate of 114 beats per minute), regular rhythm, complete right bundle branch block and large P wave amplitude which indicated an enlargement of the right atrium. The echocardiography examination revealed right isomerism heterotaxy syndrome and TAPVR supra-cardiac type, and a well patency of the right BT shunt (shunt connection between the right pulmonary artery and the right innominate artery) and a left BT shunt (shunt connection between the left pulmonary artery and the left subclavian artery) with preserved left ventricular function. The abnormal obstruction of the venous vessel was not shown on the echocardiogram. The echocardiographic result did not explain the cause of dyspnea. Thus the patient was sent to undergo a magnetic resonance imaging (MRI) study with and without a gadolinium-contrast injection to confirm the diagnosis. The gradient echo CINE MRI images demonstrated the following:
I.mesocardia
II.common atrium with bilateral right atrial morphology (right isomerism), the liver was in the middle
III.common right morphologic atrium connected to the common right morphologic ventricle, common atrio-ventricular valve
IV.double outlet connection of the aorta and pulmonary artery with the single ventricle, the right SVC and left sided IVC drained into the common atrium. All four pulmonary veins are confluence into the vertical vein and are connected to the left innominate vein on the left side, the left innominate vein is the connection vessel of the right SVC and the vertical vein
V.well patency of both Blalock Taussig shunts as reported in the echocardiography result (using the gradient echo CINE MRI and MR angiography with gadolinium contrast injection technique).
The stenosis of the left vertical vein at the emptying port to the left innominate vein, however, caused a high jet flow into the left innominate vein. This stenotic lesion was also seen on the coronal view of the gradient echo CINE MRI images and of the MR angiogram with gadolinium- contrast injection. This abnormal finding was not shown in the echocardiogram. This was an inconclusive result therefore a right heart catheterization was proposed and performed to obtain the final conclusion. The angiogram of the right heart catheterization study showed the stenosis at the junction area of the vertical vein to the left innomi- nate vein and a well patency of both BT shunts. The results of the right heart catheterization were compatible with the MRI result. Finally the patient was discharged and instructed to continue their current treatment. The patient will undergo a Fontan operation as planned.
Theory discussion
The case presented in this article is a supra-cardiac type total anomalous pulmonary venous return (TAPVR) with a right isomerism heterotaxy. The TAPVR case in this article is specified as a supra-cardiac type because the target organ of the pulmonary venous drainage, the right SVC, is found at the supra-cardiac level. TAPVR is a left (pulmonary veins-vertical vein) to right (SVC) shunt congenital heart disease. No pure oxygenated blood was emptying directly into the left atrium. The existing common atrium and common ventricle, including the connection between the vertical veins to the left innominate vein, were vital to the survival of this patient by increasing the flow of oxygenated blood flowing through the systemic circulation. The common atrium acts as a mixing tank of deoxygenated and oxygenated blood. The oxygenated blood travels from the vertical vein through the innominate vein and the right SVC to reach the common atrium. This baby has been admitted for a Fontan operation. The Fontan procedure is a palliative surgical procedure designed to divert the venous blood from the right atrium to the pulmonary artery bypassing the morphologic right ventricle. It has been used for infants with a single ventricle. It helps the single ventricle to work less hard.6 During the admission period while this patient was waiting for the Fontan operation; the patient received a bilateral Blalock Taussig (BT) shunts implantation. In theory, the Blalock Taussig shunt is a surgical connection shunt between the systemic artery and pulmonary artery and is used with the objective to increase pulmonary blood flow. It is an interim palliative treatment when waiting for specific surgical treatment in the future.7 The BT shunts of this patient are the connection between the right pulmonary artery and the right brachiocephalic artery on the right side and between the left pulmonary artery and the left subclavian artery on the left. A single ventricle with a double outlet caused an insufficiency of blood volume supply to the pulmonary system. The MRI study and a right heart catheterization revealed the stenosis of the vertical vein to the innominate vein. The obstruction of the pulmonary venous drainage can occur in any type of TAPVR. It is uncommon in type I but it is the most common obstruction in infra-cardiac type with an incidence of about 78%. In infants with TAPVR, cyanosis and congestive heart failure typically develop in the early neonatal period. Around 30% of the patients with TAPVR have other associated cardiac lesions such as heterotaxy syndrome with asplenia1 as did this patient.
Heterotaxy or isomerism or situs ambiguous are the arrangement disorder of the organs in the chest and abdominal cavities in an unformed fashion. Hetero-means different and -taxy means arrangement. The mal-formation and mal-position of the organs in heterotaxy are more complex than in situs inversus. In theory, the clinical pathologies of the heterotaxy are a discordance of the cardiac apex from the liver and stomach and include cardiac chamber malformations, with a common atrium, single ventricle, and transposition of the great vessels. A total anomalous pulmonary venous return occurs in the majority of cases, with asplenia or polysplenia. Situs inversus is defined as the mal-position of the organs in the chest and abdominal cavities as a mirror image with no presence of body organ malformation. For the heterotaxy, the discordant character of the thoracic and the abdominal organs lie between the situs solitus and situs inversus.8 The heterotaxy is also called situsinversus ambiguous. Atrial isomerism as mentioned in echocardiography and MRI results can be left or right isomerisms. The left and right isomerism mean the morphology of the two atria are left and right morphologies respectively. In this case, the patient has a right isomerism with asplenia (lack of spleen). In general, asplenia syndrome is the same as right atrial isomerism or Ivemark syndrome.9 The hallmark of heterotaxy is bilateral isomerism, left or right.10
Imaging discussion
TAPVR/heterotaxy is a good complex case to show how to approach a complex congenital heart disease with imaging tools. A thorough knowledge of the disease core pathology and imaging techniques is important to diagnose congenital heart disease. Good imaging protocol planning comes from good clinical and technical knowledge of the operator. In this article, the key to diagnose TAPVR is:
a)to document that none of the pulmonary veins drain into the left atrium,
b)to localize the common venous reservoir (vertical vein) that is the confluence of all pulmonary veins, and the target organ of the vertical venous drainage
c)to define any associated condition.
TAPVR is a complex congenital heart disease. In addition, a congenital heart disease approach by using imaging tools should be done in a systematic fashion to prevent a misdiagnosis and to prevent overlooking any information. The sequential segmental analysis principle has been proposed as an approach to evaluate congenital heart disease.11 Synchronization of the sequential segmental analysis principle with our clinical and technical knowledge to diagnose congenital heart disease using imaging tools has been proposed as a good comprehensive method for congenital heart disease approach.7 The steps in this sequential segmental analysis include an analytic method to assess and to report the diagnosis of congenital heart disease in a sequential order as shown in Table 2 and the MRI report result (step I-V). A sequential segmental analysis method involves a differentiation of cardiac tissue morphology of all chambers and a characterization of the cardiac chambers and great vessels’ connection including any associated conditions. Hence, a good application of sequential segmental analysis principle on imaging to approach congenital heart disease needs a modality with a high resolution, a widening field of view and a no limit window scan. The MRI seems to be the ideal modality for the application of the sequential segmental analysis approach principle. According to the steps of sequential segmental analysis approach, the tissue morphology differentiation is the most important. Tissue morphology analysis is the first step of this analysis approach technique to identify the components of the heart and the information results are described in sequential steps as shown in Table 2.
Well tissue characterization and differentiation are the strengths of MRI. A gradient echo white blood, CINE pulse sequence is the major pulse sequence used to perform tissue morphology differentiation. Cardiac anatomy and physiology can be assessed simultaneously on a gradient echo CINE MRI. To diagnose isomerism in cases of heterotaxy syndrome, the information about the anatomical structure arrangement and orientation of thoracic and abdominal organs is needed. As in this case, the patient was diagnosed as a bilateral right atrial morphology isomerism with asplenia, related to bilateral morphologic right bronchi or bilateral tri-lobar lungs.9 Therefore, the
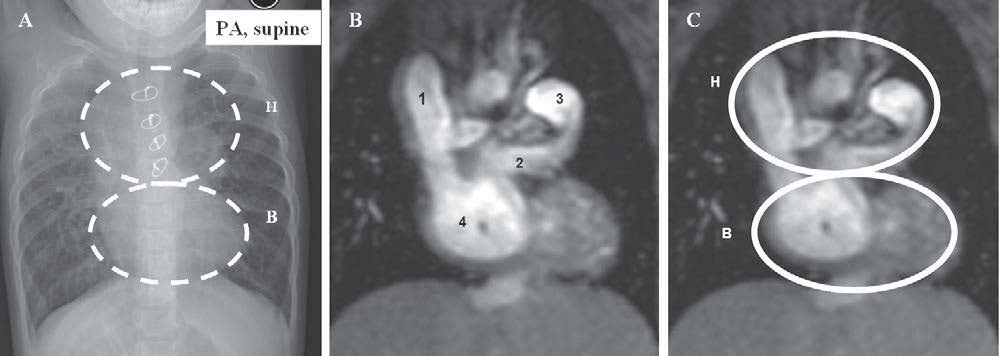
Figure 1: Chest x-ray image on PA-supine view and magnetic resonance imaging (MRI) using gradient echo CINE pulse sequence on coronal view show the Snowman sign of TAPVR supra-cardiac type. 1A: Snowman sign on chest x-ray image. 1B: Demonstration of the components of the snowman sign on a gradient echo CINE MRI image on the coronal view, 1 = Dilated right SVC, 2 = Dilated vertical vein, 3 = Dilated left SVC, 4 = Dilated right atrium. 1C: H = Head of snowman, B = Body of snowman.
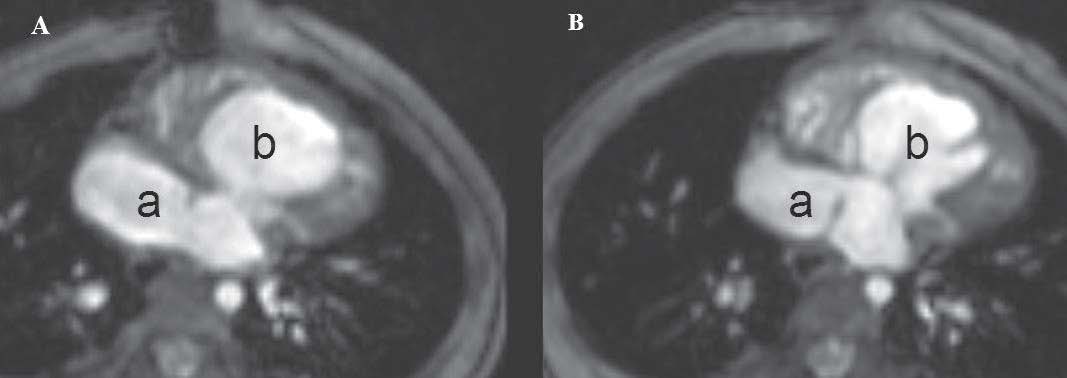
Figure 2: Sequential segmental demonstration approach steps I, II, III (see Table 1) are applied to MRI with a gradient echo CINE pulse sequence in an axial view. A and B show: mesocardia, common right atrium morphology (see atrial appendage character) (a) and common right morphology right ventricle (b), concordance of atrioventricular connection, right isomerism (bilateral atrial morphology).
imaging of bilateral morphologic right bronchial structure can be used to indicate right isomerism. The morphology of the bronchi can be seen simply by using a spin echo and gradient echo MRI pulse sequences on coronal and axial views. The hypo-signal of air in the trachea and bronchus are seen in both spin echo and gradient echo MRI images. This helps to strengthen the anatomical morphologic structure of these. Although sequential segmental analysis approach is used for cardiovascular anatomical analysis, it cannot be perfectly applied to every single imaging modality image in a one stop shop fashion. However, it can be used as a guide to approach congenital heart disease in a simple sequence of steps and can be applied completely in any combination on different modality images. Figures 1-5 show the inside of a snowman sign of TVPVR with right isomerism heterotaxy on MRI images and the synchronizing of the sequential segmental approach principle on MRI to assess a TAPVR /heterotaxy case.
Table 2: Type of TAPVR.
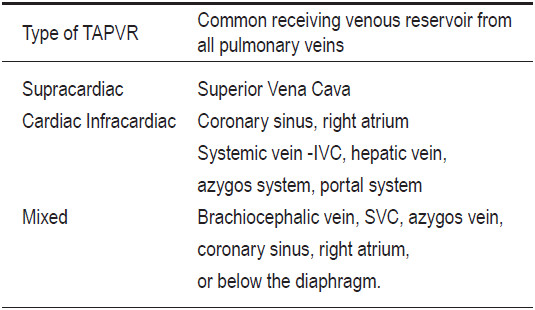
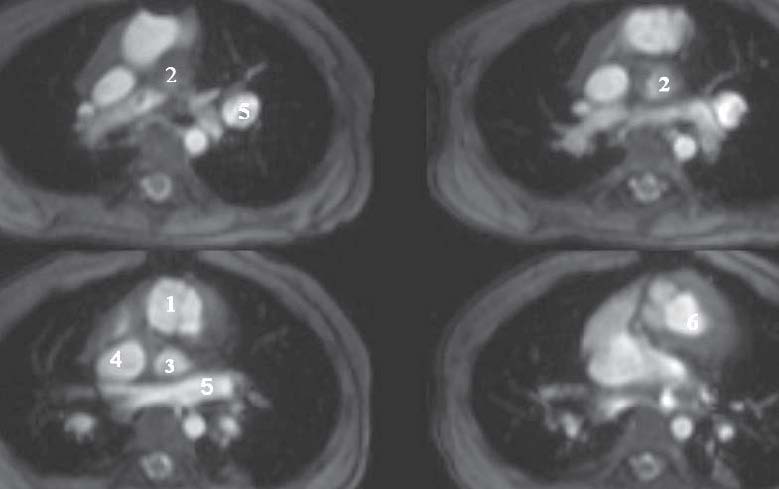
Figure 3: Sequential segmental demonstration approach step IV is applied to an MRI with a gradient echo pulse sequence in an axial view. A-D show concordant ventriculoarterial connection, with double outlet morphology. 1 = Aortic valve, 2 = Pulmonic valve, 3 = Pulmonary viens, 4 = Superior vena cava, 5 = Vertical vein (confluence of four pulmonary arteries).
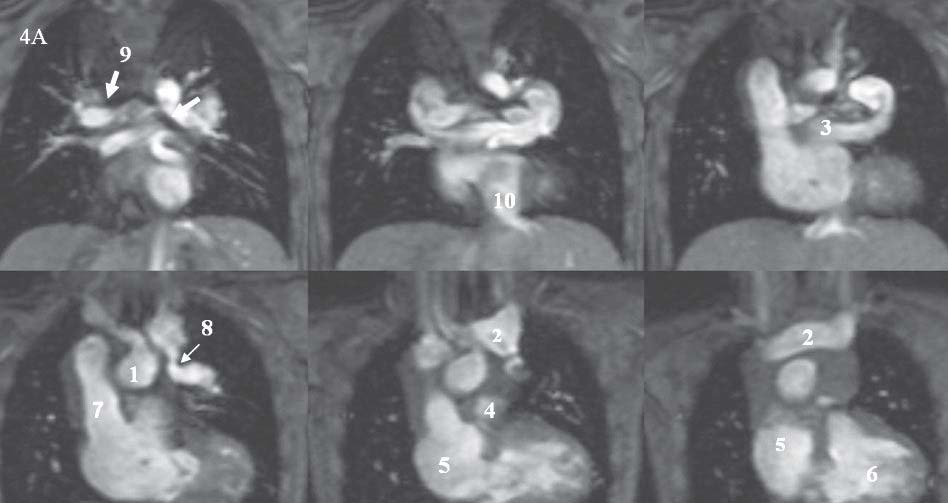
Figure 4A: Sequential segmental demonstration approach step IV is applied on a gradient echo MRI on the coronal view: 1 = Ascending aorta, 2 = Innominate vein, 3 = Vertical vein, 4 = MPA, 5 = Right atrium, 6 = Right ventricle, 7 = Right superior vena cava, 8 = Stenosis of the connection between the vertical vein and innominate vein, 9 = Bilateral right sided tracheal line (see arrow), 10 = Inferior vena cava. Chaothawee L
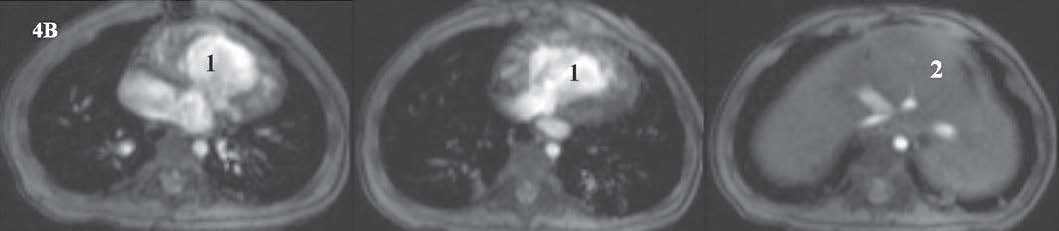
Figure 4B: Situs ambiguous with asplenia demonstrated on gradient CINE MRI images. 1= Single ventricle, 2= Liver at the mid abdomen.
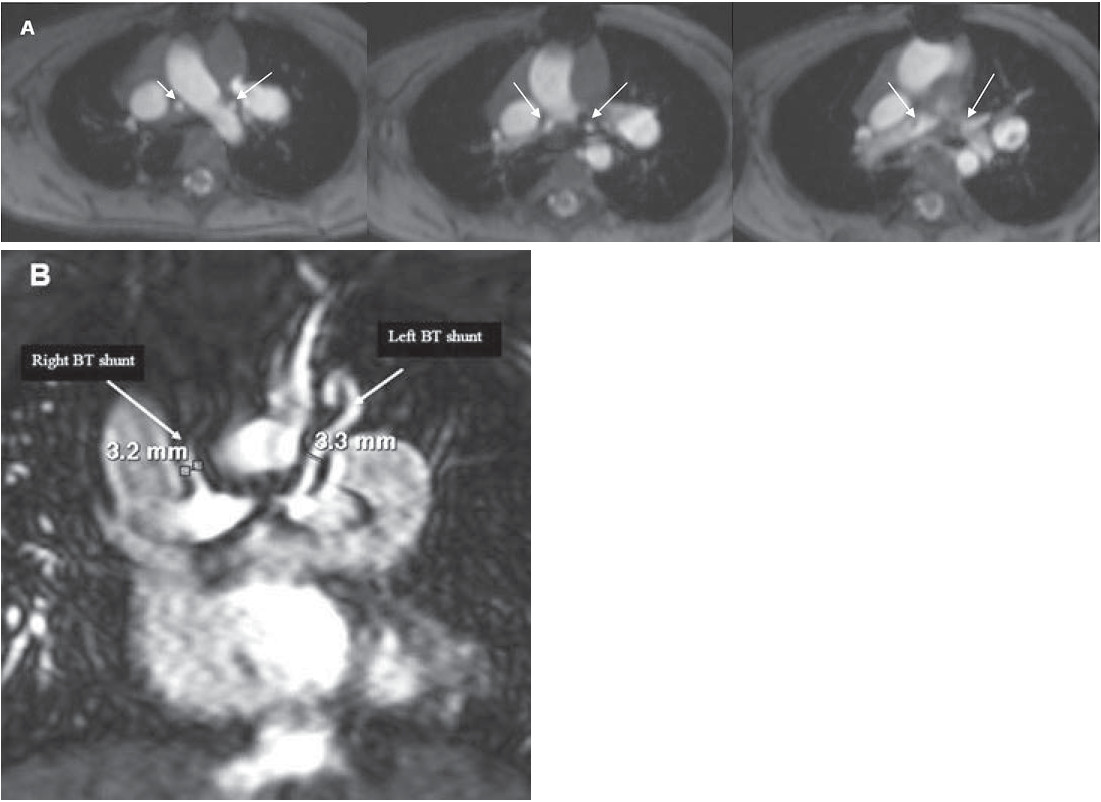
Figure 5: A = Gradient echo CINE MRI on an axial view shows the lumen of a Blalock Taussig (BT) shunt in a short axis view. B = MR angiography with a gadolinium contrast injection image on a coronal view which shows the left and right BT shunt.
The application of a sequential segmental analysis approach towards imaging is a very good method to analyze cardiac anatomy in a complex congenital heart disease case. This article has demonstrated this, by showing that the inside of the snowman sign hides a complicated story that is much more than a TAPVR. We have shown that the use of an MRI in synchronization with a sequential segmental analysis approach method is a successful approach to explore this condition. The MRI is a promising tool, given its high resolution, well tissue characterization, high reproducibility, no limited window scan, widening field of view and its many different pulse sequence techniques. This tool is well suited to be used in synchronization to a sequential segmental analysis method for cardiovascular anatomical evaluation in complex congenital heart disease.